OB/GYN Provider Manual
|
|
|
- Maryann McBride
- 10 years ago
- Views:
Transcription
1 Table of Contents Overview....1 OB/GYN Emergency coverage....1 Direct Access OB/GYN SM for HMO/POS Members....1 OB/GYN electronic Referrals....2 HMO/POS Members....2 Direct POS Members....2 PPO Members....2 OB/GYN capitation requirements for HMO/POS Members....2 Preapproval requirements....3 Women s preventive health services....4 Annual gynecological exam....4 Copayments for routine and nonroutine services....4 Requirements/restrictions by product line....4 Reimbursement above examination fees....5 Breast cancer screening....5 Cervical cancer screening....6 Osteoporosis screening....6 Assisted reproductive technologies coverage....6 HMO/POS Members....6 PPO Members....6 Maternity care....7 Prenotification of maternity care....7 Notification of fetal loss....7 Performing antepartum ultrasounds....7 OB services paid above the global fee....7 Postpartum office visits....8 Delivery out of the service area....8 Baby BluePrints maternity program....8 Register your IBC patients....8 Educational materials....9 Risk assessment....9 Pregnancy depression screening /1/2013.i
2 Antenatal/antepartum care....9 Free tobacco cessation program Postpartum programs.... Mother s Option program.... Baby BluePrints postpartum services.... Preapproval for home phototherapy /1/2013.ii
3 Overview This section provides information on benefits, policies, and procedures specific to obstetrical/ gynecological (OB/GYN) care, women s preventive health services, Baby BluePrints perinatal case management, and postpartum programs, including the Mother s Option program. Not all groups have access to all services; therefore, providers should verify Member eligibility and benefits using the NaviNet web portal or by calling the Provider Automated System at ASK-BLUE. Note: OB/GYN specialists cannot be designated as the HMO/POS Member s Primary Care Physician (PCP). OB/GYN Emergency coverage In emergent situations, Members should proceed directly to a hospital for treatment. HMO/POS Members are instructed to call their PCP (or OB/GYN Provider if pregnant) for instructions in nonemergent situations. The OB/GYN Provider may act as the referring Physician during pregnancy for pregnancy-related conditions. Be aware that Member Copayments for emergency room/department (ER) visits (emergent or nonemergent) are generally higher than office visit Copayments. Direct Access OB/GYN SM for HMO/POS Members Direct Access OB/GYN allows HMO/POS Members to receive services from any network OB/GYN specialist or subspecialist without a Referral for Preventive Care visits, routine OB/GYN care, or problem-focused OB/GYN conditions. Specialties and subspecialties not requiring Referrals include, but are not limited to, the following: OB GYN (including urogynecologist) OB/GYN gynecologic oncologist reproductive endocrinologist/infertility specialist maternal fetal medicine/perinatologist midwife reproductive health centers abortion centers mammography centers (screening and diagnostic mammograms and follow-up ultrasounds only) Although no PCP or OB/GYN Referrals are required when services are provided by network OB/GYN Providers, OB subspecialists, or certified nurse midwives (CNM), Plan and specific group restrictions may apply. Check the Member s benefits before providing the following services: abortion assisted infertility services Depo-Provera diaphragm fitting intrauterine device (IUD) insertion and removal for contraception 1/1/2013.1
4 contraceptive implant insertion and removal tubal ligation OB/GYN electronic Referrals HMO/POS Members OB/GYN Providers, CNMs, and OB/GYN specialists may send HMO/POS Members for additional services. Referrals must be sent and retrieved using NaviNet or the Provider Automated System. The OB/GYN Referral Request Form, available on NaviNet, must be used for the following services: pelvic ultrasounds, abdominal X-rays, intravenous pyelograms (IVP), and DXA scans (these tests must be performed at the Member s capitated radiology site); see OB/GYN capitation requirements for HMO/POS Members below for more information; initial consultations for HMO Members for endocrinology, general surgery, genetics, gastrointestinal, urology, pediatric cardiology, and fetal cardiovascular studies (visits beyond the initial consultation still require a PCP Referral). OB/GYN Referrals are valid for 90 days from the date of issue. Referrals are valid for eligible HMO Members. Members are responsible for payment if they are not eligible HMO Members on the date services are rendered. Direct POS Members Direct POS Members never need a Referral to receive care from participating specialists. Preapproval requirements can be found at Note: Direct POS Members should be referred to their PCP s capitated site for laboratory and radiology services. PPO Members PPO Members do not need Referrals. However, their benefits can be different from those of HMO Members. Benefits should be verified through NaviNet or the Provider Automated System before rendering care. Only certain procedures require Preapproval. Contact Customer Service for further information. OB/GYN capitation requirements for HMO/POS Members Laboratory: All routine laboratory work must be sent to the PCP s capitated laboratory site. The Member s capitated laboratory site is indicated on her Member ID card. Further information is also available on NaviNet. Note: Direct POS Members should be referred to their PCP s capitated site for laboratory and radiology services for in-network benefits. For HMO and POS referred benefits, Referrals are required. Ultrasounds: General ultrasounds for normal pregnancy and gynecology must be referred to the PCP s capitated radiology site. Nuchal translucency screening ultrasounds (first trimester screening) must be performed by ultrasound units certified for the study. Verify certification before issuing a referral. Visit the Nuchal Translucency Quality Review Program website at Participating laboratories provide the accompanying blood tests; therefore, there is no need to send Members to an out-of-network Provider for these tests. 1/1/2013.2
5 For high-risk or follow-up ultrasounds, testing, and consultations for high-risk OB patients, Members can be sent directly to a network HMO maternal fetal medicine Provider without Preapproval. Radiology: Diagnostic or screening mammograms and follow-up ultrasounds may be performed at any participating site. Sonohysterograms and hysterosalpingograms are not included in capitation and may be scheduled at any participating radiology facility. All other radiologic procedures, including DXA scans, must be performed at the PCP s capitated site. Preapproval requirements Prenotification of all maternity care must be made through our Baby BluePrints Initial Maternity Patient Questionnaire. Go to for information on obtaining this form. Preapproval of the hospital length of stay is not required. All requests for services from a nonparticipating Provider must be Preapproved for HMO Members. Referrals to a nonparticipating facility or Provider are not accepted electronically. If you determine that a nonparticipating Provider is needed for your patient, submit the request through NaviNet or call Customer Service. POS and PPO Members have the option to receive care from an out-of-network Provider but will incur a higher out-of-pocket cost. To request an exception for services to be covered at the Member s in-network level, Preapproval is required. Certain services may require Preapproval, depending on benefits coverage. Refer to preapproval for a list of services that require Preapproval. The following are some examples: procedures (office-based, outpatient, ambulatory surgical center, short procedure unit, and hospital inpatient) require preapproval, except for termination of pregnancies performed in a participating freestanding facility (surgical center, reproductive health center, office or abortion center). hospital admissions, other than maternity/surgical procedures, require preapproval. Also note the following: Except for deliveries, the admitting Physician is responsible for obtaining Preapproval at least five days prior to the scheduled admission and notifying the facility of the Preapproval number. A separate Referral to a participating hospital is not required for hospital admissions for participating OB/GYN Providers. The hospital must contact us prior to the admission to verify Member eligibility and the Preapproval number. pre-admission testing and hospital-based Physician services (e.g., anesthesia) are covered under the hospital Preapproval. Administration of Lupron for medical indications requires Preapproval.* Insertion of a Mirena IUD for medical (noncontraceptive) indications requires Preapproval.* *Preapproval is not required for these services for PPO Members. 1/1/2013.3
6 Women s preventive health services Annual gynecological exam The following services are components of a routine, preventive OB/GYN visit: breast examination; limited screening history and examination; physical exam (breast, abdomen, pelvic, and rectal); counseling regarding contraception, human sexuality and dysfunction, menopause, and sexually transmitted diseases; Pap test; pelvic examination; specimen collection and wet mount. Copayments for routine and nonroutine services When a Member visits your office for GYN services, you should collect the appropriate Copayment. To verify the correct Copayment, refer to the Member s ID card or NaviNet. In most circumstances for routine annual GYN visits, a Copayment should not be collected. However, in cases where both a routine annual screening and specific problem-focused Evaluation and Management (E&M) services are delivered during the same visit, both routine and nonroutine Copayments may apply. Bill separately for the problem-focused E&M visit only if the services you rendered beyond the preventive visit separately meet Current Procedural Terminology (CPT ) criteria for the E&M code. As required by the Patient Protection and Affordable Care Act of 2010, there is no member cost-sharing (i.e., $0 Copayment) for certain preventive services provided to Members. Claim Payment Policy # : Preventive Care Services, which includes the list of applicable preventive codes, is available on NaviNet or at Note: Documentation in the medical record must support the services billed. Requirements/restrictions by product line HMO and POS Members (Non-Flex) PCP capitated sites must be used, except for Emergencies and for mammograms. Members have coverage for all required routine and nonroutine visits. All initial services related to GYN care can be ordered directly by the OB/GYN Provider without a Referral from the PCP. HMO and POS Members (Flex Series) PCP capitated sites must be used, except for Emergencies and for mammograms. Members have coverage for an annual routine GYN exam with Pap test. Nonroutine GYN visits are covered. PPO Personal Choice Members (Flex and Non-Flex) Members may visit any specialist in the Personal Choice network without a Referral. The highest benefits level is available when in-network radiology and laboratory sites are used. 1/1/2013.4
7 Members have coverage for an annual routine GYN exam with Pap test. Some groups coverage runs on a calendar-year basis and some on a contract-year basis. Contact Customer Service for further information on your patient's coverage. Nonroutine GYN visits are covered. Medicare Advantage HMO & PPO Members Members have coverage for one routine GYN exam and Pap test annually. Reimbursement above examination fees The following procedures are eligible for separate reimbursement (if they are a covered benefit for the Member) when performed during a routine GYN exam: administration of Depo Provera endometrial biopsy office ultrasound ONLY with diagnosis of rule out ectopic pregnancy (for HMO Members only) contraceptive implant insertion and removal* diaphragm fitting* IUD insertion and removal* For more information on ultrasounds, refer to the Billing section of this manual. *This is not a standard PPO benefit. In addition, some HMO groups do not cover these procedures. Verify eligibility through NaviNet or the Provider Automated System. Breast cancer screening Mammography screening reminder program An annual reminder to schedule a yearly mammogram is sent to female managed care Members who are turning 40 as well as females ages 42 through 69 who haven t had a mammography in the last 18 months. Mammography Referral requirements All commercial and Medicare Advantage HMO Members may obtain screening and/or diagnostic mammography from an accredited in-network radiology Provider without obtaining a Referral. HMO Members must go to an in-network radiology site, but they are not restricted to their capitated site for diagnostic or screening mammograms or for ultrasound follow-up if needed. However, follow-up MRI and other radiologic imaging must be done at their capitated site, unless an out-of-capitation exception is requested and approved by IBC. Breast ultrasounds also do not require a Referral and may be performed at an in-network radiology site or outpatient department of a hospital. Note the following: Certain radiology facilities may require a Physician s written prescription. You may need to communicate this to your HMO Members asking about mammography. Be sure to provide a written prescription for the mammography study if this is a requirement of the radiology site. Proper certification, credentialing, and accreditation are required for in-network Providers to render mammography services to our Members. 1/1/2013.5
8 All MRIs require precertification through AIM Specialty Health SM (AIM). Refer to the Specialty Programs and Laboratory Services section of this manual for additional information about AIM. Breast Cancer Risk Assessment Tool Based on the Gail Model, the Breast Cancer Risk Assessment Tool is a computer program developed by the National Cancer Institute that estimates a woman s five-year and lifetime risk of developing breast cancer. The tool is available on by selecting Resources for Patient Management from the Providers drop-down menu, then Internet Resources. Women are advised to discuss their individual risk factors and options for prevention and treatment with their health care Providers. Women who are identified as high-risk may be offered chemoprophylaxis against breast cancer. Cervical cancer screening We provide coverage for standard Pap test and liquid-based Pap test technologies, such as ThinPrep and SurePath, and for other appropriate studies and procedures, including human papillomavirus (HPV) viral typing. The Member may be responsible for office visit Copayments. Be aware that a Member s health plan benefits may be based on specific time frames. For coverage questions, Members should contact Customer Service at the telephone number on their ID card. We also mail educational materials about the importance of Pap tests to our female managed care Members, ages 21 and older, for whom we have no record of a Pap test within a specified time frame. Osteoporosis screening Bone mineral density testing is covered according to Medical Policy # : Bone Mineral Density (BMD) Testing, but no more frequently than every two years, except for specific situations. Visit to view this medical policy. To learn about FRAX (World Health Organization Fracture Risk Assessment Tool), go to Assisted reproductive technologies coverage HMO/POS Members No Referral is necessary for assisted reproductive technologies (ART) services. Members may be sent by either their PCP or OB/GYN Provider, or they may schedule a visit with the specialist themselves. Most HMO/POS Member benefits contracts exclude in vitro fertilization (IVF) and related services. Verify coverage of specific procedures and pharmacy benefits through NaviNet or the Provider Automated System. All facility-based infertility procedures require Preapproval, regardless of whether they are provided by a reproductive endocrinologist or general gynecologist. PPO Members Not all Member benefits contracts include coverage for ART services. Verify coverage of specific procedures and of pharmacy benefits through NaviNet or the Provider Automated System. Infertility drug coverage: Office injectables are covered under PPO medical benefits when group coverage includes an ART coverage rider. If a rider exists, Preapproval may be required. 1/1/2013.6
9 Providers should call Customer Service for specific information about benefits coverage for infertility treatments. Maternity care First trimester prenatal care correlates well with good maternity outcomes. We urge you to schedule first visits with your pregnant IBC Members within the first trimester so that folic acid and appropriate counseling can be provided. Prenotification of maternity care IBC requires early prenotification of all maternity care, regardless of the planned delivery site hospital or birth center. Home birth requests should be submitted by the Provider using the Initial Maternity Patient Questionnaire, indicating the back-up hospital. Go to for information on obtaining this form. You can verify a Member s maternity prenotification reference number and get the inpatient routine maternity services status through NaviNet or the Provider Automated System. Notification of fetal loss In the event of an interrupted pregnancy (miscarriage or termination), notify Baby BluePrints as soon as possible so we can discontinue maternity-related educational mailings and information. Performing antepartum ultrasounds HMO Members Maternal fetal medicine specialists may perform ultrasounds in the office for patients with high-risk pregnancies. OB/GYN Providers may perform limited abdominal and transvaginal ultrasounds to rule out ectopic pregnancies. No Preapproval is required if the ultrasound is billed with the appropriate diagnosis code. For more information see the Billing section of this manual. All other ultrasounds should be performed at the capitated site of the Member s PCP. PPO Members OB and maternal fetal medicine specialists may perform ultrasounds in their offices as medically appropriate. Preapproval is not required. OB services paid above the global fee OB Providers may perform the following OB services in their offices and be paid above the global fee (or refer to in-network Providers with OB/GYN Referrals): glucose tolerance test non-stress test amniocentesis RhoGAM tubal ligation 17-alpha hydroxyprogesterone caproate with Preapproval through external cephalic version 1/1/2013.7
10 CNMs* Note: The home birth global fee includes postpartum home visits. *CNMs performing home births are eligible for a site-of-service differential. Postpartum office visits Postpartum visits should be scheduled 21 to 56 days after delivery. Adhering to this time frame provides the best opportunity to assess the physical healing of new mothers and to safely prescribe contraception, if necessary. It also meets National Committee for Quality Assurance guidelines for postpartum care. Visits should be clearly labeled postpartum care. Members should schedule postpartum visits prior to discharge from the hospital. Delivery out of the service area HMO Members. If Members do not deliver in the service area, they must call the Customer Service number on their Member ID card. Since the maternity prenotification process includes confirmation of intended delivery for an in-network provider, some services may not be fully covered if performed out-of-network. POS Members. Members have the option to deliver out-of-network and/or out of the service area, but they will be subject to Deductibles and Coinsurance. PPO Members. Members may access care outside of the service area from Providers who participate in the BlueCard PPO Program. Out-of-network services are subject to out-of-network cost-sharing (i.e., Deductible/Coinsurance). Baby BluePrints maternity program Our award-winning maternity program is designed to educate all pregnant IBC Members about pregnancy and preparing for parenthood. The program also helps to identify expectant mothers who may be at risk for complications during their pregnancy and to assist in improving the quality of care to pregnant women and newborns. If any risk factors are detected, our OB nurse case managers provide telephone support to our Members and their Physician or midwife to help coordinate their benefits and provide information they need for the healthiest delivery possible. Note: Some value-added services covered under this program are enhancements to the standard Member benefits and are therefore subject to change at any time upon notice. For more information about Baby BluePrints or to refer a Member, call or BABY (outside the 215 area). Case managers are available Monday through Friday from 8 a.m. to 5 p.m. Nurse case managers are also available after hours to assist you with urgent home care or durable medical equipment (DME) needs. Register your IBC patients Registering maternity Members into our Baby BluePrints high-risk perinatal program is imperative for early outreach. Note: The Baby BluePrints maternity program is offered only to IBC Members. Therefore, remind your staff to verify eligibility prior to giving a patient the questionnaire to complete. The Initial Maternity Patient Questionnaire should be completed by the OB Provider and the Member at the first prenatal visit and mailed immediately after to ensure timely registration into this program. These forms should not be batched and held. OB Providers should mail the form to the Baby BluePrints department immediately, using the postage-paid envelope supplied by the program. This registers the Member in the Baby BluePrints program and triggers educational mailings. 1/1/2013.8
11 Our case managers use the information as a means for identifying, tracking, and risk-stratifying all pregnant Members for care management and coordination. If you need to request additional forms, call the Provider Supply Line at Educational materials Baby BluePrints materials focus on education. Mothers-to-be will receive a packet detailing information about good self-care during pregnancy and its impact on mother and baby and about potential problems during pregnancy. Benefits information is also provided. The packet also includes offers for reimbursement for: parenting classes (e.g., childbirth preparation, lactation, sibling, exercise.), up to $50;* breast pump purchase, up to $50;* lactation consultation, $100 per pregnancy for one visit with any International Board Certified Lactation Consultant (IBCLC).* *Some of these programs are available to managed care Members only. Additionally, Members can receive exclusive discounts on the Saving Baby s Cord Blood storage program from CorCell. Members may also participate in the following: Quit&Fit tobacco cessation program (see Free tobacco cessation program on page.10); Mother s Option program (see Postpartum programs on page.). Risk assessment Members are screened for risk at the time of enrollment into Baby BluePrints using the completed enrollment forms and then are screened again at 28 weeks into their pregnancy by telephone when enrolled in case management. An OB nurse case manager is available to talk to Members, answer questions, and assist with their care throughout their pregnancy. If complications are detected, Members can expect: personalized OB nurse case management; individualized education on how to reduce risk factors; periodic assessments throughout their pregnancy; coordination of home care services as Medically Necessary and ordered by a Physician or midwife. Pregnancy depression screening Baby BluePrints has a targeted program that screens pregnant women enrolled in case management in their 28th week for risk factors associated with depression (using the Whooley Questionnaire, a twoquestion depression screening tool). Your office may receive calls regarding those Members who screen positive on the 28th week questionnaire or who are judged to be at risk during any other intervention. Case managers will assist you with triage and Referrals to the Member s behavioral health Provider or to Emergency services as required. Antenatal/antepartum care Antenatal case management programs are available for, but not limited to, the following: hyperemesis gravidarum gestational diabetes 1/1/2013.9
12 pregnancy-induced hypertension preterm labor In addition, the following antepartum services are available: skilled nursing visits, which may include: 17-alpha hydroxyprogesterone caproate injections for women who are at complete bed rest and have a history of preterm delivery; self-injection techniques for insulin, heparin, and others; home blood glucose, blood pressure, and urine monitoring; betamethasone injections (initial set only, repeat injections require Medical Director approval); nutrition consults/evaluations; social service evaluations; DME. Preapproval of antepartum home care services Call the appropriate perinatal home health agency for them to obtain Preapproval review of all antepartum home care programs/services, such as, but not limited to: hyperemesis gravidarum gestational diabetes pregnancy-induced hypertension preterm labor The perinatal agency will then obtain orders for all care to be rendered from the attending Physician/CNM. Baby BluePrints case managers are available to provide support during regular business hours, 8 a.m. to 5 p.m., Monday through Friday. Call or BABY (outside the 215 area). Free tobacco cessation program We have teamed up with American Specialty Health, an independent company, to provide a free, comprehensive tobacco cessation program called Healthyroads Quit&Fit. This program is designed to provide maximum counselor intervention and support and to enhance office-based intervention. Features of the program include: tobacco cessation manual and stress-tobacco connection CD; information for mothers-to-be describing the benefits of quitting smoking; up to four telephone sessions per month for 12 months, including kick-off, pre-quit, and general assessment sessions; a toll-free phone number for calls anytime for counselor support; lifetime access to which includes online self-guided coaching modules, tools, and trackers for monitoring progress in meeting goals related to tobacco cessation; articles and video classes on a variety of tobacco cessation topics; and an electronic message center to ask questions, receive electronic guides, and receive support from a tobacco cessation coach. Quit&Fit programs, conducted by experienced, specially trained counselors, are periodically reviewed and evaluated by an editorial board comprised of qualified health professionals. 1/1/
13 Pregnant Members can contact a Baby BluePrints case manager for more information or self-enroll by calling Healthyroads Quit&Fit at Quit&Fit is a federally registered trademark of American Specialty Health Incorporated, an independent company. Postpartum programs Mother s Option program Through this program, all Members who have an uncomplicated pregnancy and delivery have the option of choosing a shorter stay in the hospital. In order to support a smooth and safe transition home, home care visits are available according to the following guidelines: Shortened length of stay (managed care Members) Uncomplicated vaginal delivery If discharged within the first 24 hours following delivery. Two home health visits are available if desired by the Member. These visits do not require Preapproval, but they should be arranged by a hospital discharge planner with one of the Mother s Option home care Providers. The first visit should occur within 48 hours of discharge. The second visit should occur within five days of discharge. If discharged within the first 48 hours following delivery. One home health visit is available if desired by the Member. This visit does not require Preapproval, but it should be arranged by a hospital discharge planner with one of the Mother s Option home care Providers. This visit should occur within 48 hours of discharge. Uncomplicated cesarean delivery If discharged within the first 96 hours following delivery. One home health visit is available if desired by the Member. This visit does not require Preapproval, but it should be arranged by a hospital discharge planner with one of the Mother s Option home care Providers and should occur within 48 hours of discharge. Standard length of stay (managed care Members) When the standard length of stay is 48 hours (vaginal) or 96 hours (cesarean), one home health visit is available if desired by the Member/Provider. This visit does not require Preapproval, but it should be arranged by a hospital discharge planner with one of the Mother s Option home care Providers. These visits must occur within five days of discharge. If additional home health visits are Medically Necessary beyond the described Mother s Option visits, these must be Preapproved by calling the Perinatal Case Management department at or BABY (outside the 215 area). CMM/Special Care SM Members. Members who opt for less than 48-hour discharge for vaginal delivery and less than 96 hours for cesarean section are eligible for one home care visit. Prenotification for this visit must be done by calling the Perinatal Case Management department as previously noted. Baby BluePrints postpartum services Postpartum care Postpartum home skilled nursing visits beyond those provided through Mother s Option are approved when Medically Necessary. These visits must be Preapproved through Baby BluePrints and include: wound/incision checks and wound care as needed 1/1/2013.
14 bilirubin checks and home phototherapy infant assessments blood pressure checks IV antibiotics home physical therapy Lactation support programs Lactation support services include information about valuable community resources, educational websites, or certified lactation consultants. Members may self-refer to any IBCLC and receive a $100 reimbursement through Healthy Lifestyles SM. Members may submit a receipt listing the date of the visit and the consultant s IBCLC certification number within 90 days after delivery. Baby BluePrints case managers are available for initial breast feeding support by telephone. Additionally, they will be able to evaluate the need for further assistance (e.g., community resources, lactation consultant, or OB Provider). Breast pumps Breast pump reimbursement. Managed care Members who participate in Baby BluePrints and obtain a manual/mini-electric breast pump at pharmacies or baby supply stores may submit their receipt to Healthy Lifestyles for reimbursement up to $50 within 90 days after delivery. Electric breast pump rentals. Hospital-grade pumps must be Preapproved for Medical Necessity. These pumps are covered under the following circumstances and when supplied by an in-network provider: detained premature newborn; infants with feeding problems that interfere with breast feeding (e.g., cleft palate/cleft lip). Preapproval for home phototherapy Preapproval is required when ordering home phototherapy to treat jaundiced newborns. Skilled nursing visits must also be Preapproved. 1/1/
OBGYN Orientation & Billing Guide 9/22/2014
 OBGYN Orientation & Billing Guide 2014 Welcome to Magnolia Health! We thank you for being part of or considering Magnolia s network of participating providers, hospitals, and other healthcare professionals.
OBGYN Orientation & Billing Guide 2014 Welcome to Magnolia Health! We thank you for being part of or considering Magnolia s network of participating providers, hospitals, and other healthcare professionals.
Aetna Life Insurance Company
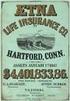 Aetna Life Insurance Company Hartford, Connecticut 06156 Amendment Policyholder: Group Policy No.: Effective Date: UNIVERSITY OF PENNSYLVANIA POSTDOCTORAL INSURANCE PLAN GP-861472 This Amendment is effective
Aetna Life Insurance Company Hartford, Connecticut 06156 Amendment Policyholder: Group Policy No.: Effective Date: UNIVERSITY OF PENNSYLVANIA POSTDOCTORAL INSURANCE PLAN GP-861472 This Amendment is effective
IN-NETWORK MEMBER PAYS. Out-of-Pocket Maximum (Includes a combination of deductible, copayments and coinsurance for health and pharmacy services)
 HMO-OA-CNT-30-45-500-500D-13 HMO Open Access Contract Year Plan Benefit Summary This is a brief summary of benefits. Refer to your Membership Agreement for complete details on benefits, conditions, limitations
HMO-OA-CNT-30-45-500-500D-13 HMO Open Access Contract Year Plan Benefit Summary This is a brief summary of benefits. Refer to your Membership Agreement for complete details on benefits, conditions, limitations
Provider Notification Obstetrical Billing
 Provider Notification Obstetrical Billing Date of Notification September 1, 20 Revision Date September 17, 2015 Plans Affected Mercy Care Plan and Mercy Care Long Term Care Plan Referrals As outlined in
Provider Notification Obstetrical Billing Date of Notification September 1, 20 Revision Date September 17, 2015 Plans Affected Mercy Care Plan and Mercy Care Long Term Care Plan Referrals As outlined in
Essentials Choice Rx 25 (HMO-POS) offered by PacificSource Medicare
 Essentials Choice Rx 25 (HMO-POS) offered by PacificSource Medicare Annual Notice of Changes for 2016 You are currently enrolled as a member of Essentials Choice Rx 25 (HMO-POS). Next year, there will
Essentials Choice Rx 25 (HMO-POS) offered by PacificSource Medicare Annual Notice of Changes for 2016 You are currently enrolled as a member of Essentials Choice Rx 25 (HMO-POS). Next year, there will
Essentials Choice Rx 24 (HMO-POS) offered by PacificSource Medicare
 Essentials Choice Rx 24 (HMO-POS) offered by PacificSource Medicare Annual Notice of Changes for 2016 You are currently enrolled as a member of Essentials Choice Rx 24 (HMO-POS). Next year, there will
Essentials Choice Rx 24 (HMO-POS) offered by PacificSource Medicare Annual Notice of Changes for 2016 You are currently enrolled as a member of Essentials Choice Rx 24 (HMO-POS). Next year, there will
Illinois Insurance Facts Illinois Department of Insurance
 Illinois Insurance Facts Illinois Department of Insurance Women s Health Care Issues Revised August 2012 Note: This information was developed to provide consumers with general information and guidance
Illinois Insurance Facts Illinois Department of Insurance Women s Health Care Issues Revised August 2012 Note: This information was developed to provide consumers with general information and guidance
California PCP Selected* Not Applicable
 PLAN FEATURES Deductible (per calendar ) Member Coinsurance * Not Applicable ** Not Applicable Copay Maximum (per calendar ) $3,000 per Individual $6,000 per Family All member copays accumulate toward
PLAN FEATURES Deductible (per calendar ) Member Coinsurance * Not Applicable ** Not Applicable Copay Maximum (per calendar ) $3,000 per Individual $6,000 per Family All member copays accumulate toward
SISC Custom SaveNet Zero Admit 10 Benefit Summary (Uniform Health Plan Benefits and Coverage Matrix)
 SISC Custom SaveNet Zero Admit 10 Benefit Summary (Uniform Health Plan Benefits and Coverage Matrix) Blue Shield of California Highlights: A description of the prescription drug coverage is provided separately
SISC Custom SaveNet Zero Admit 10 Benefit Summary (Uniform Health Plan Benefits and Coverage Matrix) Blue Shield of California Highlights: A description of the prescription drug coverage is provided separately
Greater Tompkins County Municipal Health Insurance Consortium
 WHO IS COVERED Requires both Medicare A & B enrollment. Type of Coverage Offered Single only Single only MEDICAL NECESSITY Pre-Certification Requirement None None Medical Benefit Management Program Not
WHO IS COVERED Requires both Medicare A & B enrollment. Type of Coverage Offered Single only Single only MEDICAL NECESSITY Pre-Certification Requirement None None Medical Benefit Management Program Not
PPO Hospital Care I DRAFT 18973
 This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.ibx.com or by calling 1-800-ASK-BLUE. Important Questions
This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.ibx.com or by calling 1-800-ASK-BLUE. Important Questions
Hawaii Benchmarks Benefits under the Affordable Care Act (ACA)
 Hawaii Benchmarks Benefits under the Affordable Care Act (ACA) 10/2012 Coverage for Newborn and Foster Children Coverage Outside the Provider Network Adult Routine Physical Exams Well-Baby and Well-Child
Hawaii Benchmarks Benefits under the Affordable Care Act (ACA) 10/2012 Coverage for Newborn and Foster Children Coverage Outside the Provider Network Adult Routine Physical Exams Well-Baby and Well-Child
BRYN MAWR COLLEGE MEDICAL INSURANCE BENEFITS COMPARISON EFFECTIVE NOVEMBER 1, 2009
 BENEFITS Description of Plan Annual Deductible (January - December) - Individual - Family PERSONAL CHOICE PPO BRYN MAWR COLLEGE KEYSTONE HEALTH PLAN EAST KEYSTONE POS Provides comprehensive health Provides
BENEFITS Description of Plan Annual Deductible (January - December) - Individual - Family PERSONAL CHOICE PPO BRYN MAWR COLLEGE KEYSTONE HEALTH PLAN EAST KEYSTONE POS Provides comprehensive health Provides
CIGNA HEALTH AND LIFE INSURANCE COMPANY, a Cigna company (hereinafter called Cigna)
 Home Office: Bloomfield, Connecticut Mailing Address: Hartford, Connecticut 06152 CIGNA HEALTH AND LIFE INSURANCE COMPANY, a Cigna company (hereinafter called Cigna) CERTIFICATE RIDER No CR7SI006-1 Policyholder:
Home Office: Bloomfield, Connecticut Mailing Address: Hartford, Connecticut 06152 CIGNA HEALTH AND LIFE INSURANCE COMPANY, a Cigna company (hereinafter called Cigna) CERTIFICATE RIDER No CR7SI006-1 Policyholder:
PLAN DESIGN AND BENEFITS - PA Health Network Option AHF HRA 1.3. Fund Pays Member Responsibility
 HEALTHFUND PLAN FEATURES HealthFund Amount (Per plan year. Fund changes between tiers requires a life status change qualifying event.) Fund Coinsurance (Percentage at which the Fund will reimburse) Fund
HEALTHFUND PLAN FEATURES HealthFund Amount (Per plan year. Fund changes between tiers requires a life status change qualifying event.) Fund Coinsurance (Percentage at which the Fund will reimburse) Fund
Billing Guidelines for Obstetrical Services and PCO Responsibilities
 Billing Guidelines for Obstetrical Services and PCO Responsibilities Providing obstetrical services to UnitedHealthcare Community Plan members and your patients is a collaborative effort. Complying with
Billing Guidelines for Obstetrical Services and PCO Responsibilities Providing obstetrical services to UnitedHealthcare Community Plan members and your patients is a collaborative effort. Complying with
Table of Contents Billing & Reimbursement for Hospital Services
 Table of Contents Billing & Reimbursement for Hospital Services Overview...8.1 Inpatient Services...8.1 Maternity Admissions... 8.1 Outpatient Services...8.1 Cardiology... 8.3 Diabetic education... 8.3
Table of Contents Billing & Reimbursement for Hospital Services Overview...8.1 Inpatient Services...8.1 Maternity Admissions... 8.1 Outpatient Services...8.1 Cardiology... 8.3 Diabetic education... 8.3
AVMED POS PLAN. Allergy Injections No charge 30% co-insurance after deductible Allergy Skin Testing $30 per visit 30% co-insurance after deductible
 AVMED POS PLAN This Schedule of Benefits reflects the higher provider and prescription copays for 2015. This is not a contract, it s a summary of the plan highlights and is subject to change. For specific
AVMED POS PLAN This Schedule of Benefits reflects the higher provider and prescription copays for 2015. This is not a contract, it s a summary of the plan highlights and is subject to change. For specific
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Appendix A. Prepared Exclusively for The Dow Chemical Company
 Appendix A BENEFIT PLAN Prepared Exclusively for The Dow Chemical Company What Your Plan Covers and How Benefits are Paid Choice POS II (MAP Plus Option 2 - High Deductible Health Plan (HDHP) with Prescription
Appendix A BENEFIT PLAN Prepared Exclusively for The Dow Chemical Company What Your Plan Covers and How Benefits are Paid Choice POS II (MAP Plus Option 2 - High Deductible Health Plan (HDHP) with Prescription
PLAN DESIGN AND BENEFITS POS Open Access Plan 1944
 PLAN FEATURES PARTICIPATING Deductible (per calendar year) $3,000 Individual $9,000 Family $4,000 Individual $12,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being
PLAN FEATURES PARTICIPATING Deductible (per calendar year) $3,000 Individual $9,000 Family $4,000 Individual $12,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Adobe Systems Incorporated. Aetna Choice POS II
 Adobe Systems Incorporated Aetna Choice POS II BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group Welfare
Adobe Systems Incorporated Aetna Choice POS II BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group Welfare
2015 Medical Plan Summary
 2015 Medical Plan Summary AVMED POS PLAN This Schedule of Benefits reflects the higher provider and prescription copayments for 2015. This is not a contract, it s a summary of the plan highlights and is
2015 Medical Plan Summary AVMED POS PLAN This Schedule of Benefits reflects the higher provider and prescription copayments for 2015. This is not a contract, it s a summary of the plan highlights and is
PREFERRED CARE. All covered expenses, including prescription drugs, accumulate toward both the preferred and non-preferred Payment Limit.
 PLAN FEATURES Deductible (per plan year) $300 Individual $300 Individual None Family None Family All covered expenses, excluding prescription drugs, accumulate toward both the preferred and non-preferred
PLAN FEATURES Deductible (per plan year) $300 Individual $300 Individual None Family None Family All covered expenses, excluding prescription drugs, accumulate toward both the preferred and non-preferred
Benefit Highlights for UNC Greensboro students
 bcbsnc.com/uncg Benefit Highlights for UNC Greensboro students Effective 08/01/2016 StdGrp, 4/16 U9096a, 5/16 Table of Contents This brochure is a general summary of the insurance plan offered by Blue
bcbsnc.com/uncg Benefit Highlights for UNC Greensboro students Effective 08/01/2016 StdGrp, 4/16 U9096a, 5/16 Table of Contents This brochure is a general summary of the insurance plan offered by Blue
FEATURES NETWORK OUT-OF-NETWORK
 Schedule of Benefits Employer: The Vanguard Group, Inc. ASA: 697478-A Issue Date: January 1, 2014 Effective Date: January 1, 2014 Schedule: 3B Booklet Base: 3 For: Choice POS II - 950 Option - Retirees
Schedule of Benefits Employer: The Vanguard Group, Inc. ASA: 697478-A Issue Date: January 1, 2014 Effective Date: January 1, 2014 Schedule: 3B Booklet Base: 3 For: Choice POS II - 950 Option - Retirees
PLAN DESIGN AND BENEFITS Basic HMO Copay Plan 1-10
 PLAN FEATURES Deductible (per calendar year) Member Coinsurance Not Applicable Not Applicable Out-of-Pocket Maximum $5,000 Individual (per calendar year) $10,000 Family Once the Family Out-of-Pocket Maximum
PLAN FEATURES Deductible (per calendar year) Member Coinsurance Not Applicable Not Applicable Out-of-Pocket Maximum $5,000 Individual (per calendar year) $10,000 Family Once the Family Out-of-Pocket Maximum
PLAN DESIGN AND BENEFITS Georgia 2-100 HNOption 13-1000-80
 Georgia Health Network Option (POS Open Access) PLAN DESIGN AND BENEFITS Georgia 2-100 HNOption 13-1000-80 PLAN FEATURES PARTICIPATING PROVIDERS NON-PARTICIPATING PROVIDERS Deductible (per calendar year)
Georgia Health Network Option (POS Open Access) PLAN DESIGN AND BENEFITS Georgia 2-100 HNOption 13-1000-80 PLAN FEATURES PARTICIPATING PROVIDERS NON-PARTICIPATING PROVIDERS Deductible (per calendar year)
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Adobe Systems Incorporated. Aetna HealthFund HRA Plan
 Adobe Systems Incorporated Aetna HealthFund HRA Plan BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group
Adobe Systems Incorporated Aetna HealthFund HRA Plan BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group
Western Health Advantage: City of Sacramento HSA ABHP Coverage Period: 1/1/2016-12/31/2016
 Coverage For: Self Plan Type: HMO This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.westernhealth.com or
Coverage For: Self Plan Type: HMO This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.westernhealth.com or
2015 Medical Plan Options Comparison of Benefit Coverages
 Member services 1-866-641-1689 1-866-641-1689 1-866-641-1689 1-866-641-1689 1-866-641-1689 1-800-464-4000 Web site www.anthem.com/ca/llns/ www.anthem.com/ca/llns/ www.anthem.com/ca/llns/ www.anthem.com/ca/llns/
Member services 1-866-641-1689 1-866-641-1689 1-866-641-1689 1-866-641-1689 1-866-641-1689 1-800-464-4000 Web site www.anthem.com/ca/llns/ www.anthem.com/ca/llns/ www.anthem.com/ca/llns/ www.anthem.com/ca/llns/
SMALL GROUP PLAN DESIGN AND BENEFITS OPEN CHOICE OUT-OF-STATE PPO PLAN - $1,000
 PLAN FEATURES PREFERRED CARE NON-PREFERRED CARE Deductible (per calendar year; applies to all covered services) $1,000 Individual $3,000 Family $2,000 Individual $6,000 Family Plan Coinsurance ** 80% 60%
PLAN FEATURES PREFERRED CARE NON-PREFERRED CARE Deductible (per calendar year; applies to all covered services) $1,000 Individual $3,000 Family $2,000 Individual $6,000 Family Plan Coinsurance ** 80% 60%
CSAC/EIA Health Small Group Access+ HMO 15-0 Inpatient Benefit Summary
 CSAC/EIA Health Small Group Access+ HMO 15-0 Inpatient Benefit Summary (Uniform Health Plan Benefits and Coverage Matrix) Blue Shield of California THIS MATRIX IS INTENDED TO BE USED TO HELP YOU COMPARE
CSAC/EIA Health Small Group Access+ HMO 15-0 Inpatient Benefit Summary (Uniform Health Plan Benefits and Coverage Matrix) Blue Shield of California THIS MATRIX IS INTENDED TO BE USED TO HELP YOU COMPARE
What is the overall deductible? Are there other deductibles for specific services?
 : MyPriority POS RxPlus Silver 1800 Coverage Period: Beginning on or after 01/01/2015 Summary of Benefits and Coverage: What this Plan Covers & What it Costs Coverage for: Subscriber/Dependent Plan Type:
: MyPriority POS RxPlus Silver 1800 Coverage Period: Beginning on or after 01/01/2015 Summary of Benefits and Coverage: What this Plan Covers & What it Costs Coverage for: Subscriber/Dependent Plan Type:
CENTRAL MICHIGAN UNIVERSITY - Premier Plan (PPO1) 007000285-0002 0004 Effective Date: July 1, 2015 Benefits-at-a-Glance
 CENTRAL MICHIGAN UNIVERSITY - Premier Plan (PPO1) 007000285-0002 0004 Effective Date: July 1, 2015 Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only a general overview
CENTRAL MICHIGAN UNIVERSITY - Premier Plan (PPO1) 007000285-0002 0004 Effective Date: July 1, 2015 Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only a general overview
DRAKE UNIVERSITY HEALTH PLAN
 DRAKE UNIVERSITY HEALTH PLAN Effective Date: 1/1/2015 This is a general description of coverage. It is not a statement of contract. Actual coverage is subject to terms and the conditions specified in the
DRAKE UNIVERSITY HEALTH PLAN Effective Date: 1/1/2015 This is a general description of coverage. It is not a statement of contract. Actual coverage is subject to terms and the conditions specified in the
Independent Health s Medicare Passport Advantage (PPO)
 Independent Health s Medicare Passport Advantage (PPO) (a Medicare Advantage Preferred Provider Organization Option (PPO) offered by INDEPENDENT HEALTH BENEFITS CORPORATION with a Medicare contract) Summary
Independent Health s Medicare Passport Advantage (PPO) (a Medicare Advantage Preferred Provider Organization Option (PPO) offered by INDEPENDENT HEALTH BENEFITS CORPORATION with a Medicare contract) Summary
Who Is Involved in Your Care?
 Patient Education Page 3 Pregnancy and Giving Birth Who Is Involved in Your Care? Our goal is to surround you and your family with a safe environment for the birth of your baby. We look forward to providing
Patient Education Page 3 Pregnancy and Giving Birth Who Is Involved in Your Care? Our goal is to surround you and your family with a safe environment for the birth of your baby. We look forward to providing
S c h o o l s I n s u r a n c e G r o u p Health Net Plan Comparison Fiscal Year 7/1/15-6/30/16
 S c h o o l s I n s u r a n c e G r o u p Health Net Plan Comparison Fiscal Year 7/1/15-6/30/16 This information sheet is for reference only. Please refer to Evidence of Coverage requirements, limitations
S c h o o l s I n s u r a n c e G r o u p Health Net Plan Comparison Fiscal Year 7/1/15-6/30/16 This information sheet is for reference only. Please refer to Evidence of Coverage requirements, limitations
PLAN DESIGN AND BENEFITS AETNA LIFE INSURANCE COMPANY - Insured
 PLAN FEATURES Deductible (per calendar year) Individual $750 Individual $1,500 Family $2,250 Family $4,500 All covered expenses accumulate simultaneously toward both the preferred and non-preferred Deductible.
PLAN FEATURES Deductible (per calendar year) Individual $750 Individual $1,500 Family $2,250 Family $4,500 All covered expenses accumulate simultaneously toward both the preferred and non-preferred Deductible.
PPO Schedule of Payments (Maryland Large Group) Qualified High Deductible Health Plan National QA2000-20
 PPO Schedule of Payments (Maryland Large Group) Qualified High Health Plan National QA2000-20 Benefit Year Individual Family (Amounts for Participating and s services are separated in calculating when
PPO Schedule of Payments (Maryland Large Group) Qualified High Health Plan National QA2000-20 Benefit Year Individual Family (Amounts for Participating and s services are separated in calculating when
HEALTH SAVINGS PPO PLAN (WITH HSA) - COLUMBUS PROVIDED BY AETNA LIFE INSURANCE COMPANY EFFECTIVE JANUARY 1, 2016 AETNA INC.
 HEALTH SAVINGS PPO PLAN (WITH HSA) - COLUMBUS PROVIDED BY AETNA LIFE INSURANCE COMPANY EFFECTIVE JANUARY 1, 2016 AETNA INC. CPOS II DEDUCTIBLE, COPAYS/COINSURANCE AND DOLLAR MAXIMUMS and Aligned Deductible
HEALTH SAVINGS PPO PLAN (WITH HSA) - COLUMBUS PROVIDED BY AETNA LIFE INSURANCE COMPANY EFFECTIVE JANUARY 1, 2016 AETNA INC. CPOS II DEDUCTIBLE, COPAYS/COINSURANCE AND DOLLAR MAXIMUMS and Aligned Deductible
Medical Plan - Healthfund
 18 Medical Plan - Healthfund Oklahoma City Community College Effective Date: 07-01-2010 Aetna HealthFund Open Choice (PPO) - Oklahoma PLAN DESIGN AND BENEFITS PROVIDED BY AETNA LIFE INSURANCE COMPANY -
18 Medical Plan - Healthfund Oklahoma City Community College Effective Date: 07-01-2010 Aetna HealthFund Open Choice (PPO) - Oklahoma PLAN DESIGN AND BENEFITS PROVIDED BY AETNA LIFE INSURANCE COMPANY -
PLAN DESIGN AND BENEFITS - Tx OAMC Basic 2500-10 PREFERRED CARE
 PLAN FEATURES Deductible (per calendar year) $2,500 Individual $4,000 Individual $7,500 Family $12,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
PLAN FEATURES Deductible (per calendar year) $2,500 Individual $4,000 Individual $7,500 Family $12,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
UC Care Plan. Benefit Booklet. University of California. Group Number: W0051612 Plan ID: PPOX0001 Effective Date: January 1, 2016
 UC Care Plan Benefit Booklet University of California Group Number: W0051612 Plan ID: PPOX0001 Effective Date: January 1, 2016 An independent member of the Blue Shield Association Claims Administered by
UC Care Plan Benefit Booklet University of California Group Number: W0051612 Plan ID: PPOX0001 Effective Date: January 1, 2016 An independent member of the Blue Shield Association Claims Administered by
$0 See the chart starting on page 2 for your costs for services this plan covers. Are there other deductibles for specific
 This is only a summary. If you want more detail about your medical coverage and costs, you can get the complete terms in the policy or plan document at www.teamsters-hma.com or by calling 1-866-331-5913.
This is only a summary. If you want more detail about your medical coverage and costs, you can get the complete terms in the policy or plan document at www.teamsters-hma.com or by calling 1-866-331-5913.
SUMMARY OF BENEFITS. Cigna Health and Life Insurance Co. Laramie County School District 2 Open Access Plus Base - Effective 7/1/2015
 SUMMARY OF BENEFITS Cigna Health and Life Insurance Co. Laramie County School District 2 Open Access Plus Base - Effective General Services In-Network Out-of-Network Physician office visit Urgent care
SUMMARY OF BENEFITS Cigna Health and Life Insurance Co. Laramie County School District 2 Open Access Plus Base - Effective General Services In-Network Out-of-Network Physician office visit Urgent care
1 exam every 12 months for members age 22 to age 65; 1 exam every 12 months for adults age 65 and older. Routine Well Child
 PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $1,000 Individual $1,000 Individual $2,000 Family $2,000 Family All covered expenses accumulate separately toward the preferred or
PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $1,000 Individual $1,000 Individual $2,000 Family $2,000 Family All covered expenses accumulate separately toward the preferred or
Important Questions Answers Why this Matters:
 This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.maineoptions.org or by calling 1-855-624-6463. Important
This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.maineoptions.org or by calling 1-855-624-6463. Important
National PPO 1000. PPO Schedule of Payments (Maryland Small Group)
 PPO Schedule of Payments (Maryland Small Group) National PPO 1000 The benefits outlined in this Schedule are in addition to the benefits offered under Coventry Health & Life Insurance Company Small Employer
PPO Schedule of Payments (Maryland Small Group) National PPO 1000 The benefits outlined in this Schedule are in addition to the benefits offered under Coventry Health & Life Insurance Company Small Employer
SUMMARY OF BENEFITS. Cigna Health and Life Insurance Co. Grand County Open Access Plus Effective 1/1/2015
 SUMMARY OF BENEFITS Cigna Health and Life Insurance Co. Grand County Open Access Plus Effective General Services In-Network Out-of-Network Primary care physician You pay $25 copay per visit Physician office
SUMMARY OF BENEFITS Cigna Health and Life Insurance Co. Grand County Open Access Plus Effective General Services In-Network Out-of-Network Primary care physician You pay $25 copay per visit Physician office
UnitedHealthcare Choice Plus. UnitedHealthcare Insurance Company. Certificate of Coverage
 UnitedHealthcare Choice Plus UnitedHealthcare Insurance Company Certificate of Coverage For the Health Savings Account (HSA) Plan 7PD of Educators Benefit Services, Inc. Enrolling Group Number: 717578
UnitedHealthcare Choice Plus UnitedHealthcare Insurance Company Certificate of Coverage For the Health Savings Account (HSA) Plan 7PD of Educators Benefit Services, Inc. Enrolling Group Number: 717578
UnitedHealthcare Choice Plus. UnitedHealthcare Insurance Company. Certificate of Coverage
 UnitedHealthcare Choice Plus UnitedHealthcare Insurance Company Certificate of Coverage For the Plan 7EG of Educators Benefit Services, Inc. Enrolling Group Number: 717578 Effective Date: January 1, 2012
UnitedHealthcare Choice Plus UnitedHealthcare Insurance Company Certificate of Coverage For the Plan 7EG of Educators Benefit Services, Inc. Enrolling Group Number: 717578 Effective Date: January 1, 2012
Important Questions Answers Why this Matters:
 This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.studentplanscenter.com or by calling 1-800-756-3702.
This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.studentplanscenter.com or by calling 1-800-756-3702.
California Small Group MC Aetna Life Insurance Company
 PLAN FEATURES Deductible (per calendar year) $1,000 per member $1,000 per member Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered expenses accumulate
PLAN FEATURES Deductible (per calendar year) $1,000 per member $1,000 per member Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered expenses accumulate
PLAN DESIGN AND BENEFITS - Tx OAMC 1500-10 PREFERRED CARE
 PLAN FEATURES Deductible (per calendar year) $1,500 Individual $3,000 Individual $4,500 Family $9,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
PLAN FEATURES Deductible (per calendar year) $1,500 Individual $3,000 Individual $4,500 Family $9,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
PLAN DESIGN & BENEFITS - CONCENTRIC MODEL
 PLAN FEATURES Deductible (per calendar year) Rice University None Family Member Coinsurance Applies to all expenses unless otherwise stated. Payment Limit (per calendar year) $1,500 Individual $3,000 Family
PLAN FEATURES Deductible (per calendar year) Rice University None Family Member Coinsurance Applies to all expenses unless otherwise stated. Payment Limit (per calendar year) $1,500 Individual $3,000 Family
STANDARD AND SELECT NETWORK PRODUCTS FROM TUFTS HEALTH PLAN
 STANDARD AND SELECT NETWORK PRODUCTS FROM TUFTS HEALTH PLAN 2015 PLAN OPTIONS Standard Network: The Standard Network plans provide members with a choice of more than 25,000 participating doctors and 90
STANDARD AND SELECT NETWORK PRODUCTS FROM TUFTS HEALTH PLAN 2015 PLAN OPTIONS Standard Network: The Standard Network plans provide members with a choice of more than 25,000 participating doctors and 90
Summary of Services and Cost Shares
 Summary of Services and Cost Shares This summary does not describe benefits. For the description of a benefit, including any limitations or exclusions, please refer to the identical heading in the Benefits
Summary of Services and Cost Shares This summary does not describe benefits. For the description of a benefit, including any limitations or exclusions, please refer to the identical heading in the Benefits
$6,350 Individual $12,700 Individual
 PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible $5,000 Individual $10,000 Individual $10,000 Family $20,000 Family All covered expenses accumulate separately toward the preferred or non-preferred Deductible.
PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible $5,000 Individual $10,000 Individual $10,000 Family $20,000 Family All covered expenses accumulate separately toward the preferred or non-preferred Deductible.
20% 40% Individual Family
 PLAN FEATURES NON-* Deductible (per calendar year) $2,500 Individual $3,000 Individual $5,000 Family $6,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
PLAN FEATURES NON-* Deductible (per calendar year) $2,500 Individual $3,000 Individual $5,000 Family $6,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
Important Questions Answers Why this Matters: What is the overall deductible? Are there other deductibles for specific services?
 : VIVA HEALTH Access Plan Coverage Period: 01/01/2015 12/31/2015 This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document
: VIVA HEALTH Access Plan Coverage Period: 01/01/2015 12/31/2015 This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document
PREVENTIVE CARE See the REHP Benefits Handbook for a list of preventive benefits* MATERNITY SERVICES Office visits Covered in full including first
 Network Providers Non Network Providers** DEDUCTIBLE (Per Calendar Year) None $250 per person $500 per family OUT-OF-POCKET MAXIMUM (When the out-of-pocket maximum is reached, benefits are paid at 100%
Network Providers Non Network Providers** DEDUCTIBLE (Per Calendar Year) None $250 per person $500 per family OUT-OF-POCKET MAXIMUM (When the out-of-pocket maximum is reached, benefits are paid at 100%
What is the overall deductible? Are there other deductibles for specific services? Is there an out-ofpocket
 Regence BlueCross BlueShield of Oregon: Preferred Coverage Period: 08/15/2015-08/14/2016 Summary of Benefits and Coverage: What this Plan Covers & What it Costs Coverage for: Individual & Eligible Family
Regence BlueCross BlueShield of Oregon: Preferred Coverage Period: 08/15/2015-08/14/2016 Summary of Benefits and Coverage: What this Plan Covers & What it Costs Coverage for: Individual & Eligible Family
Business Life Insurance - Health & Medical Billing Requirements
 PLAN FEATURES Deductible (per plan year) $2,000 Employee $2,000 Employee $3,000 Employee + Spouse $3,000 Employee + Spouse $3,000 Employee + Child(ren) $3,000 Employee + Child(ren) $4,000 Family $4,000
PLAN FEATURES Deductible (per plan year) $2,000 Employee $2,000 Employee $3,000 Employee + Spouse $3,000 Employee + Spouse $3,000 Employee + Child(ren) $3,000 Employee + Child(ren) $4,000 Family $4,000
SUMMARY OF BENEFITS. Out-of-Network Care: $10,000 per policy year
 OUTPATIENT BENEFITS Most Primary Care office visits at SHC are provided at no charge. This is not an insured benefit but is provided by NYU to all matriculated students including students who waive the
OUTPATIENT BENEFITS Most Primary Care office visits at SHC are provided at no charge. This is not an insured benefit but is provided by NYU to all matriculated students including students who waive the
Health Insurance Matrix 01/01/16-12/31/16
 Employee Contributions Family Monthly : $121.20 Bi-Weekly : $60.60 Monthly : $290.53 Bi-Weekly : $145.26 Monthly : $431.53 Bi-Weekly : $215.76 Monthly : $743.77 Bi-Weekly : $371.88 Employee Contributions
Employee Contributions Family Monthly : $121.20 Bi-Weekly : $60.60 Monthly : $290.53 Bi-Weekly : $145.26 Monthly : $431.53 Bi-Weekly : $215.76 Monthly : $743.77 Bi-Weekly : $371.88 Employee Contributions
S c h o o l s I n s u r a n c e G r o u p Health Net Plan Comparison Fiscal Year 7/1/14-6/30/15
 S c h o o l s I n s u r a n c e G r o u p Health Net Plan Comparison Fiscal Year 7/1/14-6/30/15 This information sheet is for reference only. Please refer to Evidence of Coverage requirements, limitations
S c h o o l s I n s u r a n c e G r o u p Health Net Plan Comparison Fiscal Year 7/1/14-6/30/15 This information sheet is for reference only. Please refer to Evidence of Coverage requirements, limitations
SERVICES IN-NETWORK COVERAGE OUT-OF-NETWORK COVERAGE
 COVENTRY HEALTH AND LIFE INSURANCE COMPANY 3838 N. Causeway Blvd. Suite 3350 Metairie, LA 70002 1-800-341-6613 SCHEDULE OF BENEFITS BENEFITS AND PRIOR AUTHORIZATION REQUIREMENTS ARE SET FORTH IN ARTICLES
COVENTRY HEALTH AND LIFE INSURANCE COMPANY 3838 N. Causeway Blvd. Suite 3350 Metairie, LA 70002 1-800-341-6613 SCHEDULE OF BENEFITS BENEFITS AND PRIOR AUTHORIZATION REQUIREMENTS ARE SET FORTH IN ARTICLES
Cost Sharing Definitions
 SU Pro ( and ) Annual Deductible 1 Coinsurance Cost Sharing Definitions $200 per individual with a maximum of $400 for a family 5% of allowable amount for inpatient hospitalization - or - 50% of allowable
SU Pro ( and ) Annual Deductible 1 Coinsurance Cost Sharing Definitions $200 per individual with a maximum of $400 for a family 5% of allowable amount for inpatient hospitalization - or - 50% of allowable
Blue Care Elect Preferred 90 Copay Coverage Period: on or after 09/01/2015
 Blue Care Elect Preferred 90 Copay Coverage Period: on or after 09/01/2015 Summary of Benefits and Coverage: What this Plan Covers & What it Costs Coverage for: Individual Only Plan Type: PPO This is only
Blue Care Elect Preferred 90 Copay Coverage Period: on or after 09/01/2015 Summary of Benefits and Coverage: What this Plan Covers & What it Costs Coverage for: Individual Only Plan Type: PPO This is only
IL Small Group PPO Aetna Life Insurance Company Plan Effective Date: 04/01/2009 PLAN DESIGN AND BENEFITS- PPO HSA HDHP $2,500 100/80 (04/09)
 PLAN FEATURES OUT-OF- Deductible (per calendar ) $2,500 Individual $5,000 Individual $5,000 Family $10,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
PLAN FEATURES OUT-OF- Deductible (per calendar ) $2,500 Individual $5,000 Individual $5,000 Family $10,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
North Carolina Medicaid Special Bulletin
 North Carolina Medicaid Special Bulletin An Information Service of the Division of Medical Assistance Visit DMA on the web at http://www.ncdhhs.gov/dma Number 1 (Revised 8/23/11) July 2011 Pregnancy Medical
North Carolina Medicaid Special Bulletin An Information Service of the Division of Medical Assistance Visit DMA on the web at http://www.ncdhhs.gov/dma Number 1 (Revised 8/23/11) July 2011 Pregnancy Medical
St. John s University Medical Select Plan Freedom Network SJ00301 Summary Plan Description
 St. John s University Medical Select Plan Freedom Network SJ00301 Summary Plan Description January 1, 2015 Important Information Reconstructive Breast Surgery Law Effective October 21, 1998, group and
St. John s University Medical Select Plan Freedom Network SJ00301 Summary Plan Description January 1, 2015 Important Information Reconstructive Breast Surgery Law Effective October 21, 1998, group and
NATIONWIDE INSURANCE $20-40 / 250A NATIONAL MANAGED CARE SCHEDULE OF BENEFITS
 WASHINGTON NATIONWIDE INSURANCE $20-40 / 250A NATIONAL MANAGED CARE SCHEDULE OF BENEFITS General Features Calendar Year Deductible Lifetime Benefit Maximum (Does not apply to Chemical Dependency) ($5,000.00
WASHINGTON NATIONWIDE INSURANCE $20-40 / 250A NATIONAL MANAGED CARE SCHEDULE OF BENEFITS General Features Calendar Year Deductible Lifetime Benefit Maximum (Does not apply to Chemical Dependency) ($5,000.00
Boston College Student Blue PPO Plan Coverage Period: 2015-2016
 Boston College Student Blue PPO Plan Coverage Period: 2015-2016 Summary of Benefits and Coverage: What this Plan Covers & What it Costs Coverage for: Individual and Family Plan Type: PPO This is only a
Boston College Student Blue PPO Plan Coverage Period: 2015-2016 Summary of Benefits and Coverage: What this Plan Covers & What it Costs Coverage for: Individual and Family Plan Type: PPO This is only a
PLAN DESIGN AND BENEFITS PROVIDED BY AETNA HEALTH INC
 PLAN FEATURES Deductible (per calendar year) $0 Deductible Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Deductible is NOT applicable to Hearing Aid Reimbursement,
PLAN FEATURES Deductible (per calendar year) $0 Deductible Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Deductible is NOT applicable to Hearing Aid Reimbursement,
Blue Care Elect Saver with Coinsurance Northeastern University HDHP Coverage Period: on or after 01/01/2016
 Blue Care Elect Saver with Coinsurance Northeastern University HDHP Coverage Period: on or after 01/01/2016 Summary of Benefits and Coverage: What this Plan Covers & What it Costs Coverage for: Individual
Blue Care Elect Saver with Coinsurance Northeastern University HDHP Coverage Period: on or after 01/01/2016 Summary of Benefits and Coverage: What this Plan Covers & What it Costs Coverage for: Individual
PARTICIPATING PROVIDERS / REFERRED Deductible (per calendar year)
 Your HMO Plan Primary Care Physician - You choose a Primary Care Physician. The Aetna HMO Deductible provider network gives you access to a wide selection of Primary Care Physicians ( PCP's) and Specialists
Your HMO Plan Primary Care Physician - You choose a Primary Care Physician. The Aetna HMO Deductible provider network gives you access to a wide selection of Primary Care Physicians ( PCP's) and Specialists
GIC Medicare Enrolled Retirees
 GIC Medicare Enrolled Retirees HMO Summary of Benefits Chart This chart provides a summary of key services offered by your HNE plan. Consult your Member Handbook for a full description of your plan s benefits
GIC Medicare Enrolled Retirees HMO Summary of Benefits Chart This chart provides a summary of key services offered by your HNE plan. Consult your Member Handbook for a full description of your plan s benefits
Important Questions Answers Why this Matters:
 This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.pplusic.com or by calling 608-282-8900 (1-800-545-5015).
This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.pplusic.com or by calling 608-282-8900 (1-800-545-5015).
No Charge (Except as described under "Rehabilitation Benefits" and "Speech Therapy Benefits")
 An Independent Licensee of the Blue Shield Association Custom Access+ HMO Plan Certificated & Management Benefit Summary (For groups of 300 and above) (Uniform Health Plan Benefits and Coverage Matrix)
An Independent Licensee of the Blue Shield Association Custom Access+ HMO Plan Certificated & Management Benefit Summary (For groups of 300 and above) (Uniform Health Plan Benefits and Coverage Matrix)
UNMH Certified Nurse-Midwife (CNM) Clinical Privileges
 All new applicants must meet the following requirements as approved by the UNMH Board of Trustees effective: 03/27/2015 INSTRUCTIONS Applicant: Check off the "Requested" box for each privilege requested.
All new applicants must meet the following requirements as approved by the UNMH Board of Trustees effective: 03/27/2015 INSTRUCTIONS Applicant: Check off the "Requested" box for each privilege requested.
Land of Lincoln Health : Family Health Network LLH 3-Tier Bronze PPO Coverage Period: 01/01/2016 12/31/2016
 This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.landoflincolnhealth.org or by calling 1-844-FHN-4YOU.
This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.landoflincolnhealth.org or by calling 1-844-FHN-4YOU.
