What Your Plan Covers and How Benefits are Paid BENEFIT PLAN. Prepared Exclusively for SAMPLE. Open Access Aetna Select
|
|
|
- Miranda Lambert
- 7 years ago
- Views:
Transcription
1 BENEFIT PLAN Prepared Exclusively for SAMPLE What Your Plan Covers and How Benefits are Paid Open Access Aetna Select
2 Table of Contents Schedule of Benefits... 1 Preface...20 Coverage for You and Your Dependents...20 Health Expense Coverage...20 Treatment Outcomes of Covered Services When Your Coverage Begins...21 Who Is Eligible...21 Employees Determining if You Are in an Eligible Class Obtaining Coverage for Dependents How and When to Enroll...22 Initial Enrollment in the Plan Late Enrollment Annual Enrollment Special Enrollment Periods When Your Coverage Begins...25 Your Effective Date of Coverage Your Dependent s Effective Date of Coverage How Your Medical Plan Works...26 Common Terms...26 About Your Aetna Select Medical Plan...26 How Your Aetna Select Medical Plan Works...27 Emergency and Urgent Care...28 In Case of a Medical Emergency Coverage for Emergency Medical Conditions In Case of an Urgent Condition Coverage for an Urgent Condition Non-Urgent Care Follow-Up Care After Treatment of an Emergency or Urgent Medical Condition Requirements For Coverage...31 What The Plan Covers...32 Aetna Select Medical Plan...32 Preventive Care...32 Routine Physical Exams Preventive Care Immunizations Well Woman Preventive Visits Routine Cancer Screenings Screening and Counseling Services Comprehensive Lactation Support and Counseling Services Family Planning Services - Female Contraceptives Family Planning Services - Other Vision Care Services Limitations Physician Services...38 Physician Visits Surgery Anesthetics Alternatives to Physician Office Visits Hospital Expenses...38 Room and Board Other Hospital Services and Supplies Outpatient Hospital Expenses Coverage for Emergency Medical Conditions Coverage for Urgent Conditions Alternatives to Hospital Stays Outpatient Surgery and Physician Surgical Services Birthing Center Home Health Care Skilled Nursing Care Skilled Nursing Facility Hospice Care Other Covered Health Care Expenses Acupuncture Ambulance Service Ground Ambulance Air or Water Ambulance Diagnostic and Preoperative Testing Diagnostic Complex Imaging Expenses Outpatient Diagnostic Lab Work and Radiological Services Outpatient Preoperative Testing Durable Medical and Surgical Equipment (DME) Experimental or Investigational Treatment Pregnancy Related Expenses Prosthetic Devices Short-Term Rehabilitation Therapy Services Cardiac and Pulmonary Rehabilitation Benefits. Outpatient Cognitive Therapy, Physical Therapy, Occupational Therapy and Speech Therapy Rehabilitation Benefits. Reconstructive or Cosmetic Surgery and Supplies Reconstructive Breast Surgery Specialized Care Chemotherapy Radiation Therapy Benefits Outpatient Infusion Therapy Benefits Specialty Care Prescription Drugs Treatment of Infertility Basic Infertility Expenses Spinal Manipulation Treatment Transplant Services Network of Transplant Specialist Facilities Treatment of Mental Disorders and Substance Abuse Oral and Maxillofacial Treatment (Mouth, Jaws and Teeth)... 56
3 Medical Plan Exclusions...58 Your Pharmacy Benefit...66 How the Pharmacy Plan Works...66 Getting Started: Common Terms...66 Accessing Pharmacies and Benefits...67 Accessing Network Pharmacies and Benefits Emergency Prescriptions Availability of Providers Cost Sharing for Network Benefits Pharmacy Benefit...68 Retail Pharmacy Benefits Mail Order Pharmacy Benefits Network Benefits for Specialty Care Drugs Other Covered Expenses Pharmacy Benefit Limitations Pharmacy Benefit Exclusions When Coverage Ends...76 When Coverage Ends For Employees Your Proof of Prior Medical Coverage When Coverage Ends for Dependents Continuation of Coverage...77 Continuing Health Care Benefits Continuing Coverage for Dependent Students on Medical Leave of Absence Handicapped Dependent Children Extension of Benefits...78 Coverage for Health Benefits COBRA Continuation of Coverage...78 Continuing Coverage through COBRA Who Qualifies for COBRA Disability May Increase Maximum Continuation to 29 Months Determining Your Contributions For Continuation Coverage When You Acquire a Dependent During a Continuation Period When Your COBRA Continuation Coverage Ends *Defines the Terms Shown in Bold Type in the Text of This Document. Coordination of Benefits - What Happens When There is More Than One Health Plan When Coordination of Benefits Applies Getting Started - Important Terms Which Plan Pays First How Coordination of Benefits Works Right To Receive And Release Needed Information Facility of Payment Right of Recovery When You Have Medicare Coverage Effect of Medicare General Provisions Type of Coverage Physical Examinations Legal Action Additional Provisions Assignments Misstatements Rescission of Coverage Subrogation and Right of Recovery Provision Workers Compensation Recovery of Overpayments Health Coverage Reporting of Claims Payment of Benefits Records of Expenses Contacting Aetna Effect of Benefits Under Other Plans Effect of An Health Maintenance Organization Plan (HMO Plan) On Coverage Discount Programs Discount Arrangements Incentives Claims, Appeals and External Review Glossary *... 98
4 Schedule of Benefits Employer: SAMPLE ASA: Issue Date: 00/00/00 Effective Date: 00/00/00 Schedule: 5A Booklet Base: 5 For: Open Access Aetna Select This is an ERISA plan, and you have certain rights under this plan. Please contact your Employer for additional information. Aetna Select Medical Plan PLAN FEATURES NETWORK OUT-OF-NETWORK Calendar Year Deductible* Individual Deductible* $250 Not applicable Family Deductible* $750 Not applicable Per Admission Copayment/Deductible $200 per admission Not applicable *Unless otherwise indicated, any applicable deductible must be met before benefits are paid. Plan Maximum Out of Pocket Limit includes plan deductible and copayments. Plan Maximum Out of Pocket Limit excludes precertification penalties. Individual Maximum Out of Pocket Limit: For network expenses: $1,000 Family Maximum Out of Pocket Limit: For network expenses: $3,000 Lifetime Maximum Benefit per person Unlimited Not applicable 1
5 Payment Percentage listed in the Schedule below reflects the Plan Payment Percentage. This is the amount the Plan pays. You are responsible to pay any deductibles and the remaining payment percentage. You are responsible for full payment of any non-covered expenses you incur. All Covered Expenses Are Subject To The Calendar Year Deductible Unless Otherwise Noted In The Schedule Below. Maximums for specific covered expenses, including visit, day and dollar maximums are combined maximums between network and out-of-network, unless specifically stated otherwise. PLAN FEATURES NETWORK OUT OF NETWORK Preventive Care Benefits Routine Physical Exams Office Visits - 100% per visit. Not Covered No copay or deductible applies. Covered Persons through age 21: Maximum Age & Visit Limits per 12 consecutive months Subject to any age and visit limits provided for in the comprehensive guidelines supported by the American Academy of Pediatrics/Bright Futures Guidelines for Children and Adolescents. For details, contact your physician or Member Services by logging onto the Aetna website or calling the number on the back of your ID card. Not Covered Covered Persons ages 22 but less than 65: Maximum Visits per 24 consecutive months Covered Persons age 65 and over: Maximum Visits per 12 consecutive months 1 visit Not Covered 1 visit Not Covered. Preventive Care Immunizations Performed in a facility or physician's office 100% per visit. No copay or deductible applies. Subject to any age and visit limits provided for in the comprehensive guidelines supported by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention. For details, contact your physician or Member Services by logging onto the Aetna website or calling the number on the back of your ID card. Not Covered 2
6 Screening & Counseling Services-Obesity, Misuse of Alcohol and/or Drugs & Use of Tobacco Products Office Visits Obesity and/or Healthy Diet Misuse of Alcohol and/or Drugs & Use of Tobacco Products Sexually Transmitted Infections Genetic Risk for Breast and Ovarian Cancer 100% per visit. No copay or deductible applies. Not Covered Obesity and/or Healthy Diet Maximum Visits per 12 consecutive months (This maximum applies only to Covered Persons ages 22 & older.) 26 visits (however, of these only 10 visits will be allowed under the Plan for healthy diet counseling provided in connection with Hyperlipidemia (high cholesterol) and other known risk factors for cardiovascular and diet-related chronic disease)* Not Covered. *Note: In figuring the Maximum Visits, each session of up to 60 minutes is equal to one visit. Misuse of Alcohol and/or Drugs Maximum Visits per 12 consecutive months 5 visits* Not Covered. *Note: In figuring the Maximum Visits, each session of up to 60 minutes is equal to one visit. Use of Tobacco Products Maximum Visits per 12 consecutive months 8 visits* Not Covered. *Note: In figuring the Maximum Visits, each session of up to 60 minutes is equal to one visit. Sexually Transmitted Infections Benefit Maximums Maximum Visits per 12 consecutive months 2 visits* Not Covered *Note: In figuring the Maximum Visits, each session of up to 30 minutes is equal to one visit. 3
7 Well Woman Preventive Visits Office Visits Subject to any age limits provided for in the comprehensive guidelines supported by the Health and Human Resources Administrations 100% No Calendar Year deductible applies Not Covered Maximum Visits per Calendar Year 1 visit Not Covered Routine Cancer Screening Outpatient 100% per visit No Calendar Year deductible applies. Not Covered Maximums Subject to any age; family history and frequency guidelines as set forth in the most current: evidence-based items that have in effect a rating of A or B in the current recommendations of the United States Preventive Services Task Force; and the comprehensive guidelines supported by the Health Resources and Services Administration. For details, contact your physician or Member Services by logging onto the Aetna website or calling the number on the back of your ID card. Not Covered For details, contact your physician or Member Services by logging onto the Aetna website or calling the number on the back of your ID card. Lung Cancer Screening Maximum One screening every 12 months* Not Covered *Important Note: Lung cancer screenings in excess of the maximum as shown above are covered under the Outpatient Diagnostic and Preoperative Testing section of your Schedule of Benefits. Prenatal Care Office Visits 100% per visit Not Covered No copay or deductible applies. Important Note: Refer to the Physician Services and Pregnancy Expenses sections of the Schedule of Benefits for more information on coverage levels for pregnancy expenses under this Plan, including other prenatal care, delivery and postnatal care office visits. Comprehensive Lactation Support and Counseling Services Lactation Counseling Services 100% per visit Facility or Office Visits No copay or deductible applies. Not Covered. 4
8 Lactation Counseling Services 6* visits per 12 months Not Covered Maximum Visits either in a group or individual setting *Important Note: Visits in excess of the Lactation Counseling Services Maximum as shown above, are covered under the Physician Services office visit section of the Schedule of Benefits. Breast Pumps & Supplies Family Planning - Other Voluntary Termination of Pregnancy Outpatient Office Visits When not part of the office visit Voluntary Sterilization for Males Outpatient Office Visits When not part of the office visit Family Planning Services Female Contraceptive Counseling Services -Office Visits. 100% per item. No copay or deductible applies. Covered at the applicable PCP or Specialist copay then the plan pays 100% No deductible applies 90% per visit after Calendar Year deductible. Covered at the applicable PCP or Specialist copay then the plan pays 100% No deductible applies 90% per visit after Calendar Year deductible. 100% per visit No Calendar Year deductible applies. Not Covered Not Covered. Not Covered. Not Covered. Contraceptive Counseling Services - 2* visits per 12 months Not Covered. Maximum Visits either in a group or individual setting *Important Note: Visits in excess of the Contraceptive Counseling Services Maximum as shown above, are covered under the Physician Services office visit section of the Schedule of Benefits. PLAN FEATURES NETWORK OUT-OF-NETWORK Female Contraceptive Generic Prescription Drugs and Devices provided, administered, or removed, by a Physician during an Office Visits. 100% per item No copay or deductible applies. Not Covered. Family Planning - Female Voluntary Sterilization Inpatient 100% per visit Not Covered 5
9 Outpatient No copay or deductible applies. 100% per visit No copay or deductible applies. Not Covered PLAN FEATURES NETWORK OUT-OF-NETWORK Vision Care Eye Examinations (including refraction) 100% Not Covered No Calendar Year deductible applies. Maximum Benefit per 24 consecutive month period 1 exam Not Covered PLAN FEATURES NETWORK OUT-OF-NETWORK Physician Services <12SECTION025> Office Visits to Primary Care Physician Office visits (non-surgical) to nonspecialist $20 visit copay then the plan pays 100% No Calendar Year deductible applies. Not Covered Specialist Office Visits 90% per visit after Calendar Year deductible applies. Not Covered Walk-In Clinic Visit (Non-Emergency) Preventive Care Services* Immunizations 100% per visit Not Covered Individual Screening and Counseling Services for Tobacco Use Maximum Benefit per visit - Individual Screening and Counseling Services for Tobacco Use No copay or deductible applies. For details, contact your physician, log onto the Aetna website or call the number on the back of your ID card. 100% per visit No copay or deductible applies. Refer to the Preventive Care Benefit section earlier in this Schedule of Benefits for maximums that may apply to these types of services Not Covered Not Applicable Individual Screening and Counseling Services for Obesity 100% per visit Not Covered 6
10 Maximum Benefit per visit - Individual Screening and Counseling Services for Obesity No copay or deductible applies. Refer to the Preventive Care Benefit section earlier in this Schedule of Benefits for maximums that may apply to these types of services Not Applicable *Important Note: Not all preventive care services are available at all Walk-In Clinics. The types of services offered will vary by the provider and location of the clinic. These services may also be obtained from your physician. All Other Services $20 visit copay then the plan pays 100% Not Covered No Calendar Year deductible applies. Physician Office Visits-Surgery $20 visit copay then the plan pays 100% No Calendar Year deductible applies. Not Covered Physician Services for Inpatient Facility and Hospital Visits 90% per visit after Calendar Year deductible Not Covered Administration of Anesthesia 90% after Calendar Year deductible Not Covered Allergy Injections 90% per visit after Calendar Year deductible. Not Covered. PLAN FEATURES NETWORK OUT-OF-NETWORK Emergency Medical Services Hospital Emergency Facility and Physician $100 copay per visit then the plan pays 100% Paid the same as the Network level of benefits. No Calendar Year deductible applies. *See Important note below *Important Note: Please note that as these providers are not Network Providers and do not have a contract with Aetna, the provider may not accept payment of your cost share as payment in full. You may receive a bill for the difference between the amount billed by the provider and the amount paid by this Plan. If the Emergency Room Facility or physician bills you for an amount above your cost share, you are not responsible for paying that amount. Please send Aetna the bill at the address listed on the back of your member ID card and Aetna will resolve any payment dispute with the provider over that amount. Make sure your member ID number is on the bill. Non-Emergency Care in a Hospital Emergency Room Not Covered Not Covered 7
11 Important Notice: A separate hospital emergency room copay or deductible applies for each visit to an emergency room for emergency care. If you are admitted to a hospital as an inpatient immediately following a visit to an emergency room, your copay or deductible is waived. Covered expenses that are applied to the emergency room copay or deductible cannot be applied to any other copay or deductible under your plan. Likewise, covered expenses that are applied to any of your plan s other copays or deductibles cannot be applied to the emergency room copay or deductible. Urgent Care Services Urgent Medical Care (at a non-hospital free standing facility) $50 copay per visit then the plan pays 100% No Calendar Year deductible applies Not Applicable Urgent Medical Care (from other than a non-hospital free standing facility) Refer to Emergency Medical Services and Physician Services above. Refer to Emergency Medical Services and Physician Services above. Non-Urgent Use of Urgent Care Provider (at an Emergency Room or a non-hospital free standing facility) Not Covered Not Covered Important Notice: A separate urgent care copay or deductible applies for each visit to an urgent care provider for urgent care. Covered expenses that are applied to the urgent care copay or deductible cannot be applied to any other copay or deductible under your plan. Likewise, covered expenses that are applied to your plan s other copays or deductibles cannot be applied to the urgent care copay or deductible. PLAN FEATURES NETWORK OUT-OF-NETWORK Outpatient Diagnostic and Preoperative Testing Complex Imaging Services Complex Imaging 90% per test after Calendar Year deductible Not Covered Diagnostic Laboratory Testing 90% per procedure after Calendar Year deductible Not Covered Diagnostic X-Rays Diagnostic X-Rays (except Complex Imaging Services) 90% per procedure after Calendar Year deductible Not Covered 8
12 PLAN FEATURES NETWORK OUT-OF-NETWORK Outpatient Surgery Outpatient Surgery 90% per visit/surgical procedure after Calendar Year deductible Not Covered PLAN FEATURES NETWORK OUT-OF-NETWORK Inpatient Facility Expenses Birthing Center Payable in accordance with the type of expense incurred and the place where service is provided. Not Covered Hospital Facility Expenses Room and Board (including maternity) Other than Room and Board 90% per admission after Calendar Year deductible 90% per admission after Calendar Year deductible Not Covered Not Covered Skilled Nursing Inpatient Facility 90% per admission after Calendar Year deductible Not Covered Maximum Days per Calendar Year 120 days Not Covered PLAN FEATURES NETWORK OUT-OF-NETWORK Specialty Benefits Home Health Care(Outpatient) 90% per visit after the Calendar Year deductible Not Covered Maximum Visits per Calendar Year 120 visits Not Covered Skilled Nursing Care (Outpatient) 90% per visit after the Calendar Year deductible Not Covered Private Duty Nursing (Outpatient) 90% per visit after the Calendar Year deductible Not Covered Maximum Visit Limit per Calendar Year 70 Private Duty Nursing Shifts. Up to 8 hours will be deemed to be one private duty nursing shift. Not Covered 9
13 Hospice Benefits Hospice Care Facility Expenses (Room & Board) Hospice Care Other Expenses during a stay 90% per admission after Calendar Year deductible 90% per admission after Calendar Year deductible Not Covered Not Covered Maximum Benefit per lifetime Unlimited days Not Covered Hospice Outpatient Visits 90% per visit after Calendar Year deductible Not Covered PLAN FEATURES NETWORK OUT-OF-NETWORK Infertility Treatment Basic Infertility Expenses Coverage is for the diagnosis and treatment of the underlying medical condition causing the infertility only. Payable in accordance with the type of expense incurred and the place where service is provided. Not Covered PLAN FEATURES NETWORK OUT-OF-NETWORK Inpatient Treatment of Mental Disorders MENTAL DISORDERS Hospital Facility Expenses Room and Board Other than Room and Board Physician Services $200 per admission copay after Calendar Year deductible then the plan pays 90% 90% per admission after Calendar Year deductible 90% per admission after Calendar Year deductible Not Covered Not Covered Not Covered Inpatient Residential Treatment Facility Expenses Inpatient Residential Treatment Facility Expenses Physician Services $200 per admission copay after Calendar Year deductible then the plan pays 90% 90% per visit after Calendar Year deductible Not Covered Not Covered 10
14 Outpatient Treatment Of Mental Disorders Outpatient Services $20 per visit copay then the plan pays 100% Not Covered No Calendar Year deductible applies PLAN FEATURES NETWORK OUT-OF-NETWORK Inpatient Treatment of Substance Abuse Hospital Facility Expenses Room and Board Other than Room and Board Physician Services $200 per admission copay after Calendar Year deductible then the plan pays 90% 90% per admission after Calendar Year deductible 90% per admission after Calendar Year deductible Not Covered Not Covered Not Covered Inpatient Residential Treatment Facility Expenses Inpatient Residential Treatment Facility Expenses Physician Services $200 per admission copay after Calendar Year deductible then the plan pays 90% 90% per visit after Calendar Year deductible Not Covered Not Covered Outpatient Treatment of Substance Abuse Outpatient Services $20 per visit copay then the plan pays 100% Not Covered No Calendar Year deductible applies PLAN FEATURES NETWORK (IOE Facility) NETWORK (Non-IOE Facility) Transplant Services Facility and Non-Facility Expenses Transplant Facility $200 per admission copay Not Covered Expenses after Calendar Year deductible, then the plan pays 90% OUT-OF-NETWORK Not Covered Transplant Physician Services (including office visits) Payable in accordance with the type of expense incurred and the place where service is provided Not Covered Not Covered 11
15 PLAN FEATURES NETWORK OUT-OF-NETWORK Other Covered Health Expenses Acupuncture in lieu of anesthesia Payable in accordance with the type of expense incurred and the place where service is provided. Not Covered Ground, Air or Water Ambulance 90% after Calendar Year deductible Not Covered Durable Medical and Surgical Equipment 90% per item after the Calendar Year deductible Not Covered Clinical Trial Therapies (Experimental or Investigational Treatment) Payable in accordance with the type of expense incurred and the place where service is provided. Not Covered. Routine Patient Costs Payable in accordance with the type of expense incurred and the place where service is provided. Not Covered. PLAN FEATURES NETWORK OUT-OF-NETWORK Oral and Maxillofacial Treatment (Mouth, Jaws and Teeth) Payable in accordance with the type of expense incurred and the place where service is provided. Not Covered Prosthetic Devices Payable in accordance with the type of expense incurred and the place where service is provided. Not Covered PLAN FEATURES NETWORK OUT-OF-NETWORK Outpatient Therapies Chemotherapy Payable in accordance with the type of expense incurred and the place where service is provided. Not Covered Infusion Therapy Payable in accordance with the type of expense incurred and the place where service is provided. Not Covered 12
16 Radiation Therapy Payable in accordance with the type of expense incurred and the place where service is provided. Not Covered PLAN FEATURES NETWORK OUT-OF-NETWORK Short Term Outpatient Rehabilitation Therapies <12SECTION095> Outpatient Physical, Occupational, and Speech Therapy combined $20 per visit copay then the plan pays 100% Not Covered No Calendar Year deductible applies Combined Physical, Occupational and Speech Therapy Maximum visits per Calendar Year 60 visits Not Covered PLAN FEATURES NETWORK OUT-OF-NETWORK Spinal Manipulation $20 per visit copay then the plan pays 100% Not Covered No Calendar Year deductible applies Spinal Manipulation Maximum visits per Calendar Year 20 visits Not Covered Pharmacy Benefit Copays/Deductibles PER PRESCRIPTION COPAY/DEDUCTIBLE NETWORK OUT-OF-NETWORK Preferred Generic Prescription Drugs For each initial 30 day supply filled at a retail pharmacy $10 Not Covered For all fills of at least a 31 day supply and up to a 90 day supply filled at a mail order pharmacy $20 Not Covered 13
17 Preferred Brand-Name Prescription Drugs For each 30 day supply (retail) $25 Not Covered For more than a 30 day supply but less than a 91 day supply (mail order) $50 Not Covered Non-Preferred Generic Prescription Drugs For each 30 day supply (retail) $10 Not Covered For more than a 30 day supply but less than a 91 day supply (mail order) $20 Not Covered Non-Preferred Brand-Name Prescription Drugs For each initial 30 day supply filled at a retail pharmacy $50 Not Covered For all fills of at least a 31 day supply and up to a 90 day supply filled at a mail order pharmacy $100 Not Covered If a prescriber prescribes a covered brand-name prescription drug where a generic prescription drug equivalent is available and specifies Dispense As Written (DAW), you will pay the cost sharing for the brand-name prescription drug. If you request a covered brand-name prescription drug where a generic prescription drug equivalent is available you will be responsible for the cost difference between the brand-name prescription drug and the generic prescription drug equivalent, plus the applicable cost sharing. Copay and Deductible Waiver Waiver for Risk-Reducing Breast Cancer Prescription Drugs The per prescription copay/deductible and any prescription drug Calendar Year deductible will not apply to risk-reducing breast cancer generic prescription drugs when obtained at a network pharmacy. This means that such risk-reducing breast cancer generic prescription drugs will be paid at 100%. Deductible and copayment/coinsurance waiver for tobacco cessation prescription and over-thecounter drugs The prescription drug deductible and the per prescription copayment/coinsurance will not apply to the first two 90-day treatment regimens for tobacco cessation prescription drugs and OTC drugs when obtained at a network pharmacy. This means that such prescription drugs and OTC drugs will be paid at 100%. Your prescription drug deductible and any prescription copayment/coinsurance will apply after those two regimens have been exhausted. Waiver for Prescription Drug Contraceptives The per prescription copay/deductible and any prescription drug Calendar Year deductible will not apply to contraceptive methods that are: generic prescription drugs; contraceptive devices; or 14
18 FDA-approved female generic emergency contraceptives, when obtained at a network pharmacy. This means that such contraceptive methods will be paid at 100%. Refer to the Pharmacy Plan Features for information on coverage for FDA-Approved female over-the-counter contraceptives (Non-Emergency). The per prescription copay/deductible and any prescription drug Calendar Year deductible continue to apply: When the contraceptive methods listed above are obtained at an out-of-network pharmacy For contraceptive methods that are: - brand-name prescription drugs and devices and - FDA-approved female brand-name emergency contraceptives, that have a generic equivalent, or generic alternative available within the same therapeutic drug class obtained at an out-of-network pharmacy or network pharmacy unless you are granted a medical exception. PLAN FEATURES NETWORK OUT-OF-NETWORK FDA-Approved Female Generic Over-the-Counter Contraceptives 100% per supply No copay or deductible applies. Not covered. For each 30 day supply filled at a retail pharmacy FDA-Approved Female Generic Emergency Over-the-Counter Contraceptives 100% per supply No copay or deductible applies. Not covered. Important Note: This Plan does not cover all over-the-counter (OTC) contraceptives. For a current listing, contact Member Services by logging on the Aetna website at or calling the toll-free number on the back of the ID card. Preventive Care Drugs and Supplements Preventive care drugs and supplements filled at a pharmacy with a prescription: Coverage will be subject to any sex, age, medical condition, family history, and frequency guidelines in the recommendations of the United States Preventive Services Task Force. For details on the guidelines and the current list of covered preventive care drugs and supplements, contact your physician or Member Services by logging onto the Aetna website or calling the number on the back of your ID card. 100% per item. No copay or deductible applies. Not Covered. 15
19 Important Note: Refer to the Booklet and the Preventive Care section for a complete description of the preventive care drugs and supplements covered under this Plan and for any limitations that apply to these benefits. Coinsurance Prescription Drug Plan Coinsurance NETWORK OUT-OF-NETWORK 100% of the negotiated charge Not Covered The prescription drug plan coinsurance is the percentage of prescription drug covered expenses that the plan pays after any applicable deductibles and copays have been met. Expense Provisions The following provisions apply to your health expense plan. This section describes cost sharing features, benefit maximums and other important provisions that apply to your Plan. The specific cost sharing features and the applicable dollar amounts or benefit percentages are contained in the attached health expense sections of this Schedule of Benefits. This Schedule of Benefits replaces any Schedule of Benefits previously in effect under your plan of health benefits. KEEP THIS SCHEDULE OF BENEFITS WITH YOUR BOOKLET. Deductible Provisions All covered expenses accumulate toward the network provider deductible except for those covered expenses identified later in this Schedule of Benefits. You and each of your covered dependents have separate Calendar Year deductibles. This Plan has individual and family Calendar Year deductibles. For purposes of Calendar Year deductible provision below, an individual means an employee enrolled for self only coverage with no dependent coverage and a family means an employee enrolled with one or more dependents. The family deductible can be met by one family member, or a combination of family members. Network Provider Calendar Year Deductible Individual This is the amount of covered expenses that you incur each Calendar Year from a network provider for which no benefits will be paid. After covered expenses reach this individual Calendar Year deductible, this Plan will begin to pay benefits for covered expenses that you incur from a network provider for the rest of the Calendar Year. You and each of your covered dependents have separate Calendar Year deductibles. Each of you must meet your deductible separately and they cannot be combined. This Plan has individual and family Calendar Year deductibles. 16
20 Network Provider Calendar Year Deductible Individual This is the amount of covered expenses that you and each of your covered dependents incur each Calendar Year from a network provider for which no benefits will be paid. This individual Calendar Year deductible applies separately to you and each of your covered dependents. After covered expenses reach this individual Calendar Year deductible; this Plan will begin to pay benefits for covered expenses that you incur from a network provider for the rest of the Calendar Year. Family Deductible Limit When you and each of your covered dependents incur covered expenses that apply towards the individual Calendar Year deductibles, these expenses will also count toward a family deductible limit. To satisfy this family deductible limit for the rest of the Calendar Year, the following must happen: The combined covered expenses that you and each of your covered dependents incur towards the individual Calendar Year deductibles must reach this family deductible limit in a Calendar Year. When this occurs in a Calendar Year, the individual Calendar Year deductibles for you and your covered dependents will be considered to be met for the rest of the Calendar Year. Copayments and Benefit Deductible Provisions Copayment, Copay This is a specified dollar amount or percentage of the negotiated charge required to be paid by you at the time you receive a covered service from a network provider. It represents a portion of the applicable expense. Per Admission Copayment A Per Admission Copayment is an amount you are required to pay when you or a covered dependent have a stay in an inpatient facility. A copayment is a specified dollar amount or percentage of the negotiated charge required to be paid by you at the time you receive a covered service from a network provider. It represents a portion of the applicable expense. Separate copayments may apply per facility. These copayments are in addition to any other copayments applicable under this plan. They may apply to each stay or they may apply on a per day basis up to a per admission maximum amount. Covered expenses applied to the per admission copayment cannot be applied to any other copayment required in your plan. Likewise, covered expenses applied to your plan s other copayments cannot be applied to meet the per admission copayment. For the stay of a well newborn baby (starting at birth), the per admission copayment amount will not exceed the hospital s actual room and board charge on the first day of the stay. Payment Provisions Payment Percentage This is the percentage of your covered expenses that the plan pays and the percentage of covered expenses that you pay. The percentage that the plan pays is referred to as the Plan Payment Percentage. Once applicable deductibles have been met, your plan will pay a percentage of the covered expenses, and you will be responsible for the rest of the costs. The payment percentage may vary by the type of expense. Refer to your Schedule of Benefits for payment percentage amounts for each covered benefit. 17
21 Maximum Out-of-Pocket Limit The Maximum Out-of-Pocket Limit is the maximum amount you are responsible to pay for covered expenses during the Calendar Year. This Plan has an individual Maximum Out-of-Pocket Limit. As to the individual Maximum Out-of-Pocket Limit, each of you must meet your Maximum Out-of-Pocket Limit separately and they cannot be combined and applied towards one limit. Certain covered expenses do not apply toward the Maximum Out-of-Pocket Limit. See list below. Network Provider Maximum Out-of-Pocket Limit Individual Once the amount of eligible network provider expenses you or your covered dependents have paid during the Calendar Year meets the individual Maximum Out-of-Pocket Limit, this Plan will pay 100% of such covered expenses that apply toward the limit for the remainder of the Calendar Year for that person. Family Maximum Out-of-Pocket Limit When you and each of your covered dependents incur covered expenses that apply towards the individual Calendar Year network provider Maximum Out-of-Pocket Limit, these expenses will also count toward a family network provider Maximum Out-of-Pocket Limit. To satisfy this family network provider Maximum Out-of-Pocket Limit for the rest of the Calendar Year, the following must happen: The family Maximum Out-of-Pocket Limit is a cumulative Maximum Out-of-Pocket Limit for all family members. The family network provider Maximum Out-of-Pocket Limit can be met by a combination of family members with no single individual within the family contributing more than the individual network provider Maximum Out-of-Pocket Limit amount in a Calendar Year. Covered expenses that are subject to the Maximum Out-of-Pocket Limit include prescription drug expenses provided under the Medical or Prescription drug Plans, as applicable. Expenses That Do Not Apply to Your In-Network Out-of-Pocket Limit Certain covered expenses do not apply toward your plan in-network out-of-pocket limit. These include: Charges over the recognized charge; Non-covered expenses; Expenses for non-emergency use of the emergency room; Expenses incurred for non-urgent use of an urgent care provider; and Expenses that are not paid, or precertification benefit reductions because a required precertification for the service(s) or supply was not obtained from Aetna. Expenses That Do Not Apply to Your Out-of-Pocket Limit Certain covered expenses do not apply toward your plan out-of-pocket limit. These include: Charges over the recognized charge; Non-covered expenses; Expenses for non-emergency use of the emergency room; 18
22 Expenses incurred for non-urgent use of an urgent care provider; and Expenses that are not paid, or precertification benefit reductions because a required precertification for the service(s) or supply was not obtained from Aetna. General This Schedule of Benefits replaces any similar Schedule of Benefits previously in effect under your plan of benefits. Requests for coverage other than that to which you are entitled in accordance with this Schedule of Benefits cannot be accepted. This Schedule is part of your Booklet and should be kept with your Booklet. 19
23 Preface The medical benefits plan described in this Booklet is a benefit plan of the Employer. These benefits are not insured with Aetna or any of its affiliates, but will be paid from the Employer's funds. Aetna and its HMO affiliates will provide certain administrative services under the Aetna medical benefits plan. Aetna agrees with the Employer to provide administrative services in accordance with the conditions, rights, and privileges as set forth in this Booklet. The Employer selects the products and benefit levels under the Aetna medical benefits plan. The Booklet describes your rights and obligations, what the Aetna medical benefits plan covers, and how benefits are paid for that coverage. It is your responsibility to understand the terms and conditions in this Booklet. Your Booklet includes the Schedule of Benefits and any amendments. This Booklet replaces and supercedes all Aetna Booklets describing coverage for the medical benefits plan described in this Booklet that you may previously have received. Employer: SAMPLE Contract Number: Effective Date: 00/00/00 Issue Date: 00/00/00 Booklet Number: 5 Coverage for You and Your Dependents Health Expense Coverage Benefits are payable for covered health care expenses that are incurred by you or your covered dependents while coverage is in effect. An expense is incurred on the day you receive a health care service or supply. Coverage under this plan is non-occupational. Only non-occupational injuries and non-occupational illnesses are covered. Refer to the What the Plan Covers section of the Booklet for more information about your coverage. Treatment Outcomes of Covered Services Aetna is not a provider of health care services and therefore is not responsible for and does not guarantee any results or outcomes of the covered health care services and supplies you receive. Except for Aetna RX Home Delivery LLC, providers of health care services, including hospitals, institutions, facilities or agencies, are independent contractors and are neither agents nor employees of Aetna or its affiliates. 20
24 When Your Coverage Begins Who Is Eligible How and When to Enroll When Your Coverage Begins Throughout this section you will find information on who can be covered under the plan, how to enroll and what to do when there is a change in your life that affects coverage. In this section, you means the employee. Who Is Eligible Employees To be covered by this plan, the following requirements must be met: You will need to be in an eligible class, as defined below; and You will need to meet the eligibility date criteria described below. Determining if You Are in an Eligible Class You are in an eligible class if: You are a regular full-time employee, as defined by your employer. Determining When You Become Eligible You become eligible for the plan on your eligibility date, which is determined as follows. On the Effective Date of the Plan If you are in an eligible class on the effective date of this plan, your coverage eligibility date is the effective date of the plan. After the Effective Date of the Plan If you are hired after the effective date of this plan, your coverage eligibility date is the date you are hired. If you enter an eligible class after the effective date of this plan, your coverage eligibility date is the date you enter the eligible class. Obtaining Coverage for Dependents Your dependents can be covered under this Plan. You may enroll the following dependents: Your spouse. Your dependent children. Aetna will rely upon your employer to determine whether or not a person meets the definition of a dependent for coverage under this Plan. This determination will be conclusive and binding upon all persons for the purposes of this Plan. Coverage for Dependent Children To be eligible for coverage, a dependent child must be under 26 years of age. 21
25 An eligible dependent child includes: Your biological children; Your stepchildren; Your legally adopted children; Your foster children, including any children placed with you for adoption; Any children for whom you are responsible under court order; Your grandchildren in your court-ordered custody; and Any other child with whom you have a parent-child relationship. Coverage for a handicapped child may be continued past the age limits shown above. See Handicapped Dependent Children for more information. Important Reminder Keep in mind that you cannot receive coverage under this Plan as: Both an employee and a dependent; or A dependent of more than one employee. How and When to Enroll Initial Enrollment in the Plan You will be provided with plan benefit and enrollment information when you first become eligible to enroll. You will need to enroll in a manner determined by Aetna and your employer. To complete the enrollment process, you will need to provide all requested information for yourself and your eligible dependents. You will also need to agree to make required contributions for any contributory coverage. Your employer will determine the amount of your plan contributions, which you will need to agree to before you can enroll. Your employer will advise you of the required amount of your contributions and will deduct your contributions from your pay. Remember plan contributions are subject to change. You will need to enroll within 31 days of your eligibility date. Otherwise, you may be considered a Late Enrollee. If you miss the enrollment period, you will not be able to participate in the plan until the next annual enrollment period, unless you qualify under a Special Enrollment Period, as described below. If you do not enroll for coverage when you first become eligible, but wish to do so later, your employer will provide you with information on when and how you can enroll. Newborns are automatically covered for 31 days after birth. To continue coverage after 31 days, you will need to complete a change form and return it to your employer within the 31-day enrollment period. Late Enrollment If you do not enroll during the Initial Enrollment Period, or a subsequent annual enrollment period, you and your eligible dependents may be considered Late Enrollees and coverage may be deferred until the next annual enrollment period. If, at the time of your initial enrollment, you elect coverage for yourself only and later request coverage for your eligible dependents, they may be considered Late Enrollees. You must return your completed enrollment form before the end of the next annual enrollment period as described below. However, you and your eligible dependents may not be considered Late Enrollees if you qualify for one of the circumstances described in the Special Enrollment Periods section below. 22
26 Annual Enrollment During the annual enrollment period, you will have the opportunity to review your coverage needs for the upcoming year. During this period, you have the option to change your coverage. The choices you make during this annual enrollment period will become effective the following year. If you do not enroll yourself or a dependent for coverage when you first become eligible, but wish to do so later, you will need to do so during the next annual enrollment period, unless you qualify under one of the Special Enrollment Periods, as described below. Special Enrollment Periods You will not be considered a Late Enrollee if you qualify under a Special Enrollment Period as defined below. If one of these situations applies, you may enroll before the next annual enrollment period. Loss of Other Health Care Coverage You or your dependents may qualify for a Special Enrollment Period if: You did not enroll yourself or your dependent when you first became eligible or during any subsequent annual enrollments because, at that time: You or your dependents were covered under other creditable coverage; and You refused coverage and stated, in writing, at the time you refused coverage that the reason was that you or your dependents had other creditable coverage; and You or your dependents are no longer eligible for other creditable coverage because of one of the following: The end of your employment; A reduction in your hours of employment (for example, moving from a full-time to part-time position); The ending of the other plan s coverage; Death; Divorce or legal separation; Employer contributions toward that coverage have ended; COBRA coverage ends; The employer s decision to stop offering the group health plan to the eligible class to which you belong; Cessation of a dependent s status as an eligible dependent as such is defined under this Plan; With respect to coverage under Medicaid or an S-CHIP Plan, you or your dependents no longer qualify for such coverage; or You or your dependents have reached the lifetime maximum of another Plan for all benefits under that Plan. You or your dependents become eligible for premium assistance, with respect to coverage under the group health plan, under Medicaid or an S-CHIP Plan. You will need to enroll yourself or a dependent for coverage within: 31 days of when other creditable coverage ends; within 60 days of when coverage under Medicaid or an S-CHIP Plan ends; or within 60 days of the date you or your dependents become eligible for Medicaid or S-CHIP premium assistance. Evidence of termination of creditable coverage must be provided to your employer or the party it designates. If you do not enroll during this time, you will need to wait until the next annual enrollment period. 23
27 New Dependents You and your dependents may qualify for a Special Enrollment Period if: You did not enroll when you were first eligible for coverage; and You later acquire a dependent, as defined under the plan, through marriage, birth, adoption, or placement for adoption; and You elect coverage for yourself and your dependent within 31 days of acquiring the dependent. Your spouse or child who meets the definition of a dependent under the plan may qualify for a Special Enrollment Period if: You did not enroll them when they were first eligible; and You later elect coverage for them within 31 days of a court order requiring you to provide coverage. You will need to report any new dependents by completing a change form, which is available from your employer. The form must be completed and returned to your employer within 31 days of the change. If you do not return the form within 31 days of the change, you will need to make the changes during the next annual enrollment period. If You Adopt a Child Your plan will cover a child who is placed for adoption. This means you have taken on the legal obligation for total or partial support of a child whom you plan to adopt. Your plan will provide coverage for a child who is placed with you for adoption if: The child meets the plan s definition of an eligible dependent on the date he or she is placed for adoption; and You request coverage for the child in writing within 31 days of the placement; Proof of placement will need to be presented to your employer prior to the dependent enrollment; Any coverage limitations for a preexisting condition will not apply to a child placed with you for adoption provided that the placement occurs on or after the effective date of your coverage. When You Receive a Qualified Child Support Order A Qualified Medical Child Support Order (QMCSO) is a court order requiring a parent to provide health care coverage to one or more children. Your plan will provide coverage for a child who is covered under a QMCSO, if: The child meets the plan s definition of an eligible dependent; and You request coverage for the child in writing within 31 days of the court order. Coverage for the dependent will become effective on the date of the court order. Any coverage limitations for a preexisting condition will not apply, as long as you submit a written request for coverage within the 31-day period. If you do not request coverage for the child within the 31-day period, you will need to wait until the next annual enrollment period. Under a QMCSO, if you are the non-custodial parent, the custodial parent may file claims for benefits. Benefits for such claims will be paid to the custodial parent. 24
28 When Your Coverage Begins Your Effective Date of Coverage If you have met all the eligibility requirements, your coverage takes effect on the later of: The date you are eligible for coverage; and The date your enrollment information is received; and The date your required contribution is received by Aetna. If your completed enrollment information is not received within 31 days of your eligibility date, the rules under the Special or Late Enrollment Periods section will apply. Important Notice: You must pay the required contribution in full or coverage will not be effective. Your Dependent s Effective Date of Coverage Your dependent s coverage takes effect on the same day that your coverage becomes effective, if you have enrolled them in the plan. Note: New dependents need to be reported to your employer within 31 days because they may affect your contributions. If you do not report a new dependent within 31 days of his or her eligibility date, the rules under the Special or Late Enrollment Periods section will apply. 25
What Your Plan Covers and How Benefits are Paid BENEFIT PLAN. Prepared Exclusively for Leidos, Inc. Aetna Choice POS II (HDHP) - Advantage Plan
 BENEFIT PLAN Prepared Exclusively for Leidos, Inc. What Your Plan Covers and How Benefits are Paid Aetna Choice POS II (HDHP) - Advantage Plan Table of Contents Schedule of Benefits...1 Preface...18 Coverage
BENEFIT PLAN Prepared Exclusively for Leidos, Inc. What Your Plan Covers and How Benefits are Paid Aetna Choice POS II (HDHP) - Advantage Plan Table of Contents Schedule of Benefits...1 Preface...18 Coverage
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Appendix A. Prepared Exclusively for The Dow Chemical Company
 Appendix A BENEFIT PLAN Prepared Exclusively for The Dow Chemical Company What Your Plan Covers and How Benefits are Paid Choice POS II (MAP Plus Option 2 - High Deductible Health Plan (HDHP) with Prescription
Appendix A BENEFIT PLAN Prepared Exclusively for The Dow Chemical Company What Your Plan Covers and How Benefits are Paid Choice POS II (MAP Plus Option 2 - High Deductible Health Plan (HDHP) with Prescription
FEATURES NETWORK OUT-OF-NETWORK
 Schedule of Benefits Employer: The Vanguard Group, Inc. ASA: 697478-A Issue Date: January 1, 2014 Effective Date: January 1, 2014 Schedule: 3B Booklet Base: 3 For: Choice POS II - 950 Option - Retirees
Schedule of Benefits Employer: The Vanguard Group, Inc. ASA: 697478-A Issue Date: January 1, 2014 Effective Date: January 1, 2014 Schedule: 3B Booklet Base: 3 For: Choice POS II - 950 Option - Retirees
What Your Plan Covers and How Benefits are Paid BENEFIT PLAN. Prepared Exclusively for Vanderbilt University. Aetna Choice POS II Health Fund Plan
 BENEFIT PLAN Prepared Exclusively for Vanderbilt University What Your Plan Covers and How Benefits are Paid Aetna Choice POS II Health Fund Plan Table of Contents Schedule of Benefits... Issued with Your
BENEFIT PLAN Prepared Exclusively for Vanderbilt University What Your Plan Covers and How Benefits are Paid Aetna Choice POS II Health Fund Plan Table of Contents Schedule of Benefits... Issued with Your
Additional Information Provided by Aetna Life Insurance Company
 Additional Information Provided by Aetna Life Insurance Company Inquiry Procedure The plan of benefits described in the Booklet-Certificate is underwritten by: Aetna Life Insurance Company (Aetna) 151
Additional Information Provided by Aetna Life Insurance Company Inquiry Procedure The plan of benefits described in the Booklet-Certificate is underwritten by: Aetna Life Insurance Company (Aetna) 151
100% Percentage at which the Fund will reimburse Fund Administration
 FUND FEATURES HealthFund Amount $500 Employee $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund amount reflected is on a per
FUND FEATURES HealthFund Amount $500 Employee $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund amount reflected is on a per
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Prepared Exclusively for Yale University
 BENEFIT PLAN Prepared Exclusively for Yale University What Your Plan Covers and How Benefits are Paid Aetna Choice POS II - Faculty, Management and Professional Staff Table of Contents Preface...1 Important
BENEFIT PLAN Prepared Exclusively for Yale University What Your Plan Covers and How Benefits are Paid Aetna Choice POS II - Faculty, Management and Professional Staff Table of Contents Preface...1 Important
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Prepared Exclusively for Cerner Corporation (Expatriate Employees)
 BENEFIT PLAN Prepared Exclusively for Cerner Corporation (Expatriate Employees) What Your Plan Covers and How Benefits are Paid PPO Medical, PPO Dental, Basic Vision and Pharmacy Aetna Life and Casualty
BENEFIT PLAN Prepared Exclusively for Cerner Corporation (Expatriate Employees) What Your Plan Covers and How Benefits are Paid PPO Medical, PPO Dental, Basic Vision and Pharmacy Aetna Life and Casualty
What Your Plan Covers and How Benefits are Paid BENEFIT PLAN. Prepared Exclusively for The McClatchy Company. Aetna Choice Plan
 BENEFIT PLAN Prepared Exclusively for The McClatchy Company What Your Plan Covers and How Benefits are Paid Aetna Choice Plan Table of Contents Preface...1 Important Information Regarding Availability
BENEFIT PLAN Prepared Exclusively for The McClatchy Company What Your Plan Covers and How Benefits are Paid Aetna Choice Plan Table of Contents Preface...1 Important Information Regarding Availability
Employee + 2 Dependents
 FUND FEATURES HealthFund Amount $500 Individual $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance Percentage at
FUND FEATURES HealthFund Amount $500 Individual $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance Percentage at
PDS Tech, Inc Proposed Effective Date: 01-01-2012 Aetna HealthFund Aetna Choice POS ll - ASC
 FUND FEATURES HealthFund Amount $500 Individual $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance 100% Percentage
FUND FEATURES HealthFund Amount $500 Individual $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance 100% Percentage
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Prepared Exclusively for ConocoPhillips
 BENEFIT PLAN Prepared Exclusively for ConocoPhillips What Your Plan Covers and How Benefits are Paid PPO Medical, Pharmacy, and Comprehensive Dental Inpatriate Plan Aetna Life Insurance Company Booklet-Certificate
BENEFIT PLAN Prepared Exclusively for ConocoPhillips What Your Plan Covers and How Benefits are Paid PPO Medical, Pharmacy, and Comprehensive Dental Inpatriate Plan Aetna Life Insurance Company Booklet-Certificate
California Small Group MC Aetna Life Insurance Company
 PLAN FEATURES Deductible (per calendar year) $3,000 Individual $6,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered expenses accumulate separately
PLAN FEATURES Deductible (per calendar year) $3,000 Individual $6,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered expenses accumulate separately
Unlimited except where otherwise indicated.
 PLAN FEATURES Deductible (per calendar year) $1,250 Individual $5,000 Individual $2,500 Family $10,000 Family All covered expenses including prescription drugs accumulate separately toward both the preferred
PLAN FEATURES Deductible (per calendar year) $1,250 Individual $5,000 Individual $2,500 Family $10,000 Family All covered expenses including prescription drugs accumulate separately toward both the preferred
100% Fund Administration
 FUND FEATURES HealthFund Amount $500 Employee $750 Employee + Spouse $750 Employee + Child(ren) $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance Percentage at which the Fund
FUND FEATURES HealthFund Amount $500 Employee $750 Employee + Spouse $750 Employee + Child(ren) $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance Percentage at which the Fund
Business Life Insurance - Health & Medical Billing Requirements
 PLAN FEATURES Deductible (per plan year) $2,000 Employee $2,000 Employee $3,000 Employee + Spouse $3,000 Employee + Spouse $3,000 Employee + Child(ren) $3,000 Employee + Child(ren) $4,000 Family $4,000
PLAN FEATURES Deductible (per plan year) $2,000 Employee $2,000 Employee $3,000 Employee + Spouse $3,000 Employee + Spouse $3,000 Employee + Child(ren) $3,000 Employee + Child(ren) $4,000 Family $4,000
California Small Group MC Aetna Life Insurance Company
 PLAN FEATURES Deductible (per calendar year) $1,000 per member $1,000 per member Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered expenses accumulate
PLAN FEATURES Deductible (per calendar year) $1,000 per member $1,000 per member Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered expenses accumulate
Individual. Employee + 1 Family
 FUND FEATURES HealthFund Amount Individual Employee + 1 Family $750 $1,125 $1,500 Amount contributed to the Fund by the employer is reflected above. Fund Amount reflected is on a per calendar year basis.
FUND FEATURES HealthFund Amount Individual Employee + 1 Family $750 $1,125 $1,500 Amount contributed to the Fund by the employer is reflected above. Fund Amount reflected is on a per calendar year basis.
$6,350 Individual $12,700 Individual
 PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible $5,000 Individual $10,000 Individual $10,000 Family $20,000 Family All covered expenses accumulate separately toward the preferred or non-preferred Deductible.
PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible $5,000 Individual $10,000 Individual $10,000 Family $20,000 Family All covered expenses accumulate separately toward the preferred or non-preferred Deductible.
PARTICIPATING PROVIDERS / REFERRED Deductible (per calendar year)
 Your HMO Plan Primary Care Physician - You choose a Primary Care Physician. The Aetna HMO Deductible provider network gives you access to a wide selection of Primary Care Physicians ( PCP's) and Specialists
Your HMO Plan Primary Care Physician - You choose a Primary Care Physician. The Aetna HMO Deductible provider network gives you access to a wide selection of Primary Care Physicians ( PCP's) and Specialists
PLAN DESIGN AND BENEFITS - PA Health Network Option AHF HRA 1.3. Fund Pays Member Responsibility
 HEALTHFUND PLAN FEATURES HealthFund Amount (Per plan year. Fund changes between tiers requires a life status change qualifying event.) Fund Coinsurance (Percentage at which the Fund will reimburse) Fund
HEALTHFUND PLAN FEATURES HealthFund Amount (Per plan year. Fund changes between tiers requires a life status change qualifying event.) Fund Coinsurance (Percentage at which the Fund will reimburse) Fund
Medical Plan - Healthfund
 18 Medical Plan - Healthfund Oklahoma City Community College Effective Date: 07-01-2010 Aetna HealthFund Open Choice (PPO) - Oklahoma PLAN DESIGN AND BENEFITS PROVIDED BY AETNA LIFE INSURANCE COMPANY -
18 Medical Plan - Healthfund Oklahoma City Community College Effective Date: 07-01-2010 Aetna HealthFund Open Choice (PPO) - Oklahoma PLAN DESIGN AND BENEFITS PROVIDED BY AETNA LIFE INSURANCE COMPANY -
PLAN DESIGN AND BENEFITS POS Open Access Plan 1944
 PLAN FEATURES PARTICIPATING Deductible (per calendar year) $3,000 Individual $9,000 Family $4,000 Individual $12,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being
PLAN FEATURES PARTICIPATING Deductible (per calendar year) $3,000 Individual $9,000 Family $4,000 Individual $12,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being
PLAN DESIGN & BENEFITS MEDICAL PLAN PROVIDED BY AETNA LIFE INSURANCE COMPANY
 Gettysburg College, Inc. PLAN FEATURES Deductible (per calendar year) $500 Individual $1,500 Individual $1,000 Family $3,000 Family All covered expenses accumulate separately toward the preferred or non-preferred
Gettysburg College, Inc. PLAN FEATURES Deductible (per calendar year) $500 Individual $1,500 Individual $1,000 Family $3,000 Family All covered expenses accumulate separately toward the preferred or non-preferred
PREFERRED CARE. All covered expenses, including prescription drugs, accumulate toward both the preferred and non-preferred Payment Limit.
 PLAN FEATURES Deductible (per plan year) $300 Individual $300 Individual None Family None Family All covered expenses, excluding prescription drugs, accumulate toward both the preferred and non-preferred
PLAN FEATURES Deductible (per plan year) $300 Individual $300 Individual None Family None Family All covered expenses, excluding prescription drugs, accumulate toward both the preferred and non-preferred
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Adobe Systems Incorporated. Aetna Choice POS II
 Adobe Systems Incorporated Aetna Choice POS II BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group Welfare
Adobe Systems Incorporated Aetna Choice POS II BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group Welfare
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Adobe Systems Incorporated. Aetna HealthFund HRA Plan
 Adobe Systems Incorporated Aetna HealthFund HRA Plan BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group
Adobe Systems Incorporated Aetna HealthFund HRA Plan BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group
PLAN DESIGN AND BENEFITS AETNA LIFE INSURANCE COMPANY - Insured
 PLAN FEATURES Deductible (per calendar year) Individual $750 Individual $1,500 Family $2,250 Family $4,500 All covered expenses accumulate simultaneously toward both the preferred and non-preferred Deductible.
PLAN FEATURES Deductible (per calendar year) Individual $750 Individual $1,500 Family $2,250 Family $4,500 All covered expenses accumulate simultaneously toward both the preferred and non-preferred Deductible.
PLAN DESIGN AND BENEFITS - Tx OAMC Basic 2500-10 PREFERRED CARE
 PLAN FEATURES Deductible (per calendar year) $2,500 Individual $4,000 Individual $7,500 Family $12,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
PLAN FEATURES Deductible (per calendar year) $2,500 Individual $4,000 Individual $7,500 Family $12,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
National PPO 1000. PPO Schedule of Payments (Maryland Small Group)
 PPO Schedule of Payments (Maryland Small Group) National PPO 1000 The benefits outlined in this Schedule are in addition to the benefits offered under Coventry Health & Life Insurance Company Small Employer
PPO Schedule of Payments (Maryland Small Group) National PPO 1000 The benefits outlined in this Schedule are in addition to the benefits offered under Coventry Health & Life Insurance Company Small Employer
PLAN DESIGN AND BENEFITS - New York Open Access EPO 1-10/10
 PLAN FEATURES Deductible (per calendar year) $1,000 Individual $3,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services,
PLAN FEATURES Deductible (per calendar year) $1,000 Individual $3,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services,
1 exam every 12 months for members age 22 to age 65; 1 exam every 12 months for adults age 65 and older. Routine Well Child
 PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $1,000 Individual $1,000 Individual $2,000 Family $2,000 Family All covered expenses accumulate separately toward the preferred or
PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $1,000 Individual $1,000 Individual $2,000 Family $2,000 Family All covered expenses accumulate separately toward the preferred or
PLAN DESIGN AND BENEFITS HMO Open Access Plan 912
 PLAN FEATURES Deductible (per calendar year) $1,000 Individual $2,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services
PLAN FEATURES Deductible (per calendar year) $1,000 Individual $2,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services
PLAN DESIGN AND BENEFITS STANDARD HEALTH BENEFITS PLAN NJ HMO $30 PLAN (Also Marketed As: NJ SGB HMO $30/$300/D (5/10K) Plan)
 PLAN FEATURES Deductible (per calendar year) Plan Coinsurance Maximum Out-of-Pocket (per calendar year) $5,000 Individual $10,000 Family All covered expenses apply toward the Maximum Out-of-Pocket. Once
PLAN FEATURES Deductible (per calendar year) Plan Coinsurance Maximum Out-of-Pocket (per calendar year) $5,000 Individual $10,000 Family All covered expenses apply toward the Maximum Out-of-Pocket. Once
THE MITRE CORPORATION PPO High Deductible Plan with a Health Saving Account (HSA)
 THE MITRE CORPORATION PPO High Deductible Plan with a Health Saving Account (HSA) Effective Date: 01-01-2016 PLAN FEATURES Annual Deductible $1,500 Employee $3,000 Employee $3,000 Employee + 1 Dependent
THE MITRE CORPORATION PPO High Deductible Plan with a Health Saving Account (HSA) Effective Date: 01-01-2016 PLAN FEATURES Annual Deductible $1,500 Employee $3,000 Employee $3,000 Employee + 1 Dependent
SMALL GROUP PLAN DESIGN AND BENEFITS OPEN CHOICE OUT-OF-STATE PPO PLAN - $1,000
 PLAN FEATURES PREFERRED CARE NON-PREFERRED CARE Deductible (per calendar year; applies to all covered services) $1,000 Individual $3,000 Family $2,000 Individual $6,000 Family Plan Coinsurance ** 80% 60%
PLAN FEATURES PREFERRED CARE NON-PREFERRED CARE Deductible (per calendar year; applies to all covered services) $1,000 Individual $3,000 Family $2,000 Individual $6,000 Family Plan Coinsurance ** 80% 60%
Bates College Effective date: 01-01-2010 HMO - Maine PLAN DESIGN AND BENEFITS PROVIDED BY AETNA HEALTH INC. - FULL RISK PLAN FEATURES
 PLAN FEATURES Deductible (per calendar year) $500 Individual $1,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Once Family Deductible is met, all family
PLAN FEATURES Deductible (per calendar year) $500 Individual $1,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Once Family Deductible is met, all family
New York Small Group Indemnity Aetna Life Insurance Company Plan Effective Date: 10/01/2010. PLAN DESIGN AND BENEFITS - NY Indemnity 1-10/10*
 PLAN FEATURES Deductible (per calendar year) $2,500 Individual $7,500 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services,
PLAN FEATURES Deductible (per calendar year) $2,500 Individual $7,500 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services,
PLAN DESIGN AND BENEFITS - Tx OAMC 2500 08 PREFERRED CARE
 PLAN FEATURES Deductible (per calendar year) $2,500 Individual $5,000 Individual $7,500 3 Individuals per $15,000 3 Individuals per Unless otherwise indicated, the Deductible must be met prior to benefits
PLAN FEATURES Deductible (per calendar year) $2,500 Individual $5,000 Individual $7,500 3 Individuals per $15,000 3 Individuals per Unless otherwise indicated, the Deductible must be met prior to benefits
PLAN DESIGN AND BENEFITS - Tx OAMC 1500-10 PREFERRED CARE
 PLAN FEATURES Deductible (per calendar year) $1,500 Individual $3,000 Individual $4,500 Family $9,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
PLAN FEATURES Deductible (per calendar year) $1,500 Individual $3,000 Individual $4,500 Family $9,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
Prepared: 04/06/2012 04:19 PM
 PLAN FEATURES NON- Deductible (per calendar year) $2,000 Individual $4,000 Individual $6,000 Family $12,000 Family All covered expenses accumulate simultaneously toward both the preferred and non-preferred
PLAN FEATURES NON- Deductible (per calendar year) $2,000 Individual $4,000 Individual $6,000 Family $12,000 Family All covered expenses accumulate simultaneously toward both the preferred and non-preferred
CA Group Business 2-50 Employees
 PLAN FEATURES Network Primary Care Physician Selection Deductible (per calendar year) Member Coinsurance Copay Maximum (per calendar year) Lifetime Maximum Referral Requirement PHYSICIAN SERVICES Primary
PLAN FEATURES Network Primary Care Physician Selection Deductible (per calendar year) Member Coinsurance Copay Maximum (per calendar year) Lifetime Maximum Referral Requirement PHYSICIAN SERVICES Primary
IL Small Group MC Open Access Aetna Life Insurance Company Plan Effective Date: 10/01/2010 PLAN DESIGN AND BENEFITS- MC CDHP $2,500 90/70 (10/10)
 PLAN FEATURES Deductible (per calendar ) $2,500 Individual $5,000 Individual $7,500 Family $15,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered
PLAN FEATURES Deductible (per calendar ) $2,500 Individual $5,000 Individual $7,500 Family $15,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered
PPO Schedule of Payments (Maryland Large Group) Qualified High Deductible Health Plan National QA2000-20
 PPO Schedule of Payments (Maryland Large Group) Qualified High Health Plan National QA2000-20 Benefit Year Individual Family (Amounts for Participating and s services are separated in calculating when
PPO Schedule of Payments (Maryland Large Group) Qualified High Health Plan National QA2000-20 Benefit Year Individual Family (Amounts for Participating and s services are separated in calculating when
PLAN DESIGN AND BENEFITS Basic HMO Copay Plan 1-10
 PLAN FEATURES Deductible (per calendar year) Member Coinsurance Not Applicable Not Applicable Out-of-Pocket Maximum $5,000 Individual (per calendar year) $10,000 Family Once the Family Out-of-Pocket Maximum
PLAN FEATURES Deductible (per calendar year) Member Coinsurance Not Applicable Not Applicable Out-of-Pocket Maximum $5,000 Individual (per calendar year) $10,000 Family Once the Family Out-of-Pocket Maximum
Aetna HealthFund Health Reimbursement Account Plan (Aetna HealthFund Open Access Managed Choice POS II )
 Health Fund The Health Fund amount reflected is on a per calendar year basis. If you do not use the entire fund by 12/31/2015, it will be moved into a Limited-Purpose Flexible Spending Account. Health
Health Fund The Health Fund amount reflected is on a per calendar year basis. If you do not use the entire fund by 12/31/2015, it will be moved into a Limited-Purpose Flexible Spending Account. Health
PLAN DESIGN AND BENEFITS Georgia 2-100 HNOption 13-1000-80
 Georgia Health Network Option (POS Open Access) PLAN DESIGN AND BENEFITS Georgia 2-100 HNOption 13-1000-80 PLAN FEATURES PARTICIPATING PROVIDERS NON-PARTICIPATING PROVIDERS Deductible (per calendar year)
Georgia Health Network Option (POS Open Access) PLAN DESIGN AND BENEFITS Georgia 2-100 HNOption 13-1000-80 PLAN FEATURES PARTICIPATING PROVIDERS NON-PARTICIPATING PROVIDERS Deductible (per calendar year)
PLAN DESIGN & BENEFITS - CONCENTRIC MODEL
 PLAN FEATURES Deductible (per calendar year) Rice University None Family Member Coinsurance Applies to all expenses unless otherwise stated. Payment Limit (per calendar year) $1,500 Individual $3,000 Family
PLAN FEATURES Deductible (per calendar year) Rice University None Family Member Coinsurance Applies to all expenses unless otherwise stated. Payment Limit (per calendar year) $1,500 Individual $3,000 Family
Schedule of Benefits for the MoDOT/MSHP Medical Plan Medicare ASO PPO 20088 Effective 1/1/2016
 Schedule of Benefits for the MoDOT/MSHP Medical Plan Medicare ASO PPO 20088 Effective 1/1/2016 This Schedule of Benefits summarizes your obligation towards the cost of certain covered services. Refer to
Schedule of Benefits for the MoDOT/MSHP Medical Plan Medicare ASO PPO 20088 Effective 1/1/2016 This Schedule of Benefits summarizes your obligation towards the cost of certain covered services. Refer to
$100 Individual. Deductible
 PLAN FEATURES Deductible $100 Individual (per calendar year) $200 Family Unless otherwise indicated, the deductible must be met prior to benefits being payable. Member cost sharing for certain services,
PLAN FEATURES Deductible $100 Individual (per calendar year) $200 Family Unless otherwise indicated, the deductible must be met prior to benefits being payable. Member cost sharing for certain services,
OverVIEW of Your Eligibility Class by determineing Benefits
 OVERVIEW OF YOUR BENEFITS IMPORTANT PHONE NUMBERS Benefit Fund s Member Services Department (646) 473-9200 For answers to questions about your eligibility or prescription drug benefit. You can also visit
OVERVIEW OF YOUR BENEFITS IMPORTANT PHONE NUMBERS Benefit Fund s Member Services Department (646) 473-9200 For answers to questions about your eligibility or prescription drug benefit. You can also visit
SPIN Effective Date: 01-01-2013 Aetna HealthFund Aetna Choice POS ll - ASC PLAN DESIGN & BENEFITS ADMINISTERED BY AETNA LIFE INSURANCE COMPANY
 HealthFund Amount $1,500 Employee $1,500 Employee + 1 Dependent $1,500 Employee + 2 Dependents $1,500 Family Amount contributed to Fund by employer Fund Coinsurance 100% Percentage at which Fund will reimburse
HealthFund Amount $1,500 Employee $1,500 Employee + 1 Dependent $1,500 Employee + 2 Dependents $1,500 Family Amount contributed to Fund by employer Fund Coinsurance 100% Percentage at which Fund will reimburse
IL Small Group PPO Aetna Life Insurance Company Plan Effective Date: 04/01/2009 PLAN DESIGN AND BENEFITS- PPO HSA HDHP $2,500 100/80 (04/09)
 PLAN FEATURES OUT-OF- Deductible (per calendar ) $2,500 Individual $5,000 Individual $5,000 Family $10,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
PLAN FEATURES OUT-OF- Deductible (per calendar ) $2,500 Individual $5,000 Individual $5,000 Family $10,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
20% 40% Individual Family
 PLAN FEATURES NON-* Deductible (per calendar year) $2,500 Individual $3,000 Individual $5,000 Family $6,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
PLAN FEATURES NON-* Deductible (per calendar year) $2,500 Individual $3,000 Individual $5,000 Family $6,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
Rice University Effective Date: 07-01-2014 Aetna Choice POS ll - ASC PLAN DESIGN & BENEFITS ADMINISTERED BY AETNA LIFE INSURANCE COMPANY PLAN FEATURES
 PLAN DESIGN & BENEFITS PLAN FEATURES NON- Deductible (per calendar year) None Individual $1,000 Individual None Family $3,000 Family All covered expenses, excluding prescription drugs, accumulate toward
PLAN DESIGN & BENEFITS PLAN FEATURES NON- Deductible (per calendar year) None Individual $1,000 Individual None Family $3,000 Family All covered expenses, excluding prescription drugs, accumulate toward
SUMMARY OF BENEFITS. Cigna Health and Life Insurance Co. Laramie County School District 2 Open Access Plus Base - Effective 7/1/2015
 SUMMARY OF BENEFITS Cigna Health and Life Insurance Co. Laramie County School District 2 Open Access Plus Base - Effective General Services In-Network Out-of-Network Physician office visit Urgent care
SUMMARY OF BENEFITS Cigna Health and Life Insurance Co. Laramie County School District 2 Open Access Plus Base - Effective General Services In-Network Out-of-Network Physician office visit Urgent care
Greater Tompkins County Municipal Health Insurance Consortium
 WHO IS COVERED Requires both Medicare A & B enrollment. Type of Coverage Offered Single only Single only MEDICAL NECESSITY Pre-Certification Requirement None None Medical Benefit Management Program Not
WHO IS COVERED Requires both Medicare A & B enrollment. Type of Coverage Offered Single only Single only MEDICAL NECESSITY Pre-Certification Requirement None None Medical Benefit Management Program Not
Services and supplies required by Health Care Reform Age and frequency guidelines apply to covered preventive care Not subject to deductible if PPO
 Page 1 of 5 Individual Deductible Calendar year $400 COMBINED Individual / Family OOP Calendar year $4,800 Individual $12,700 per family UNLIMITED Annual Maximum July 1 st to June 30 th UNLIMITED UNLIMITED
Page 1 of 5 Individual Deductible Calendar year $400 COMBINED Individual / Family OOP Calendar year $4,800 Individual $12,700 per family UNLIMITED Annual Maximum July 1 st to June 30 th UNLIMITED UNLIMITED
SUMMARY OF BENEFITS. Cigna Health and Life Insurance Co. Grand County Open Access Plus Effective 1/1/2015
 SUMMARY OF BENEFITS Cigna Health and Life Insurance Co. Grand County Open Access Plus Effective General Services In-Network Out-of-Network Primary care physician You pay $25 copay per visit Physician office
SUMMARY OF BENEFITS Cigna Health and Life Insurance Co. Grand County Open Access Plus Effective General Services In-Network Out-of-Network Primary care physician You pay $25 copay per visit Physician office
$20 office visit copay; deductible 20%; after deductible. $30 office visit copay; deductible Not Covered. $30 office visit copay; deductible waived
 PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $300 Individual $600 Individual $600 Family $1,200 Family All covered expenses, accumulate separately toward the preferred or non-preferred
PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $300 Individual $600 Individual $600 Family $1,200 Family All covered expenses, accumulate separately toward the preferred or non-preferred
California PCP Selected* Not Applicable
 PLAN FEATURES Deductible (per calendar ) Member Coinsurance * Not Applicable ** Not Applicable Copay Maximum (per calendar ) $3,000 per Individual $6,000 per Family All member copays accumulate toward
PLAN FEATURES Deductible (per calendar ) Member Coinsurance * Not Applicable ** Not Applicable Copay Maximum (per calendar ) $3,000 per Individual $6,000 per Family All member copays accumulate toward
Sherwin-Williams Medical, Prescription Drug and Dental Plans Plan Comparison Charts
 Sherwin-Williams Medical, Prescription Drug and Dental Plans Plan Comparison Charts You and Sherwin-Williams share the cost of certain benefits including medical and dental coverage and you have the opportunity
Sherwin-Williams Medical, Prescription Drug and Dental Plans Plan Comparison Charts You and Sherwin-Williams share the cost of certain benefits including medical and dental coverage and you have the opportunity
2015 Medical Plan Summary
 2015 Medical Plan Summary AVMED POS PLAN This Schedule of Benefits reflects the higher provider and prescription copayments for 2015. This is not a contract, it s a summary of the plan highlights and is
2015 Medical Plan Summary AVMED POS PLAN This Schedule of Benefits reflects the higher provider and prescription copayments for 2015. This is not a contract, it s a summary of the plan highlights and is
Medical plan options. Small Business Solutions. New York FOR BUSINESSES WITH 2 50 ELIGIBLE EMPLOYEES
 Medical plan options Small Business Solutions New York FOR BUSINESSES WITH 2 50 ELIGIBLE EMPLOYEES Health insurance plans are offered, underwritten or administered by Aetna Life Insurance Company. 14.02.929.1-NY
Medical plan options Small Business Solutions New York FOR BUSINESSES WITH 2 50 ELIGIBLE EMPLOYEES Health insurance plans are offered, underwritten or administered by Aetna Life Insurance Company. 14.02.929.1-NY
LOCKHEED MARTIN AERONAUTICS COMPANY PALMDALE 2011 IAM NEGOTIATIONS UNDER AGE 65 LM HEALTHWORKS SUMMARY
 Annual Deductibles, Out-of-Pocket Maximums, Lifetime Maximum Benefits Calendar Year Deductible Calendar Year Out-of- Pocket Maximum Lifetime Maximum Per Individual Physician Office Visits Primary Care
Annual Deductibles, Out-of-Pocket Maximums, Lifetime Maximum Benefits Calendar Year Deductible Calendar Year Out-of- Pocket Maximum Lifetime Maximum Per Individual Physician Office Visits Primary Care
The Deductible is applicable to all covered services except for flat dollar Copayment services.
 PRIORITY HEALTH www.priorityhealth.com/mpsers PRIORITYHMO SM PLUS PLAN MICHIGAN PUBLIC SCHOOL EMPLOYEES RETIREMENT SYSTEM (MPSERS) Effective January 1, 2016 through December 31, 2016 The HMO Plus plan
PRIORITY HEALTH www.priorityhealth.com/mpsers PRIORITYHMO SM PLUS PLAN MICHIGAN PUBLIC SCHOOL EMPLOYEES RETIREMENT SYSTEM (MPSERS) Effective January 1, 2016 through December 31, 2016 The HMO Plus plan
Benefit Summary - A, G, C, E, Y, J and M
 Benefit Summary - A, G, C, E, Y, J and M Benefit Year: Calendar Year Payment for Services Deductible Individual $600 $1,200 Family (Embedded*) $1,200 $2,400 Coinsurance (the percentage amount the Covered
Benefit Summary - A, G, C, E, Y, J and M Benefit Year: Calendar Year Payment for Services Deductible Individual $600 $1,200 Family (Embedded*) $1,200 $2,400 Coinsurance (the percentage amount the Covered
IN-NETWORK MEMBER PAYS. Out-of-Pocket Maximum (Includes a combination of deductible, copayments and coinsurance for health and pharmacy services)
 HMO-OA-CNT-30-45-500-500D-13 HMO Open Access Contract Year Plan Benefit Summary This is a brief summary of benefits. Refer to your Membership Agreement for complete details on benefits, conditions, limitations
HMO-OA-CNT-30-45-500-500D-13 HMO Open Access Contract Year Plan Benefit Summary This is a brief summary of benefits. Refer to your Membership Agreement for complete details on benefits, conditions, limitations
Plans. Who is eligible to enroll in the Plan? Blue Care Network (BCN) Health Alliance Plan (HAP) Health Plus. McLaren Health Plan
 Who is eligible to enroll in the Plan? All State of Michigan Employees who reside in the coverage area determined by zip code. All State of Michigan Employees who reside in the coverage area determined
Who is eligible to enroll in the Plan? All State of Michigan Employees who reside in the coverage area determined by zip code. All State of Michigan Employees who reside in the coverage area determined
$25 copay. One routine GYN visit and pap smear per 365 days. Direct access to participating providers.
 HMO-1 Primary Care Physician Visits Office Hours After-Hours/Home Specialty Care Office Visits Diagnostic OP Lab/X Ray Testing (at facility) with PCP referral. Diagnostic OP Lab/X Ray Testing (at specialist)
HMO-1 Primary Care Physician Visits Office Hours After-Hours/Home Specialty Care Office Visits Diagnostic OP Lab/X Ray Testing (at facility) with PCP referral. Diagnostic OP Lab/X Ray Testing (at specialist)
AVMED POS PLAN. Allergy Injections No charge 30% co-insurance after deductible Allergy Skin Testing $30 per visit 30% co-insurance after deductible
 AVMED POS PLAN This Schedule of Benefits reflects the higher provider and prescription copays for 2015. This is not a contract, it s a summary of the plan highlights and is subject to change. For specific
AVMED POS PLAN This Schedule of Benefits reflects the higher provider and prescription copays for 2015. This is not a contract, it s a summary of the plan highlights and is subject to change. For specific
UNIVERSITY OF VIRGINIA HEALTH PLAN 2015 SCHEDULE OF BENEFITS CHOICE HEALTH
 UNIVERSITY OF VIRGINIA HEALTH PLAN 2015 SCHEDULE OF BENEFITS CHOICE HEALTH SERVICES PROVIDED Direct Access through UVa Provider Network 1. PLAN COINSURANCE Applies to all expenses unless otherwise stated.
UNIVERSITY OF VIRGINIA HEALTH PLAN 2015 SCHEDULE OF BENEFITS CHOICE HEALTH SERVICES PROVIDED Direct Access through UVa Provider Network 1. PLAN COINSURANCE Applies to all expenses unless otherwise stated.
UnitedHealthcare Insurance Company of the River Valley Attachment D - Schedule of Benefits
 UnitedHealthcare Insurance Company of the River Valley Attachment D - Schedule of Benefits Please refer to your Provider Directory for listings of Participating Physicians, Hospitals, and other Providers.
UnitedHealthcare Insurance Company of the River Valley Attachment D - Schedule of Benefits Please refer to your Provider Directory for listings of Participating Physicians, Hospitals, and other Providers.
International Student Health Insurance Program (ISHIP) 2014-2015
 2014 2015 Medical Plan Summary for International Students Translation Services If you need an interpreter to help with oral translation services, you may contact the LifeWise Customer Service team at 1-800-971-1491
2014 2015 Medical Plan Summary for International Students Translation Services If you need an interpreter to help with oral translation services, you may contact the LifeWise Customer Service team at 1-800-971-1491
Dickinson Wright, PLLC 03956-006
 Dickinson Wright, PLLC 03956-006 Flexible Blue SM Plan 3 Medical Coverage with Preventive Care and Mammography Benefits Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only
Dickinson Wright, PLLC 03956-006 Flexible Blue SM Plan 3 Medical Coverage with Preventive Care and Mammography Benefits Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only
Member s responsibility (deductibles, copays, coinsurance and dollar maximums)
 MICHIGAN CATHOLIC CONFERENCE January 2015 Benefit Summary This is intended as an easy-to-read summary and provides only a general overview of your benefits. It is not a contract. Additional limitations
MICHIGAN CATHOLIC CONFERENCE January 2015 Benefit Summary This is intended as an easy-to-read summary and provides only a general overview of your benefits. It is not a contract. Additional limitations
2015 Medical Plan Options Comparison of Benefit Coverages
 Member services 1-866-641-1689 1-866-641-1689 1-866-641-1689 1-866-641-1689 1-866-641-1689 1-800-464-4000 Web site www.anthem.com/ca/llns/ www.anthem.com/ca/llns/ www.anthem.com/ca/llns/ www.anthem.com/ca/llns/
Member services 1-866-641-1689 1-866-641-1689 1-866-641-1689 1-866-641-1689 1-866-641-1689 1-800-464-4000 Web site www.anthem.com/ca/llns/ www.anthem.com/ca/llns/ www.anthem.com/ca/llns/ www.anthem.com/ca/llns/
Aetna Life Insurance Company
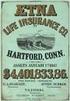 Aetna Life Insurance Company Hartford, Connecticut 06156 Amendment Policyholder: Group Policy No.: Effective Date: UNIVERSITY OF PENNSYLVANIA POSTDOCTORAL INSURANCE PLAN GP-861472 This Amendment is effective
Aetna Life Insurance Company Hartford, Connecticut 06156 Amendment Policyholder: Group Policy No.: Effective Date: UNIVERSITY OF PENNSYLVANIA POSTDOCTORAL INSURANCE PLAN GP-861472 This Amendment is effective
Orthodox HealthPlan Effective: 05-01-2015 Aetna HealthFund Open Choice (PPO)
 FUND FEATURES HealthFund Amount Orthodox HealthPlan $750 Employee $1,500 Family Amount contributed to the Fund by the employer Fund amount reflected is on a per calendar year basis. The fund received may
FUND FEATURES HealthFund Amount Orthodox HealthPlan $750 Employee $1,500 Family Amount contributed to the Fund by the employer Fund amount reflected is on a per calendar year basis. The fund received may
What is the overall deductible? Are there other deductibles for specific services?
 Small Group Agility MS200 Coverage Period: Beginning on or after 01/01/2015 This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or
Small Group Agility MS200 Coverage Period: Beginning on or after 01/01/2015 This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or
Small Business Solutions Medical Plan Options
 Small Business Solutions Medical Plan Options Indiana Choice. Simplicity. Affordability. 14.02.927.1-IN (10/04) AETNA SMALL GROUP MEDICAL PLANS AETNA CHOICE PPO PLAN OPTIONS Plan Option 1 Plan Option 2
Small Business Solutions Medical Plan Options Indiana Choice. Simplicity. Affordability. 14.02.927.1-IN (10/04) AETNA SMALL GROUP MEDICAL PLANS AETNA CHOICE PPO PLAN OPTIONS Plan Option 1 Plan Option 2
Important Questions Answers Why this Matters:
 This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at http://www.whyviva.com/memberaccess.aspx or by calling 1-800-294-7780.
This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at http://www.whyviva.com/memberaccess.aspx or by calling 1-800-294-7780.
CENTRAL MICHIGAN UNIVERSITY - Premier Plan (PPO1) 007000285-0002 0004 Effective Date: July 1, 2015 Benefits-at-a-Glance
 CENTRAL MICHIGAN UNIVERSITY - Premier Plan (PPO1) 007000285-0002 0004 Effective Date: July 1, 2015 Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only a general overview
CENTRAL MICHIGAN UNIVERSITY - Premier Plan (PPO1) 007000285-0002 0004 Effective Date: July 1, 2015 Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only a general overview
CSAC/EIA Health Small Group Access+ HMO 15-0 Inpatient Benefit Summary
 CSAC/EIA Health Small Group Access+ HMO 15-0 Inpatient Benefit Summary (Uniform Health Plan Benefits and Coverage Matrix) Blue Shield of California THIS MATRIX IS INTENDED TO BE USED TO HELP YOU COMPARE
CSAC/EIA Health Small Group Access+ HMO 15-0 Inpatient Benefit Summary (Uniform Health Plan Benefits and Coverage Matrix) Blue Shield of California THIS MATRIX IS INTENDED TO BE USED TO HELP YOU COMPARE
100% Percentage at which the Fund will reimburse Fund Administration
 FUND FEATURES HealthFund Amount $750 Employee $1,500 Family Amount contributed to the Fund by the employer Fund amount reflected is on a per calendar year basis, The fund received may be prorated based
FUND FEATURES HealthFund Amount $750 Employee $1,500 Family Amount contributed to the Fund by the employer Fund amount reflected is on a per calendar year basis, The fund received may be prorated based
Greater Tompkins County Municipal Health Insurance Consortium
 WHO IS COVERED Requires Covered Member to be Enrolled in Both Medicare Parts A & B Type of Coverage Offered Single only Single only MEDICAL NECESSITY Pre-Certification Requirement Not Applicable Not Applicable
WHO IS COVERED Requires Covered Member to be Enrolled in Both Medicare Parts A & B Type of Coverage Offered Single only Single only MEDICAL NECESSITY Pre-Certification Requirement Not Applicable Not Applicable
DRAKE UNIVERSITY HEALTH PLAN
 DRAKE UNIVERSITY HEALTH PLAN Effective Date: 1/1/2015 This is a general description of coverage. It is not a statement of contract. Actual coverage is subject to terms and the conditions specified in the
DRAKE UNIVERSITY HEALTH PLAN Effective Date: 1/1/2015 This is a general description of coverage. It is not a statement of contract. Actual coverage is subject to terms and the conditions specified in the
Sub Health Insurance Option Food Service - New Hire Memo
 MESQUITE ISD BENEFITS Sub Health Insurance Option Food Service - New Hire Memo Welcome to the Mesquite ISD family! If you are a new substitute, you must enroll in or decline medical coverage within 31
MESQUITE ISD BENEFITS Sub Health Insurance Option Food Service - New Hire Memo Welcome to the Mesquite ISD family! If you are a new substitute, you must enroll in or decline medical coverage within 31
Flexible Blue SM Plan 2 Medical Coverage with Flexible Blue SM RX Prescription Drugs Benefits-at-a-Glance for Western Michigan Health Insurance Pool
 Flexible Blue SM Plan 2 Medical Coverage with Flexible Blue SM RX Prescription Drugs Benefits-at-a-Glance for Western Michigan Health Insurance Pool The information in this document is based on BCBSM s
Flexible Blue SM Plan 2 Medical Coverage with Flexible Blue SM RX Prescription Drugs Benefits-at-a-Glance for Western Michigan Health Insurance Pool The information in this document is based on BCBSM s
Commercial. Individual & Family Plan. Health Net California Farm Bureau and PPO. Insurance Plans. Outline of Coverage and Exclusions and Limitations
 Commercial Individual & Family Plan Health Net California Farm Bureau and PPO Insurance Plans Outline of Coverage and Exclusions and Limitations Table of Contents Health Plans Outline of coverage 1 Read
Commercial Individual & Family Plan Health Net California Farm Bureau and PPO Insurance Plans Outline of Coverage and Exclusions and Limitations Table of Contents Health Plans Outline of coverage 1 Read
Covered 100% No deductible Not Applicable (exam, related tests and x-rays, immunizations, pap smears, mammography and screening tests)
 A AmeriHealth EPO Individual Summary of Benefits Value Network IHC EPO $30/50% Benefit Network Non network Benefit Period+ Calendar year Individual deductible $2,500 Family deductible $5,000 50% Individual
A AmeriHealth EPO Individual Summary of Benefits Value Network IHC EPO $30/50% Benefit Network Non network Benefit Period+ Calendar year Individual deductible $2,500 Family deductible $5,000 50% Individual
Group Insurance Plan of Benefits for New York University (Control # 620610) administered by Aetna International Effective Date: January 1, 2016
 Eligibility Provision Employee Regular full-time employees of New York University participating in this plan working a minimum of 25 hours per week. Dependent Wife or husband; same or opposite sex domestic
Eligibility Provision Employee Regular full-time employees of New York University participating in this plan working a minimum of 25 hours per week. Dependent Wife or husband; same or opposite sex domestic
CIGNA HEALTH AND LIFE INSURANCE COMPANY, a Cigna company (hereinafter called Cigna)
 Home Office: Bloomfield, Connecticut Mailing Address: Hartford, Connecticut 06152 CIGNA HEALTH AND LIFE INSURANCE COMPANY, a Cigna company (hereinafter called Cigna) CERTIFICATE RIDER No CR7SI006-1 Policyholder:
Home Office: Bloomfield, Connecticut Mailing Address: Hartford, Connecticut 06152 CIGNA HEALTH AND LIFE INSURANCE COMPANY, a Cigna company (hereinafter called Cigna) CERTIFICATE RIDER No CR7SI006-1 Policyholder:
Schedule of Benefits HARVARD PILGRIM LAHEY HEALTH VALUE HMO MASSACHUSETTS MEMBER COST SHARING
 Schedule of s HARVARD PILGRIM LAHEY HEALTH VALUE HMO MASSACHUSETTS ID: MD0000003378_ X Please Note: In this plan, Members have access to network benefits only from the providers in the Harvard Pilgrim-Lahey
Schedule of s HARVARD PILGRIM LAHEY HEALTH VALUE HMO MASSACHUSETTS ID: MD0000003378_ X Please Note: In this plan, Members have access to network benefits only from the providers in the Harvard Pilgrim-Lahey
PPO Benefit Summary $1, 000 Deductible Pete King Construction Company Group #19120 Effective 11/01/2011
 PPO Benefit Summary $1, 000 Deductible Pete King Construction Company Group #19120 Effective 11/01/2011 Calendar-Year Deductible Coinsurance This is a percentage members must pay for certain covered services
PPO Benefit Summary $1, 000 Deductible Pete King Construction Company Group #19120 Effective 11/01/2011 Calendar-Year Deductible Coinsurance This is a percentage members must pay for certain covered services
Medicare. Medicare Overview. Medicare Part D Prescription Plans. Medicare
 58 requires enrollment as soon as a retiree, spouse or dependent of a retiree is eligible for. Parts A & B MUST be elected. Overview There are three parts to : Hospital Insurance (also called Part A. Your
58 requires enrollment as soon as a retiree, spouse or dependent of a retiree is eligible for. Parts A & B MUST be elected. Overview There are three parts to : Hospital Insurance (also called Part A. Your
Summary Table of Benefits Select Medicare Supplement Plan
 2016 EXCLUSIVE CARE SUMMARY OF COVERED BENEFITS Select Medicare Eligible Supplement Plan Summary Table of Benefits Select Medicare Supplement Plan PLAN REIMBURSEMENT METHOD DEDUCTIBLE - Individual Medicare
2016 EXCLUSIVE CARE SUMMARY OF COVERED BENEFITS Select Medicare Eligible Supplement Plan Summary Table of Benefits Select Medicare Supplement Plan PLAN REIMBURSEMENT METHOD DEDUCTIBLE - Individual Medicare
Nationwide Life Insurance Co.: University of Phoenix NJ Coverage Period: 9/24/13-8/23/14
 This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.chpstudent.com or by calling 1-800-633-7867. Important
This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.chpstudent.com or by calling 1-800-633-7867. Important
The State Health Benefits Program Plan
 State of New Jersey Department of the Treasury Division of Pensions and Benefits STATE HEALTH BENEFITS PROGRAM PLAN COMPARISON SUMMARY FOR STATE EMPLOYEES EFFECTIVE APRIL 1, 2008 (March 29, 2008 for State
State of New Jersey Department of the Treasury Division of Pensions and Benefits STATE HEALTH BENEFITS PROGRAM PLAN COMPARISON SUMMARY FOR STATE EMPLOYEES EFFECTIVE APRIL 1, 2008 (March 29, 2008 for State
Important Questions Answers Why this Matters:
 This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.anthem.com or by calling 1-877-453-5645. Important Questions
This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy or plan document at www.anthem.com or by calling 1-877-453-5645. Important Questions
