AETNA HEALTH INC. (Arizona) CERTIFICATE OF COVERAGE
|
|
|
- Gwenda Walsh
- 9 years ago
- Views:
Transcription
1 AETNA HEALTH INC. (Arizona) CERTIFICATE OF COVERAGE Plan Name: AZ Silver HNOption /50 AZO This Certificate of Coverage ("Certificate") is part of the Group Agreement ("Group Agreement") between Aetna Health Inc., hereinafter referred to as Aetna, and the Contract Holder. The Group Agreement determines the terms and conditions of coverage. The Certificate describes covered health care benefits. Provisions of this Certificate include the Schedule of Benefits, and any amendments, endorsements, inserts, or attachments. Amendments, endorsements, inserts, or attachments may be delivered with the Certificate or added thereafter. Coverage is not provided for any services received before coverage starts or after coverage ends, except as shown in the Continuation section of this Certificate. Certain words have specific meanings when used in this Certificate. The defined terms appear in bold type with initial capital letters. The definitions of those terms are found in the Definitions section of this Certificate. This Certificate is not in lieu of insurance for Workers Compensation. This Certificate is governed by applicable federal law and the laws of Arizona. Coverage under this plan is non-occupational. Only non-occupational injuries and non-occupational illnesses are covered under this plan. If you are an owner of the company that applied for coverage under this plan and no other sources of coverage or reimbursement are available to you for the services or supplies, then you will also be covered for occupational injuries and occupational illnesses. Other sources of coverage or reimbursement may include workers compensation, or an occupational illness or similar program under local, state or federal law. A source of coverage or reimbursement will be considered available to you even if you waived your right to payment from that source. If you are also covered under a workers compensation law or similar law, and submit proof that you are not covered for a particular illness or injury under such law, that illness or injury will be considered non-occupational regardless of cause. READ THIS ENTIRE CERTIFICATE CAREFULLY. IT DESCRIBES THE RIGHTS AND OBLIGATIONS OF MEMBERS AND AETNA. IT IS THE CONTRACT HOLDER S AND THE MEMBER'S RESPONSIBILITY TO UNDERSTAND THE TERMS AND CONDITIONS IN THIS CERTIFICATE. IN SOME CIRCUMSTANCES, CERTAIN MEDICAL SERVICES ARE NOT COVERED OR MAY REQUIRE PRECERTIFICATION BY AETNA. NO SERVICES ARE COVERED UNDER THIS CERTIFICATE IN THE ABSENCE OF PAYMENT OF CURRENT PREMIUMS SUBJECT TO THE GRACE PERIOD AND THE PREMIUMS SECTION OF THE GROUP AGREEMENT. THIS CERTIFICATE APPLIES TO COVERAGE ONLY AND DOES NOT RESTRICT A MEMBER S ABILITY TO RECEIVE HEALTH CARE SERVICES THAT ARE NOT, OR MIGHT NOT BE, COVERED BENEFITS UNDER THIS CERTIFICATE. HI HMO-HNOSG2016COC 04 1 SG Off Exchange
2 PARTICIPATING PROVIDERS, NON-PARTICIPATING PROVIDERS, INSTITUTIONS, FACILITIES OR AGENCIES ARE NEITHER AGENTS NOR EMPLOYEES OF AETNA. Important Unless otherwise specifically provided, no Member has the right to receive the benefits of this plan for health care services or supplies furnished following termination of coverage. Benefits of this plan are available only for services or supplies furnished during the term the coverage is in effect and while the individual claiming the benefits is actually covered by the Group Agreement. Benefits may be modified during the term of this plan as specifically provided under the terms of the Group Agreement or upon renewal. If benefits are modified, the revised benefits (including any reduction in benefits or elimination of benefits) apply for services or supplies furnished on or after the effective date of the modification. Aetna will provide 60 day advance notice to the Member before the effective date of any material modification including changes in preventative benefits. There is no vested right to receive the benefits of the Group Agreement. HI HMO-HNOSG2016COC 04 2 SG Off Exchange
3 TABLE OF CONTENTS Section Page Aetna Procedure 4 Eligibility and Enrollment 7 Covered Benefits 12 Exclusions and Limitations 52 Termination of Coverage 74 Continuation 75 Claim Procedures/Complaints and Appeals 78 /Dispute Resolution Coordination of Benefits 85 Right of Recovery 90 Responsibility of Members 91 General Provisions 92 Definitions 97 HI HMO-HNOSG2016COC 04 3 SG Off Exchange
4 AETNA PROCEDURE Selecting a Participating Primary Care Physician At the time of enrollment, each Member may choose to select a Participating Primary Care Physician (PCP) from Aetna s Directory of Participating Providers to access Covered Benefits as described in this Certificate. The choice of a PCP is made solely by the Member. If the Member is a minor or otherwise incapable of selecting a PCP, the Subscriber should select a PCP on the Member s behalf. If the Member does not select a PCP, Aetna may choose one for you, in which case the Member will be notified of the PCP s name, address and telephone number. The Primary Care Physician The PCP coordinates a Member's medical care, as appropriate, either by providing treatment or may direct the Member to another Participating Provider. The PCP can also order lab tests and x-rays, prescribe medicines or therapies, and arrange hospitalization. The PCP provides services for the treatment of routine illnesses, injuries, well baby and preventive care services which do not require the services of a Specialist, and for non-office hour Urgent Care services under this plan. The Member s selected PCP or that PCP s covering Physician is required to be available 7 days a week, 24 hours a day for Urgent Care services. A Member will be subject to the PCP Copayment listed on the Schedule of Benefits when a Member obtains Covered Benefits from any Participating PCP. Certain PCP offices are affiliated with integrated delivery systems or other provider groups (i.e., Independent Practice Associations and Physician-Hospital Organizations), and Members who select these PCPs will generally be referred to Specialists and Hospitals within that system or group. However, if the group does not include a Provider qualified to meet the Member s medical needs, the Member may request to have services provided by nonaffiliated Providers. If the Member s PCP performs, suggests, or recommends a Member for a course of treatment that includes services that are not Covered Benefits, the entire cost of any such non-covered services will be the Member s responsibility. Covered Benefits also include E-visits. Registration with an internet service vendor may be required. Information about Participating Providers who conduct E-visits may be found in the provider Directory, online in DocFind on or by calling the number on your Member identification card. HI HMO-HNOSG2016COC 04 4 SG Off Exchange
5 Availability of Providers Aetna cannot guarantee the availability or continued participation of a particular Provider. Either Aetna or any Participating Provider may terminate the Provider contract or limit the number of Members that will be accepted as patients. If the PCP initially selected cannot accept additional patients, the Member will be notified and given an opportunity to make another PCP selection. The Member must then cooperate with Aetna to select another PCP. If the Member does not select a PCP, Aetna may choose one for you, in which case the Member will be notified of the PCP s name, address and telephone number. Changing a PCP You may change your PCP at any time by calling Member Services at the toll-free telephone number listed on the Member s identification card or by written or electronic submission of the Aetna s change form. A Member may contact Aetna to request a change form or for assistance in completing that form. The change will become effective upon Aetna s receipt and approval of the request. Ongoing Reviews Aetna conducts ongoing reviews of those services and supplies which are recommended or provided by Health Professionals to determine whether such services and supplies are Covered Benefits under this Certificate. If Aetna determines that the recommended services and supplies are not Covered Benefits, the Member will be notified. If a Member wishes to appeal such determination, the Member may then contact Aetna to seek a review of the determination. Please refer to the Claim Procedures/Complaints and Appeals and External Review/Dispute Resolution section of this Certificate. Precertification Certain services and supplies under this Certificate may require precertification by Aetna to determine if they are Covered Benefits under this Certificate. Continuity of Care Existing Enrollees If your current Hospital or Physician does not have a contract with Aetna, coverage will be provided for new Members to continue an active, ongoing course of treatment with the Member s current health care Provider during a transitional period, upon Member s written request to Aetna, as follows: 1. For a Member with a life threatening disease or condition, the transitional period is 30 days after the date of the Participating Provider s termination date; or 2. For a Member who has entered the third trimester of pregnancy on the Participating Provider s termination date, the transitional period includes the delivery and any care up to six weeks after the delivery that is related to the delivery. Aetna will authorize the coverage for the transitional period only if the health care Provider agrees to the following in writing: HI HMO-HNOSG2016COC 04 5 SG Off Exchange
6 1. to accept Aetna s normal reimbursement rates for similar services; 2. to adhere to Aetna s quality standards and to provide medical information related to such care; and 3. to adhere to Aetna s policies and procedures. This provision shall not be construed to require Aetna to provide coverage for benefits not otherwise covered under this Certificate. New Enrollees If your current Hospital or Physician does not have a contract with Aetna, coverage will be provided for new Members to continue an active, ongoing course of treatment with the Member s current health care Provider during a transitional period, upon Member s written request to Aetna, as follows: 1. For a Member with a life threatening disease or condition on their effective date, the transitional period is 30 days after the Member s effective date of coverage; or 2. For a Member who has entered the third trimester of pregnancy on their effective date, the transitional period includes the delivery and any care up to 6 weeks after the delivery that is related to the delivery. HI HMO-HNOSG2016COC 04 6 SG Off Exchange
7 ELIGIBILITY AND ENROLLMENT Eligibility Subscriber To be eligible to enroll as a Subscriber, an individual must: Meet all applicable eligibility requirements agreed upon by the Contract Holder and Aetna; and Live or work in the Service Area Determining if You Are in an Eligible Class You are in an eligible class if you are a regular full-time employee, as defined by your employer. Determining When You Become Eligible You become eligible for the plan on your eligibility date, which is determined as follows. On the Effective Date of the Plan If you are in an Eligible Class on the effective date of your plan, your Eligibility Date is the effective date of this Plan or, if later, the date you complete the period of continuous service required by your employer. Your employer determines the criteria that is used to define the Eligible Class for coverage under this Certificate. Such criteria are based solely upon conditions related to your employment. See your employer for details. After the Effective Date of the Plan If you are in an Eligible Class on the date of hire, your Eligibility Date is the effective date of this Plan or, if later, the date you complete the period of continuous service required by your employer. Your employer determines the criteria that is used to define the Eligible Class for coverage under this Certificate. Such criteria are based solely upon conditions related to your employment. See your employer for details. Waiting Period Once you enter an eligible class, you will need to complete the waiting period before your coverage under this plan begins. Obtaining Coverage for Dependents To be eligible to enroll as a Covered Dependent, the Contract Holder must provide dependent coverage for Subscribers who are eligible and must be: Your legal spouse; or Your domestic partner who meets the rules set by your employer; and Your dependent children; and Dependent children of your domestic partner. HI HMO-HNOSG2016COC 04 7 SG Off Exchange
8 Coverage for Dependent Children To be eligible for coverage, a dependent child must be: Under 26years of age. Covered Benefits for a Covered Dependent who is not capable of self-support due to mental or physical incapacity will be continued past the maximum age for a child. An eligible dependent child includes: Your biological children. Your stepchildren. Your legally adopted children or children placed with you for adoption. Your foster children, including any children placed with you for adoption. Any children for whom you are responsible under court order. Your grandchildren in your court-ordered custody. Any child whose parent is your child and your child is covered as a dependent under this Plan. Any other child with whom you have a parent-child relationship. No individual may be covered both as an employee and dependent and no individual may be covered as a dependent of more than one employee. A Member who resides outside the Service Area is required to choose a PCP and return to the Service Area for Covered Benefits. The only services covered outside the Service Area are Emergency Services and Urgent Care. Coverage for a Domestic Partner Your domestic partner may be covered. To be eligible for coverage, you and your domestic partner will need to complete and sign a Declaration of Domestic Partnership which is acceptable to your Contract Holder. How And When To Enroll Enrollment Unless otherwise noted, an eligible individual and any eligible dependents may enroll in Aetna regardless of health status, age, or requirements for health services within 31 days from the eligibility date. Newly Eligible Individuals and Eligible Dependents An eligible individual and any eligible dependents may enroll within 31 days of the eligibility date. HI HMO-HNOSG2016COC 04 8 SG Off Exchange
9 Open Enrollment Period Eligible individuals or dependents who are eligible for enrollment but do not enroll as stated above, may be enrolled during any subsequent Open Enrollment Period upon submission of complete enrollment information and Premium payment to Aetna. Enrollment of Newly Eligible Dependents Newborn Children A newborn child is covered for 31 days from the date of birth. To continue coverage beyond this initial period, the child must be enrolled in Aetna within the initial 31 day period. If coverage does not require the payment of an additional Premium for a Covered Dependent, the Subscriber must still enroll the child within 31 days after the date of birth. The coverage for newly born, adopted children, and children placed for adoption consists of coverage of injury and sickness, including the necessary care and treatment of congenital defects and birth abnormalities, and within the limits of this Certificate. Coverage includes necessary transportation costs from place of birth to the nearest specialized Participating treatment center. Adopted Children A legally adopted child or a child for whom a Subscriber is a court appointed legal guardian, and who meets the definition of a Covered Dependent, will be treated as a dependent from the date of adoption or upon the date the child was placed for adoption with the Subscriber. Placed for adoption means the assumption and retention of a legal obligation for total or partial support of a child in anticipation of adoption of the child. The Subscriber must make a written request for coverage within 31 days of the date the child is adopted or placed with the Subscriber for adoption. To continue coverage beyond this initial period, the child must be enrolled within the initial 31-day period. If coverage does not require the payment of an additional Premium for a Covered Dependent, the Subscriber should still enroll the child within 31 days after the date of adoption. Special Rules Which Apply to Children Qualified Medical Child Support Order Coverage is available for a dependent child not residing with a Subscriber and who resides outside the Service Area, if there is a qualified medical child support order requiring the Subscriber to provide dependent health coverage for a non-resident child. The child must meet the definition of a Covered Dependent, and the Subscriber must make a written request for coverage within 31 days of the court order. Handicapped Children Coverage is available for a child who has reached the maximum dependent age for a child under this Certificate and is chiefly dependent upon the Subscriber for support and maintenance and is incapable of self-support due to mental or physical incapacity. The incapacity must have commenced prior to the age the dependent would have lost eligibility. In order to continue coverage for a handicapped child, the Subscriber must provide evidence of the child's incapacity and dependency to Aetna within 31 days of the date the child's coverage would otherwise terminate. Proof of continued incapacity, including a medical examination, must be submitted to Aetna as requested, but not more frequently than annually beginning after the 2 year period following the child's attainment of the age specified on the Schedule of Benefits. This eligibility provision will no longer apply on the date the dependent s incapacity ends. HI HMO-HNOSG2016COC 04 9 SG Off Exchange
10 Notification of Change in Status It shall be a Member s responsibility to notify Aetna of any changes which affect the Member s coverage under this Certificate, unless a different notification process is agreed to between Aetna and Contract Holder. Such status changes include, but are not limited to, change of address, change of Covered Dependent status, and enrollment in Medicare or any other group health plan of any Member. Additionally, if requested, a Subscriber must provide to Aetna, within 31 days of the date of the request, evidence satisfactory to Aetna that a dependent meets the eligibility requirements described in this Certificate. Special Enrollment Period An eligible individual and eligible dependents may be enrolled during a Special Enrollment Periods. A Special Enrollment Period may apply when an eligible individual or eligible dependent loses other health coverage or when an eligible individual acquires a new eligible dependent through marriage, birth, adoption or placement for adoption. Special Enrollment Period for Certain Individuals Who Lose Other Health Coverage: An eligible individual or an eligible dependent may be enrolled during a Special Enrollment Period, if the following requirements, as applicable, are met: The eligible individual or the eligible dependent was covered under another group health plan or other health insurance coverage when initially eligible for coverage under Aetna; The eligible individual or eligible dependent previously declined coverage in writing under Aetna; The eligible individual or eligible dependent loses coverage under the other group health plan or other health insurance coverage for one of the following reasons: - The other group health coverage is COBRA continuation coverage under another plan, and the COBRA continuation coverage under that other plan has since been exhausted; - The other coverage is a group health plan or other health insurance coverage, and the other coverage has been terminated as a result of loss of eligibility for the coverage or employer contributions towards the other coverage have been terminated; or - The other health insurance coverage is Medicaid or an S-Chip plan and the eligible individual or eligible dependent no longer qualifies for such coverage. - Employer contributions toward that coverage have ended. - The employer s decision to stop offering the group health plan to the eligible class to which you belong. - COBRA coverage ends. Loss of eligibility includes the following: - A loss of coverage as a result of legal separation, divorce or death; - Termination of employment; - Reduction in the number of hours of employment; - Any loss of eligibility after a period that is measured by reference to any of the foregoing; - Termination of Aetna coverage due to Member action- movement outside of the Aetna s service area; and also the termination of health coverage including Non-Aetna, due to plan termination. - Plan ceases to offer coverage to a group of similarly situated individuals; - Cessation of a dependent s status as an eligible dependent HI HMO-HNOSG2016COC SG Off Exchange
11 - Termination of benefit package Loss of eligibility does not include a loss due to failure of the individual or the participant to pay Premiums on a timely basis or due to termination of coverage for cause as referenced in the Termination of Coverage section of this Certificate. To be enrolled in Aetna during a Special Enrollment Period, the eligible individual or eligible dependent must enroll within: 60 days, beginning on the date of the eligible individual's or eligible dependent's loss of other group health plan or other health insurance coverage; or 60 days, beginning on the date the eligible individual or eligible dependent - Becomes eligible for premium assistance in connection with coverage under Aetna, or - Is no longer qualified for coverage under Medicaid or S-Chip. The Effective Date of Coverage will be the first day of the first calendar month following the date the completed request for enrollment is received. Special Enrollment Period When a New Eligible Dependent is Acquired: When a new eligible dependent is acquired through marriage, birth, adoption or placement for adoption, the new eligible dependent (and, if not otherwise enrolled, the eligible individual and other eligible dependents) may be enrolled during a special enrollment period. The special enrollment period is a period of 31 days, beginning on the date of the marriage, birth, adoption or placement for adoption (as the case may be). If a completed request for enrollment is made during that period, the Effective Date of Coverage will be: In the case of marriage, the first day of the first calendar month following the date the completed request for enrollment is received. In the case of a dependent s birth, adoption or placement for adoption, the date of such birth, adoption or placement for adoption. The eligible individual or the eligible dependent enrolling during a special enrollment period will not be subject to late enrollment provisions, if any, described in this Certificate. Effective Date of Coverage Coverage shall take effect at 12:01 a.m. on the Member s effective date. Coverage shall continue in effect from month to month subject to payment of Premiums made by the Contract Holder and subject to the Termination section of the Group Agreement, and the Termination of Coverage section of this Certificate. Hospital Confinement on Effective Date of Coverage If a Member is an inpatient in a Hospital on the Effective Date of Coverage, the Member will be covered as of that date. Such services are not covered if the Member is covered by another health plan on that date and the other health plan is responsible for the cost of the services. Aetna will not cover any service that is not a Covered Benefit under this Certificate. To be covered, the Member must utilize Participating Providers and is subject to all the terms and conditions of this Certificate. HI HMO-HNOSG2016COC SG Off Exchange
12 COVERED BENEFITS A Member shall be entitled to the Covered Benefits as specified below, in accordance with the terms and conditions of this Certificate. Unless specifically stated otherwise, in order for benefits to be covered, they must be Medically Necessary. For the purpose of coverage, Aetna may determine whether any benefit provided under the Certificate is Medically Necessary, and Aetna has the option to only authorize coverage for a Covered Benefit performed by a particular Provider. Preventive care, as described below, will be considered Medically Necessary. Important Note: You should review your Schedule of Benefits for the cost sharing that applies to the Covered Benefits in this section. This will help you become familiar with your payment responsibilities. Some Covered Benefits may have visit limits and maximums that apply to the service or supply. You should always review your Certificate and Schedule of Benefits together. ALL SERVICES ARE SUBJECT TO THE EXCLUSIONS AND LIMITATIONS DESCRIBED IN THIS CERTIFICATE. To be Medically Necessary, the service or supply must: Be care or treatment as likely to produce a significant positive outcome as, and no more likely to produce a negative outcome than, any alternative service or supply, both as to the disease or injury involved and the Member's overall health condition; Be care or services related to diagnosis or treatment of an existing illness or injury, except for Preventive Care Benefits, as determined by Aetna; Be a diagnostic procedure, indicated by the health status of the Member and be as likely to result in information that could affect the course of treatment as, and no more likely to produce a negative outcome than, any alternative service or supply, both as to the disease or injury involved and the Member's overall health condition; Include only those services and supplies that cannot be safely and satisfactorily provided at home, in a Physician s or Dental Provider s office, on an outpatient basis, or in any facility other than a Hospital, when used in relation to inpatient Hospital services; and As to diagnosis, care and treatment be no more costly (taking into account all health expenses incurred in connection with the service or supply) than any equally effective service or supply in meeting the above tests. In determining if a service or supply is Medically Necessary, Aetna s Patient Management Medical Director or its Physician or Dentist designee will consider: Information provided on the Member's health status; Reports in peer reviewed medical literature; Reports and guidelines published by nationally recognized health care organizations that include supporting scientific data; HI HMO-HNOSG2016COC SG Off Exchange
13 Professional standards of safety and effectiveness which are generally recognized in the United States for diagnosis, care or treatment; The opinion of Health Professionals in the generally recognized health specialty involved; The opinion of the attending Physicians or Dental Providers, which have credence but do not overrule contrary opinions; and Any other relevant information brought to Aetna's attention. All Covered Benefits will be covered in accordance with the guidelines determined by Aetna. If a Member has questions regarding coverage under this Certificate, the Member may call the Member Services toll-free telephone number listed on the Member s identification card. THE MEMBER IS RESPONSIBLE FOR PAYMENT OF THE APPLICABLE COPAYMENTS AND DEDUCTIBLES LISTED ON THE SCHEDULE OF BENEFITS. EXCEPT FOR DIRECT ACCESS SPECIALIST BENEFITS OR IN A MEDICAL EMERGENCY OR URGENT CARE SITUATION AS DESCRIBED IN THIS CERTIFICATE, THE FOLLOWING BENEFITS MUST BE ACCESSED THROUGH THE PCP S OFFICE THAT IS SHOWN ON THE MEMBER S IDENTIFICATION CARD, OR ELSEWHERE. 1. Preventive Care and Wellness Benefits Preventive Care 1. The recommendations and guidelines of the: Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention; United States Preventive Services Task Force; Health Resources and Services Administration; and American Academy of Pediatrics/Bright Futures Guidelines for Children and Adolescents as referenced throughout this Preventive Care Benefit may be updated periodically. This Plan is subject to updated recommendations or guidelines that are issued by these organizations beginning on the first day of the plan year, one year after the recommendation or guideline is issued. 2. If any diagnostic x-rays, lab, or other tests or procedures are ordered, or given, in connection with any of the Preventive Care Benefits described below, those diagnostic x-rays, lab or other tests or procedures will not be covered as Preventive Care Benefits. Those that are Covered Benefits will be subject to the cost-sharing that applies to those specific services under this Plan. 3. Refer to the Schedule of Benefits for information about cost-sharing and maximums that apply to Preventive Care benefits. 4. Gender-Specific Preventive Care Benefits -- covered expenses include any recommended Preventive Care benefits described below that are determined by your provider to be medically necessary, regardless of the sex you were assigned at birth, your gender identity, or your recorded gender. HI HMO-HNOSG2016COC SG Off Exchange
14 5. To learn what frequency and age limits apply to routine physical exams and routine cancer screenings, contact your physician or contact Member Services by logging on to your Aetna Navigator secure member website at www. aetna.com or at the toll-free number on your ID card. This information can also be found at the website. Routine Physical Exam Benefit Covered Benefits include office visits to a Member's Participating Provider or Primary Care Physician (PCP) for routine physical exams, including routine vision and hearing screenings given as part of the routine physical exam. A routine exam is a medical exam given by a Participating Provider or PCP for a reason other than to diagnose or treat a suspected or identified illness or injury, and also includes: Evidence-based items that have in effect a rating of A or B in the current recommendations of the United States Preventive Services Task Force; Services as recommended in the American Academy of Pediatrics/Bright Futures/Health Resources and Services Administration guidelines for children and adolescents. For females, screenings and counseling services as provided for in the comprehensive guidelines recommended by the Health Resources and Services Administration. These services may include but are not limited to: - Screening and counseling services, such as those on: - Interpersonal and domestic violence; - Sexually transmitted diseases; and - Human Immune Deficiency Virus (HIV) infections. - Screening for gestational diabetes. - High risk Human Papillomavirus (HPV) DNA testing for women age 30 and older. X-rays, lab and other tests given in connection with the exam. For covered newborns, an initial Hospital checkup. Benefits for the routine physical exam services above may be subject to visit maximums as shown in the Schedule of Benefits. For details on the frequency and age limits that apply to Routine Physical Exam Benefit, Members may contact their Physician or Member Services by logging onto the Aetna Navigator website or calling the toll-free number on the back of the ID card. For a detailed listing of preventive care services described in this section refer to Benefit Limitations: Unless specified above, not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; Services which are for diagnosis or treatment of a suspected or identified illness or injury; Exams given while the Member is confined in a Hospital or other facility for medical care; Services not given by a Physician or under his or her direction; and Psychiatric, psychological, personality or emotional testing or exams. HI HMO-HNOSG2016COC SG Off Exchange
15 Preventive Care Immunizations Benefit Covered Benefits include: Immunizations for infectious diseases; and The materials for administration of immunizations; provided by a Member's Participating Provider or PCP or a facility. The immunizations must be recommended by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention. Specifically, the following immunizations are covered for adults at the recommended ages and populations: Hepatitis A, Hepatitis B, Herpes Zoster, Human Papillomavirus, Influenza (flu shot), Measles, Mumps, Rubella, Meningococcal, Pneumococcal, Tetanus, Diphtheria, Pertussis, and Varicella. Specifically, the following immunizations are covered for children, from birth to age 18, at the recommended ages and populations: Diphtheria, Tetanus, Pertussis, Haemophilus Influenza type b, Hepatitis A, Hepatitis B, Human Papillomavirus, Inactivated Poliovirus, Influenza (flu shot), Measles, Mumps, Rubella, Meningococcal, Pneumococcal, Rotavirus, and Varicella. Benefit Limitations: Not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; and Immunizations that are not considered preventive care such as those required due to a Member's employment or travel. Well Woman Preventive Visits Benefit Covered Benefits include a routine well woman preventive exam office visit, including Pap smears, provided by a Member's PCP, Physician, obstetrician, or gynecologist in accordance with the recommendations by the Health Resources and Services Administration. A routine well woman preventive exam is a medical exam given by a Physician for a reason other than to diagnose or treat a suspected or identified illness or injury; and routine preventive care breast cancer genetic counseling and breast cancer (BRCA) gene blood testing. Covered Benefits include charges made by a Physician and lab for the BRCA gene blood test and charges made by a genetic counselor to interpret the test results and evaluate treatment. These benefits will be subject to any age; family history; and frequency guidelines that are: Evidence-based items or services that have in effect a rating of A or B in the recommendations of the United States Preventive Services Task Force; and Evidence-informed items or services provided in the comprehensive guidelines supported by the Health Resources and Services Administration. Benefits for the well woman preventive visit services above are subject to visit maximums as shown in the Schedule of Benefits. Benefit Limitations: Unless specified above, not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; HI HMO-HNOSG2016COC SG Off Exchange
16 Services which are for diagnosis or treatment of a suspected or identified illness or injury; Exams given while the Member is confined in a Hospital or other facility for medical care; Services not given by a Physician or under his or her direction; and Psychiatric, psychological, personality or emotional testing or exams; and Services and supplies furnished by an out-of-network Provider. Screening and Counseling Services Benefit Covered Benefits include the following services provided by a Member's PCP or Physician, as applicable, in an individual or group setting: Obesity and Healthy Diet Counseling Benefit Covered Benefits include screening and counseling services to aid in weight reduction due to obesity. Coverage includes: Preventive counseling visits and/or risk factor reduction intervention; Nutritional counseling; and Healthy diet counseling visits provided in connection with Hyperlipidemia (high cholesterol) and other known risk factors for cardiovascular and diet-related chronic disease. Benefits for the screening and counseling services above are subject to the visit maximums as shown in the Schedule of Benefits. Misuse of Alcohol and/or Drugs Benefit Covered Benefits include screening and counseling services to aid in the prevention or reduction of the use of an alcohol agent or controlled substance. Coverage includes preventive counseling visits, risk factor reduction intervention and a structured assessment. Benefits for the screening and counseling services above are subject to visit maximums as shown later in this amendment. Use of Tobacco Products Benefit Covered Benefits include screening and counseling services to aid in the cessation of the use of tobacco products. Coverage includes: Preventive counseling visits; Treatment visits; and Class visits; to aid in the cessation of the use of tobacco products. Tobacco product means a substance containing tobacco or nicotine including: Cigarettes; Cigars; Smoking tobacco; Snuff; HI HMO-HNOSG2016COC SG Off Exchange
17 Smokeless tobacco; and Candy-like products that contain tobacco. Benefits for the screening and counseling services above are subject to visit maximums as shown in the Schedule of Benefits. Sexually Transmitted Infection Counseling Covered Benefits include the counseling services to help you prevent or reduce sexually transmitted infections. Genetic Risk Counseling for Breast and Ovarian Cancer Covered Benefits include the counseling and evaluation services to help you assess whether or not you are at risk of breast and ovarian cancer. Benefit Limitations: Unless specified above, not covered under this benefit are services which are covered to any extent under any other part of this Certificate. Tobacco Cessation Prescription and Over-the-Counter Drugs Covered Benefits include FDA-approved prescription drugs and over-the-counter (OTC) drugs to help stop the use of tobacco products, when prescribed by a prescriber and the prescription is submitted to the pharmacist for processing. Routine Cancer Screenings Benefit Covered Benefits include, but are not limited to, the following routine cancer screenings: One baseline mammogram for a woman age 35 to 39; One annual mammogram for a woman age 40 and over; Fecal occult blood tests; Digital rectal exams; Prostate specific antigen (PSA) tests; Sigmoidoscopies; Double contrast barium enema (DCBE); and Colonoscopies; (removal of polyps performed during a screening procedure is a Covered Benefit); and Lung cancer screenings. These benefits will be subject to any age, family history and frequency guidelines that are: Evidence-based items or services that have in effect a rating of A or B in the recommendations of the United States Preventive Services Task Force; and Evidence-informed items or services provided in the comprehensive guidelines supported by the Health Resources and Services Administration. For details on the frequency and age limits that apply to Routine Cancer Screenings Benefit, Members may contact their Physician or Member Services by logging onto the Aetna Navigator website or calling the toll-free number on the back of the ID card. HI HMO-HNOSG2016COC SG Off Exchange
18 As to routine gynecological exams performed as part of a routine cancer screening, the Member may go directly to a Participating obstetrician (OB), gynecologist (GYN), obstetrician/gynecologist (OB/GYN). See the Direct Access Specialist Benefits section of the Certificate, for a description of this provision. Benefit Limitations: Unless specified above, not covered under this benefit are services which are covered to any extent under any other part of this Plan. Prenatal Care Benefit Prenatal care will be covered as Preventive Care for services received by a pregnant female in a PCP, Physician's, OB-GYN, obstetrician's, or gynecologist's office but only to the extent described below. Coverage for prenatal care under this benefit is limited to pregnancy-related Physician office visits including the initial and subsequent history and physical exams of the pregnant woman (maternal weight, blood pressure, fetal heart rate check and fundal height). Benefit Limitations: Unless specified above, not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; and Services for maternity care (other than prenatal care as described above). Important Note: Refer to the: Maternity Care and Related Newborn Care Benefits section of the Certificate; and Prenatal Care Services, Delivery Services and Postpartum Care Services cost-sharing in the Schedule of Benefits; for more information on coverage for services related to maternity care under this Plan. Comprehensive Lactation Support and Counseling Services Benefit Covered Benefits include comprehensive lactation support (assistance and training in breast feeding) and counseling services provided to females during pregnancy or at any time following delivery, for breastfeeding by a certified lactation support provider. Covered Benefits also include the rental or purchase of breast feeding equipment as described below. Lactation support and lactation counseling services are Covered Benefits when provided in either a group or individual setting. Benefits for lactation counseling services are subject to the visit maximum shown later in this amendment. Breast Feeding Durable Medical Equipment Covered Benefits includes the rental or purchase of breast feeding Durable Medical Equipment for the purpose of lactation support (pumping and storage of breast milk) as follows. HI HMO-HNOSG2016COC SG Off Exchange
19 Breast Pumps Covered Benefits include the following: The rental of a hospital-grade electric pump for a newborn child when the newborn child is confined in a Hospital. The purchase of: - An electric breast pump (non-hospital grade),. A purchase will be covered once every three years; or - A manual breast pump. A purchase will be covered once per pregnancy. If a breast pump was purchased within the previous three year period, the purchase of another breast pump will not be covered until a three year period has elapsed from the last purchase. Breast Pump Supplies Coverage is limited to only one purchase per pregnancy in any year where a covered female would not qualify for the purchase of a new pump. Coverage for the purchase of breast pump equipment is limited to one item of equipment, for the same or similar purpose, and the accessories and supplies needed to operate the item. A Member is responsible for the entire cost of any additional pieces of the same or similar equipment purchased or rented for personal convenience or mobility. Aetna reserves the right to limit Covered Benefits to the most cost efficient and least restrictive level of service or item which can be safely and effectively provided. The decision to rent or purchase is at the discretion of Aetna. Benefit Limitations: Unless specified above, not covered under this benefit are services which are covered to any extent under any other part of this Plan. Family Planning Services - Female Contraceptives Benefit Important Note: For a list of the types of female contraceptives covered under this plan, refer to the section What the Pharmacy Benefit Covers and the Contraceptives benefit later in this Booklet-Certificate. For females with reproductive capacity, Covered Benefits include those services and supplies that are provided to a Member to prevent pregnancy. All contraceptive methods, services and supplies covered under this benefit must be approved by the U.S. Food and Drug Administration (FDA). Voluntary Sterilization Covered Benefits include charges billed separately by the provider for female voluntary sterilization procedures and related services and supplies including, but not limited to, tubal ligation and sterilization implants. Covered Benefits under this benefit would not include a voluntary sterilization procedure to the extent that the procedure was not billed separately by the provider or because it was not the primary purpose of the confinement. HI HMO-HNOSG2016COC SG Off Exchange
20 Important Reminder: Refer to the section Your Pharmacy Benefit later in this Certificate for additional coverage of female contraceptives. Benefit Limitations: Unless specified above, not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; Services and supplies incurred for an abortion; Services which are for the treatment of an identified illness or injury; Services that are not given by a Physician or under his or her direction; Psychiatric, psychological, personality or emotional testing or exams; Any contraceptive methods that are only "reviewed" by the FDA and not "approved" by the FDA; and The reversal of voluntary sterilization procedures, including any related follow-up care. 2. Physician and Other Health Professional Care Primary Care Physician Benefit Office visits during office hours. Home visits. After-hours PCP services. PCPs are required to provide or arrange for on-call coverage 24 hours a day, 7 days a week. If a Member becomes sick or is injured after the PCP's regular office hours, the Member should: - call the PCP's office; - identify himself or herself as a Member; and - follow the PCP's or covering Physician s instructions. If the Member's injury or illness is a Medical Emergency, the Member should follow the procedures outlined under the Emergency Care/Urgent Care Benefits section of this Certificate. Hospital visits. Immunizations for infectious disease, but not if solely for your employment or travel. Allergy testing and allergy injections. Charges made by the Physician for supplies, radiological services, x-rays, and tests provided by the Physician. Alternatives to Physicians Office Visits Walk-in Clinic Benefits Covered Benefits include charges made by walk-in clinics for: Unscheduled, non-emergency illnesses and injuries; The administration of certain immunizations administered within the scope of the clinic s license; and Individual screening and counseling services to aid you: HI HMO-HNOSG2016COC SG Off Exchange
21 - In weight reduction due to obesity; - In developing and maintaining a healthy diet; - To stop the use of tobacco products. Benefit Limitations: Unless specified above, not covered under this benefit are charges incurred for services and supplies furnished in a group setting for screening and counseling services Important Note: Not all services are available at all Walk-In Clinics. The types of services offered will vary by the provider and location of the clinic. For a complete description of the screening and counseling services provided on the use of tobacco products, healthy diet and to aid in weight reduction due to obesity, refer to the Preventive Care Benefits section in this Certificate and the Screening and Counseling Services benefit for a description of these services. These services may also be obtained from your PCP. E-Visits and Telemedicine Consultations Covered Benefits include charges made by your PCP or physician for a routine, non-emergency, medical consultation. You must make your E-visit or telemedicine appointment through an Aetna authorized internet service vendor. You may have to register with that internet service vendor. Information about providers who are signed up with an authorized vendor may be found in the provider Directory or online in DocFind on or by calling the number on your identification card. Specialist Physician Benefits Covered Benefits include outpatient and inpatient services. Member may request a second opinion regarding a proposed surgery or course of treatment recommended by Member's Participating Provider or a Specialist. Second opinions must be obtained by a Participating Provider and are subject to precertification. Covered Benefits also include E-visits. Registration with an internet service vendor may be required. Information about Participating Providers who conduct E-visits may be found in the provider Directory, online in DocFind on or by calling the number on your Member identification card. Important Reminder: For a description of the preventive care benefits covered under this Certificate, refer to the Preventive Care Benefits section in this Certificate. HI HMO-HNOSG2016COC SG Off Exchange
22 3. Hospital and Other Facility Care Hospital Benefit A Member is covered for services only at Participating Hospitals. All services are subject to precertification by Aetna. In the event that the Member elects to remain in the Hospital after the date that the Participating Provider and/or the Aetna Medical Director has determined and advised the Member that the Member no longer meets the criteria for continued inpatient confinement, the Member shall be fully responsible for direct payment to the Hospital Facility for such additional Hospital, Physician and other Provider services, and Aetna shall not be financially responsible for such additional services. Inpatient Hospital cardiac and pulmonary rehabilitation services are covered by Participating Providers and precertification by Aetna. Refer to the Short-Term Cardiac and Pulmonary Rehabilitation Therapy Services benefit for more information. Private hospital rooms and/or private duty nursing are only available during inpatient stays and determined to be medically appropriate by the Plan. Private duty nursing is available only in an inpatient setting when skilled nursing is not available from the facility. Skilled Nursing Facility Benefit A Member is covered for services only at Participating Skilled Nursing Facilities. All services are subject to precertification by Aetna. In the event that the Member elects to remain in the Skilled Nursing Facility after the date that the Participating Provider and/or the Aetna Medical Director has determined and advised the Member that the Member no longer meets the criteria for continued inpatient confinement, the Member shall be fully responsible for direct payment to the Skilled Nursing Facility for such additional Skilled Nursing Facility, Physician and other Provider services, and Aetna shall not be financially responsible for such additional services. Outpatient Surgery Benefit Coverage is provided for outpatient surgical services and supplies in connection with a covered surgical procedure when furnished by a Participating outpatient surgery center. All services and supplies are subject to precertification by Aetna. Home Health Care Benefit The following services are covered for a Homebound Member when provided by a Participating home health care agency. Precertification must be obtained from the Aetna by the Member s attending Participating Physician. Aetna shall not be required to provide home health benefits when Aetna determines the treatment setting is not appropriate, or when there is a more cost effective setting in which to provide covered health care services. Coverage for Home Health Services is not determined by the availability of caregivers to perform the services; the absence of a person to perform a non-skilled or Custodial Care service does not cause the service to become covered. If the Member is a minor or an adult who is dependent upon others for non-skilled care (e.g. bathing, eating, toileting), coverage for Home Health Services will only be provided during times when there is a family member or caregiver present in the home to meet the Member s non-skilled needs. HI HMO-HNOSG2016COC SG Off Exchange
23 Skilled Nursing services that require the medical training of and are provided by a licensed nursing professional are a covered benefit. Services must be provided during intermittent visits of 4 hours or less with a daily maximum of 3 visits. Up to 12 hours (3 visits) of continuous Skilled Nursing services per day within 30 days of an inpatient Hospital or Skilled Nursing Facility discharge may be covered, when all home health care criteria are met, for transition from the Hospital or Skilled Nursing Facility to home care. Services of a home health aide are covered only when they are provided in conjunction with Skilled Nursing services and directly support the Skilled Nursing. Services must be provided during intermittent visits of 4 hours or less with a daily maximum of 3 visits. Skilled behavioral health care services provided in the home by a behavioral health provider when ordered by a physician and directly related to an active treatment plan of care established by the physician. All of the following must be met: - The skilled behavioral health care is appropriate for the active treatment of a condition, illness or disease to avoid placing you at risk for serious complications. - The services are in lieu of a continued confinement in a hospital or residential treatment facility, or receiving outpatient services outside of the home. - You are homebound because of illness or injury. - The services provided are not primarily for comfort, convenience or custodial in nature. - The services are intermittent or hourly in nature. Medical social services are covered only when they are provided in conjunction with Skilled Nursing services and must be provided by a qualified social worker. Outpatient home health short-term physical, speech, or occupational therapy is covered when the above home health care criteria are met. Coverage is subject to the conditions and limits listed in the Short- Term Rehabilitation Therapy Services Benefit section of the Certificate and the Short-Term Rehabilitation and Habilitation Therapy Services Benefit section of the Schedule of Benefits. Covered Home Health Care benefits do not include charges for infusion therapy or applied behavior analysis. Hospice Benefit Hospice Care services for a terminally ill Member are covered when precertified by Aetna. Services may include home and Hospital visits by nurses and social workers; pain management and symptom control; instruction and supervision of a family Member; inpatient care; counseling and emotional support; and other home health benefits listed in the Home Health Benefits section of this Certificate. Benefit Limitations: Coverage is not provided for funeral arrangements, pastoral counseling, and financial or legal counseling. Homemaker or caretaker services, and any service not solely related to the care of the Member, including but not limited to, sitter or companion services for the Member or other Members of the family, transportation, house cleaning, and maintenance of the house are not covered. HI HMO-HNOSG2016COC SG Off Exchange
24 4. Emergency Care and Urgent Care Emergency Care/Urgent Care Benefit 1. Emergency Care: A Member is covered for Emergency Services, provided the service is a Covered Benefit, and Aetna's review determines that a Medical Emergency existed at the time medical attention was sought by the Member. The Copayment for an emergency room visit as described on the Schedule of Benefits will not apply if the Member is admitted into the Hospital. The Member will be reimbursed for the cost for Emergency Services rendered by a nonparticipating Provider located either within or outside the Aetna Service Area, for those expenses, less Copayments, which are incurred up to the time the Member is determined by Aetna and the attending Physician to be medically able to travel or to be transported to a Participating Provider. In the event that transportation is Medically Necessary, the Member will be reimbursed for the cost as determined by Aetna, minus any applicable Copayments. Reimbursement may be subject to payment by the Member of all Copayments which would have been required had similar benefits been provided during office hours. Medical transportation is covered during a Medical Emergency including Medically Necessary nonemergency transportation when approved by a Participating Provider. 2. Urgent Care: Urgent Care Within the Aetna Service Area. If the Member needs Urgent Care while within the Aetna Service Area, but the Member s illness, injury or condition is not serious enough to be a Medical Emergency, the Member should first seek care through the Member s Participating Provider. If the Member s Participating Provider is not reasonably available to provide services for the Member, the Member may access Urgent Care from a Participating Urgent Care Facility within the Aetna Service Area. Urgent Care Outside the Aetna Service Area. The Member will be covered for Urgent Care obtained from a Physician or licensed facility outside of the Aetna Service Area if the Member is temporarily absent from the Aetna Service Area and receipt of the health care service cannot be delayed until the Member returns to the Aetna Service Area. A Member is covered for any follow-up care. Follow-up care is any care directly related to the need for Emergency Services which is provided to a Member after the Medical Emergency or Urgent Care situation has terminated. All follow-up and continuing care must be provided or arranged by a Member s Participating Provider unless it can be shown that it was not reasonably possible to communicate with the Participating Provider within such time. The Member must follow this procedure, or the Member will be responsible for payment for all services received. HI HMO-HNOSG2016COC SG Off Exchange
25 5. Specific Conditions Maternity Care and Related Newborn Care Benefit Outpatient and inpatient pre-natal and postpartum care and obstetrical services provided by Participating Providers are a Covered Benefit. The Participating Provider is responsible for obtaining any required precertification for all non-routine obstetrical services from Aetna after the first prenatal visit. Coverage does not include routine maternity care (including delivery) received while outside the Service Area unless the Member receives precertification from Aetna. As with any other medical condition, Emergency Services are covered when Medically Necessary. As an exception to the Medically Necessary requirements of this Certificate, the following coverage is provided for a mother and newly born child: A minimum of 48 hours of inpatient care in a Participating Hospital following a vaginal delivery; A minimum of 96 hours of inpatient care in a Participating Hospital following a cesarean section; or A shorter Hospital stay, if requested by a mother, and if determined to be medically appropriate by the Participating Providers in consultation with the mother. If a Member requests a shorter Hospital stay, the Member will be covered for one home health care visit scheduled to occur within 24 hours of discharge. An additional visit will be covered when prescribed by the Participating Provider. This benefit is in addition to the home health maximum number of visits, if any, shown on the Schedule of Benefits. A Copayment will not apply for home health care visits. Coverage for a legally adopted child or for a child who has been placed for adoption with the Subscriber will include expenses incurred for services and supplies related to the cost of such child's birth, if: 1. the child is adopted within one year of birth; and 2. the Subscriber is legally obligated to pay the costs of the child's birth; and 3. the Subscriber has notified Aetna of his or her acceptability to adopt children pursuant to Arizona law regarding adoption, within 60 days after such acceptance or within 60 days after enrolling; whichever occurs last. Aetna coverage shall be secondary to and in excess of any other maternity benefits coverage of the natural mother. The Subscriber must notify Aetna regarding the existence and extent of any other such coverage of the natural mother. Within 31 days of Aetna's request, the Subscriber shall provide evidence satisfactory to Aetna that the child meets any of the above requirements. Reconstructive Breast Surgery Benefit Covered Benefits include reconstruction of the breast on which a mastectomy was performed, including an implant and areolar reconstruction. Also included is surgery on a healthy breast to make it symmetrical with the reconstructed breast and Medically Necessary physical therapy to treat complications of mastectomy, including lymphedema. HI HMO-HNOSG2016COC SG Off Exchange
26 Reconstructive or Cosmetic Surgery and Supplies Covered Benefits include charges made by a Physician, Hospital, or surgery center for reconstructive services and supplies, including: Surgery needed to improve a significant functional impairment of a body part. Surgery to correct the result of an accidental injury, including subsequent related or staged surgery, provided that the surgery occurs no more than 24 months after the original injury. For a covered child, the time period for coverage may be extended through age 18. Surgery to correct the result of an injury that occurred during a covered surgical procedure provided that the reconstructive surgery occurs no more than 24 months after the original injury. Important Note: Injuries that occur as a result of a medical (i.e., non-surgical) treatment are not considered accidental injuries, even if unplanned or unexpected. Surgery to correct a gross anatomical defect present at birth or appearing after birth (but not the result of an illness or injury) when - The defect results in severe facial disfigurement, or - The defect results in significant functional impairment and the surgery is needed to improve function Mental Disorders Benefit Covered Benefits include charges made by a Hospital, Psychiatric Hospital, Residential Treatment Facility or Behavioral Health Provider for the treatment of Mental Disorders as follows: Inpatient room and board at the semi-private room rate, and other services and supplies related to your condition that are provided during your stay in a Hospital, Psychiatric Hospital, or Residential Treatment Facility. Outpatient treatment received while not confined as an inpatient in a Hospital or Psychiatric Hospital or Residential Treatment Facility, including: - Partial Hospitalization Treatment (at least 4 hours, but less than 24 hours per day of clinical treatment) provided in a facility or program under the direction of a Physician. The facility or program does not make a room and board charge for the treatment. - Intensive Outpatient Program (at least 2 hours per day and at least 6 hours per week of clinical treatment) provided in a facility or program under the direction of a Physician. - Office visits to a Physician (such as a psychiatrist), psychologist, social worker, or licensed professional counselor, as well as other health professionals. Important Note: Not all types of services are covered. For example, educational services and certain types of therapies are not covered. See Exclusions section for more information. Inpatient and certain outpatient treatments must be precertified by Aetna. HI HMO-HNOSG2016COC SG Off Exchange
27 Substance Abuse Benefit Covered Benefits include charges made by a Hospital, Psychiatric Hospital, Residential Treatment Facility or Behavioral Health Provider for the treatment of Substance Abuse as follows: Inpatient room and board at the semi-private room rate and other services and supplies that are provided during your stay in a Hospital, Psychiatric Hospital or Residential Treatment Facility. Treatment of Substance Abuse in a general medical Hospital is only covered when you are admitted to the Hospital s separate Substance Abuse section (or unit) for treatment of medical complications of Substance Abuse. As used here, medical complications include, but are not limited to, Detoxification, electrolyte imbalances, malnutrition, cirrhosis of the liver, delirium tremens and hepatitis. Outpatient treatment received while not confined as an inpatient in a Hospital, Psychiatric Hospital or Residential Treatment Facility, including: - Partial Hospitalization Treatment (at least 4 hours, but less than 24 hours per day of clinical treatment) provided in a facility or program under the direction of a Physician. The facility or program does not make a room and board charge for the treatment. - Intensive Outpatient Program (at least 2 hours per day and at least 6 hours per week of clinical treatment) provided in a facility or program under the direction of a Physician. - Ambulatory detoxification Outpatient services that monitor withdrawal from alcohol or other Substance Abuse, including administration of medications. - Office visits to a Physician (such as a psychiatrist), psychologist, social worker, or licensed professional counselor, as well as other health care professional. Important Note: Not all types of services are covered. For example, educational services and certain types of therapies are not covered. See Exclusions section for more information. Inpatient and certain outpatient treatments must be precertification by Aetna. Autism Spectrum Disorders Benefit Autism Spectrum Disorder is defined in the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association. Covered Benefits include the services and supplies for the screening, diagnosis and treatment, (including behavioral therapy and Applied Behavioral Analysis), of Autism Spectrum Disorder. The services and supplies must be ordered by a Physician or Behavioral Health Provider. Coverage also includes early intensive behavioral interventions such as Applied Behavioral Analysis (ABA). Applied Behavioral Analysis is an educational service that is the process of applying interventions that: Systematically change behavior; and Are responsible for the observable improvement in behavior. Coverage for Applied Behavioral Analysis is shown in the Schedule of Benefits. HI HMO-HNOSG2016COC SG Off Exchange
28 Important: Applied Behavioral Analysis requires precertification by the Aetna and the Participating Provider is responsible for obtaining precertification. Diabetes Benefit Covered Benefits include charges for the following services, supplies, equipment, and training for the treatment of insulin- and non-insulin-dependent diabetes as well as gestational diabetes: Services and Supplies: - Foot care to minimize the risk of infection; - Insulin preparations; - Diabetic needles and syringes; - Diabetic test agents; - Lancets/lancing devices; - Prescribed oral medications whose primary purpose is to influence blood sugar; - Alcohol swabs; - Injectable glucagons; and - Glucagon emergency kits. Equipment: - External insulin pumps; and - Blood glucose monitors without special features unless required due to blindness. Training: - Self-management training provided by a licensed health care provider certified in diabetes self-management training. Basic Infertility Services Benefit Covered Benefits include only those Infertility services provided to a Member: a) by a Participating Provider to diagnose Infertility; and b) by a Participating Infertility Specialist to surgically treat the underlying cause of Infertility. Transplant Benefit Transplant Benefit Once it has been determined that a Member may require a Transplant, the Member or the Member s Physician must call the Aetna precertification department to discuss coordination of the Transplant process. Non-experimental or non-investigational Transplants coordinated by Aetna and performed at an Institute of Excellence, (IOE), are Covered Benefits. The IOE facility must be specifically approved and designated by Aetna to perform the Transplant required by the Member. Covered Benefits include the following when provided by an IOE. Inpatient and outpatient expenses directly related to a Transplant Occurrence. Charges made by a Physician or Transplant team. Compatibility testing of prospective organ donors who are immediate family members. For the purpose of this coverage, an immediate family member is defined as a first-degree biological relative. These are your: biological parent, sibling or child. Charges for activating the donor search process with national registries. HI HMO-HNOSG2016COC SG Off Exchange
29 Charges made by a Hospital or outpatient facility and/or Physician for the medical and surgical expenses of a live donor, but only to the extent not covered by another plan or program. Related supplies and services provided by the IOE facility during the Transplant Occurrence process. These services and supplies may include: physical, speech and occupational therapy; biomedicals and immunosuppressants; Home Health Services and home infusion services. Any Copayments or Coinsurance associated with Transplants are set forth in the Schedule of Benefits. Copayments or Coinsurance apply per Transplant Occurrence. One Transplant Occurrence includes the following four phases of Transplant care: Pre-Transplant Evaluation/Screening: Includes all Transplant-related professional and technical components required for assessment, evaluation and acceptance into a Transplant facility s Transplant program. Pre-Transplant/Candidacy Screening: Includes HLA typing of immediate family members. Transplant Event: Includes inpatient and outpatient services for all Transplant-related health services and supplies provided to a Member and donor during the one or more surgical procedures or medical therapies for a Transplant; prescription drugs provided during the Member s inpatient stay or outpatient visit(s), including bio-medical and immunosuppressant drugs; physical, speech or occupational therapy provided during the Member s inpatient stay or outpatient visit(s); cadaveric and live donor organ procurement. Follow-up Care: Includes Home Health Services; home infusion services; and Transplantrelated outpatient services rendered within 180 days from the date of the Transplant. For the purposes of this section, the following will be considered to be one Transplant Occurrence: Heart Lung Heart/ Lung Simultaneous Pancreas Kidney (SPK) Pancreas Kidney Liver Intestine Bone Marrow/Stem Cell Transplant Multiple organs replaced during one Transplant surgery Tandem Transplants (Stem Cell) Sequential Transplants Re-Transplant of same organ type within 180 days of the first Transplant Any other single organ Transplant, unless otherwise excluded under the coverage The following will be considered to be more than one Transplant Occurrence: Autologous Blood/Bone Marrow Transplant followed by Allogenic Blood/Bone Marrow Transplant (when not part of a tandem Transplant) Allogenic Blood/Bone Marrow Transplant followed by an Autologous Blood/Bone Marrow Transplant (when not part of a tandem Transplant) Re-Transplant after 180 days of the first Transplant HI HMO-HNOSG2016COC SG Off Exchange
30 Pancreas Transplant following a kidney Transplant A Transplant necessitated by an additional organ failure during the original Transplant surgery/process. More than one Transplant when not performed as part of a planned tandem or sequential Transplant, (e.g. a liver Transplant with subsequent heart Transplant). Travel and Lodging Expenses: Travel and Lodging Expenses are those expenses incurred by an IOE patient and a companion to travel between the IOE patient s home and the IOE facility, if the facility is located 60 miles or more from the IOE patient s home. Travel expenses include those incurred for round trip air, train, or bus travel, but only in coach class. You must be approved by Aetna for this program before you incur the expenses, otherwise you will not be reimbursed. The plan will reimburse you for some of the cost of your travel and lodging expenses up to the limits shown in the Schedule of Benefits. Your approval notification from Aetna will describe the process to follow for reimbursement. You will be required to submit proof of loss (receipts) to Aetna. For details about this program, contact Member Services at the toll-free number on your ID card. Benefit Limitations Unless specified above, not covered under this benefit are charges incurred for: Outpatient drugs including bio-medicals and immunosuppressants not expressly related to an outpatient transplant occurrence; Services that are covered under any other part of this plan; Services and supplies furnished to a donor when the recipient is not covered under this plan; Harvesting or storage of organs, without the expectation of immediate transplantation for an existing illness; Harvesting and/or storage of bone marrow, tissue or stem cells, without the expectation of transplantation within 12 months for an existing illness; Services and supplies furnished by a non-ioe facility. Cornea (Corneal Graft with Amniotic Membrane) or Cartilage (autologous chondrocyte or autologous osteochondral mosaicplasty) transplants, unless otherwise authorized by Aetna. Network of Transplant Specialist Facilities Through the IOE network, you will have access to a Participating Provider network that specializes in transplants. The IOE facility must be specifically approved and designated by Aetna to perform the procedure you require. Each facility in the IOE network has been selected to perform only certain types of transplants, based on quality of care and successful clinical outcomes. Oral and Maxillofacial Treatment (Mouth, Jaws and Teeth) Benefit Covered Benefits include charges made by a Physician, a Dentist and Hospital for: Non-surgical treatment of infections or diseases of the mouth, jaw joints or supporting tissues. Services and supplies for treatment of, or related conditions of, the teeth, mouth, jaws, jaw joints or supporting tissues, (this includes bones, muscles, and nerves), for surgery needed to: Treat a fracture, dislocation, or wound. Cut out cysts, tumors, or other diseased tissues. HI HMO-HNOSG2016COC SG Off Exchange
31 Cut into gums and tissues of the mouth. This is only covered when not done in connection with the removal, replacement or repair of teeth. Alter the jaw, jaw joints, or bite relationships by a cutting procedure when appliance therapy alone cannot result in functional improvement. Hospital services and supplies received for a stay required because of your condition. Dental work, surgery and orthodontic treatment needed to remove, repair, restore or reposition: Natural teeth damaged, lost, or removed; or Other body tissues of the mouth fractured or cut due to injury. Any such teeth must have been free from decay or in good repair, and are firmly attached to the jaw bone at the time of the injury. The treatment must begin within six months from the date of the injury. The treatment must be completed in the Calendar Year of the accident or in the next Calendar Year. If crowns, dentures, bridges, or in-mouth appliances are installed due to injury, covered benefits only include charges for: The first denture or fixed bridgework to replace lost teeth; The first crown needed to repair each damaged tooth; and An in-mouth appliance used in the first course of orthodontic treatment after the injury. 6. Specific Therapies and Tests Diagnostic and Preoperative Testing Diagnostic Complex Imaging Benefit Covered Benefits include charges made on an outpatient basis by a Physician, Hospital or a licensed imaging or radiological facility for complex imaging services to diagnose an illness or injury, including: C.A.T. scans; Magnetic Resonance Imaging (MRI); Nuclear medicine imaging, including Positron Emission Tomography (PET) Scans; and Any other outpatient diagnostic imaging service costing over $500. Complex Imaging Expenses for preoperative testing will be payable under this benefit. Benefit Limitations: The plan does not cover diagnostic complex imaging expenses under this part of the plan if such imaging expenses are covered under any other part of the plan. HI HMO-HNOSG2016COC SG Off Exchange
32 Outpatient Diagnostic Lab Work Covered Benefits include charges for lab services, and pathology and other tests provided to diagnose an illness or injury. The charges must be made by a Physician, Hospital or licensed radiological facility or lab. Important Reminder: Refer to the Schedule of Benefits for details about any cost-sharing or benefit maximums that may apply to outpatient diagnostic testing, lab services and radiological services. Outpatient Diagnostic Radiological Services Covered Benefits include charges for radiological services (other than complex imaging services), provided to diagnose an illness or injury. The services must be provided by a Physician, Hospital or licensed radiological facility. Benefit Limitations: The plan does not cover diagnostic complex imaging expenses under this part of the plan if such imaging expenses are covered under any other part of the plan. Outpatient Preoperative Testing Prior to a scheduled covered surgery, Covered Benefits include charges made for tests performed by a Hospital, Physician or licensed diagnostic laboratory provided the charges for the surgery are Covered Benefits and the tests are: Related to your surgery, and the surgery takes place in a Hospital; Completed within 14 days before your surgery; Performed on an outpatient basis; Covered if you were an inpatient in a Hospital; Not repeated in or by the Hospital where the surgery will be performed. Test results should appear in your medical record kept by the Hospital where the surgery is performed. Benefit Limitations: The plan does not cover diagnostic complex imaging expenses under this part of the plan if such imaging expenses are covered under any other part of the plan. If your tests indicate that surgery should not be performed because of your physical condition, the plan will pay for the tests, however surgery will not be covered. Important: Complex Imaging testing for preoperative testing is covered under the Diagnostic Complex Imaging Expense section. Separate cost sharing may apply. Refer to your Schedule of Benefits for information on cost sharing amounts for complex imaging. Clinical Trial Therapies (Experimental or Investigational) Covered Benefits include charges made by a Participating Provider for experimental or investigational drugs, devices, treatments or procedures under an approved clinical trial only when you have cancer or a terminal illness, and all of the following conditions are met: HI HMO-HNOSG2016COC SG Off Exchange
33 Standard therapies have not been effective or are inappropriate; Aetna determines based on published, peer-reviewed scientific evidence, that you may benefit from the treatment; and You are enrolled in an approved clinical trial that meets these criteria. An approved clinical trial is a clinical trial that meets these criteria; - The FDA has approved the drug, device, treatment, or procedure to be investigated or has granted it investigational new drug (IND) or group c/treatment IND status. This requirement does not apply to procedures and treatments that do not require FDA approval. - The clinical trial has been approved by an Institutional Review Board that will oversee the investigation; - The clinical trial is sponsored by the National Cancer Institute (NCI) or similar federal organization. - The trial conforms to standards of the NCI or other, applicable federal organization. - The clinical trial takes place at an NCI-designated cancer center or takes place at more than one institution. - You are treated in accordance with the protocols of that study. Clinical Trials (Routine Patient Costs) Covered Benefits include charges made by a Participating Provider for "routine patient costs" furnished in connection with participation in an "approved clinical trial as a qualified individual" for cancer or other life-threatening disease or condition, as those terms are defined in the federal Public Health Service Act, Section Coverage is limited to benefits for routine patient services provided within the network. Not covered under this Plan are: Services and supplies related to data collection and record-keeping that is solely needed due to the clinical trial (i.e. protocol-induced costs); Services and supplies provided by the trial sponsor without charge to the Member; and The experimental intervention itself (except medically necessary Category B investigational devices and promising experimental or investigational interventions for terminal illnesses in certain clinical trials in accordance with Aetna s claim policies). Important Notes: 1. Refer to the Schedule of Benefits for details about cost sharing and any benefit maximums that apply to the Clinical Trial benefit. 2. These Clinical Trial benefits are subject to all of the terms; conditions; provisions; limitations; and exclusions of this Plan including, but not limited to, any precertification and referral requirements. HI HMO-HNOSG2016COC SG Off Exchange
34 Outpatient Therapies Outpatient Infusion Therapy Benefit Covered Benefits include infusion therapy you receive in an outpatient setting. An outpatient setting includes but is not limited to: A free-standing outpatient facility The outpatient department of a Hospital A Physician in his/her office or in your home The list of preferred infusion locations can be found by contacting Member Services by logging onto your Aetna Navigator secure member website at or calling the number on the back of your ID card. Infusion therapy is the intravenous or continuous administration of medications or solutions that are medically necessary for your course of treatment. Charges for the following outpatient infusion therapy services and supplies are covered expenses: Pharmaceutical when administered in connection with infusion therapy and any medical supplies, equipment and nursing services required to support the infusion therapy; Professional services; Total parenteral nutrition (TPN); Chemotherapy; Drug therapy (includes antibiotic and antivirals); Pain management (narcotics); and Hydration therapy (includes fluids, electrolytes, and other additives). Benefit Limitations: Not included under this infusion therapy benefit are charges incurred for: Enteral nutrition; Blood transfusions and blood products; Insulin. Benefits payable for Infusion Therapy will not count toward any applicable Home Health Care maximums. Specialty care prescription drugs Covered expenses include specialty care prescription drugs when they are: Purchased by the Member s Provider, and Injected or infused by the Member s Provider in an outpatient setting such as: - A free-standing outpatient facility - The outpatient department of a Hospital - A Physician in his/her office - A home care Provider in the Member s home And, listed on our specialty care prescription drug list as covered under this certificate. Certain infused medications may be covered under the prescription drug plan. You can access the list of specialty care prescription drugs by contacting Member Services or by logging onto your Aetna Navigator secure member website at or calling the number on the back of your ID card to determine if coverage is under the prescription drug plan or this certificate. HI HMO-HNOSG2016COC SG Off Exchange
35 Chemotherapy Covered Benefits include charges for chemotherapy treatment. Coverage levels depend on where treatment is received. In most cases, chemotherapy is covered as outpatient care. Inpatient Hospitalization for chemotherapy is limited to the initial dose while Hospitalized for the diagnosis of cancer and when a Hospital stay is otherwise Medically Necessary based on your health status. Radiation Therapy Benefit Covered Benefits include charges for the treatment of illness by x-ray, gamma ray, accelerated particles, mesons, neutrons, radium or radioactive isotopes. Short-Term Cardiac and Pulmonary Rehabilitation Therapy Services Benefit Covered Benefits include short-term rehabilitation therapy services, as described below provided in a hospital, when prescribed by a Physician. All services are subject to precertification by Aetna. The services have to be performed by: A licensed or certified physical or occupational therapist; or A physician. The following are Covered Benefits for short term rehabilitation therapy services: Cardiac Rehabilitation Benefits Cardiac rehabilitation benefits are available as part of a Member s inpatient Hospital stay. A course of outpatient cardiac rehabilitation appropriate for your condition is covered when Medically Necessary for a cardiac condition that can be changed. The plan will cover charges in accordance with a treatment plan as determined by your risk level when recommended by a Physician. Pulmonary Rehabilitation Benefits Pulmonary rehabilitation benefits are available as part of a Member s inpatient Hospital stay. A course of outpatient pulmonary rehabilitation appropriate for your condition is covered when Medically Necessary for the treatment of reversible pulmonary disease states. Benefit Limitations Unless specifically covered above, not covered under this benefit are charges for: Any services which are covered expenses in whole or in part under any other group plan sponsored by an employer; Any services unless provided in accordance with a specific treatment plan; Services not performed by a physician or under the direct supervision of a physician; Services provided by a physician or physical or occupational therapist who resides in your home; or who is a member of your family, or a member of your spouse s family; or your domestic partner. Special education to instruct a person whose speech has been lost or impaired, to function without that ability. This includes lessons in sign language. HI HMO-HNOSG2016COC SG Off Exchange
36 Short-Term Rehabilitation Therapy Services Benefit Covered Benefits include charges for short-term rehabilitation therapy services, as described below, when prescribed by a Physician up to the benefit maximums listed on your Schedule of Benefits. The services have to be performed by: A licensed or certified physical, occupational or speech therapist; A Hospital, Skilled Nursing Facility, or Hospice Facility; A Home Health Care Agency; or A Physician. Short-term rehabilitation services have to follow a specific treatment plan, ordered by your physician, that: Details the treatment, and specifies frequency and duration, and Provides for ongoing reviews and is renewed only if continued therapy is appropriate. Allows therapy services, provided in your home, if you are homebound Cognitive Therapy, Physical Therapy, Occupational Therapy, Speech Therapy Rehabilitation Benefits Coverage is subject to the limits, if any, shown on the Schedule of Benefits. For inpatient rehabilitation benefits for the services listed below, refer to the Inpatient Hospital and Skilled Nursing Facility benefits provision under the Covered Benefits section of this Certificate. Physical therapy is covered for non-chronic conditions and acute illnesses and injuries provided the therapy is expected to: - Significantly improve, develop or restore physical functions lost; or - Improves any impaired function as a result of an acute illness, injury or surgical procedure. Physical therapy does not include educational training except for treatment of Autism Spectrum Disorders Occupational therapy, (except for vocational rehabilitation or employment counseling), is covered for non-chronic conditions and acute illnesses and injuries provided the therapy is expected to: - Significantly improve, develop or restore physical functions lost as a result of an acute illness, injury or surgical procedure; or - Improve an impaired function as a result of an acute illness, injury or surgical procedure; or - To relearn skills to significantly improve independence in the activities of daily living. Occupational therapy does not include educational training except for treatment of Autism Spectrum Disorders. Speech therapy is covered for non-chronic conditions and acute illnesses and injuries provided the therapy is expected to: - Significantly improve or Restore the speech function or correct a speech impairment resulting from illness, injury or surgical procedure; or; - Improve delays in speech function development as a result of a gross anatomical defect present at birth. Speech function is the ability to express thoughts, speak words and form sentences. Speech impairment is difficulty with expressing one s thoughts with spoken words. HI HMO-HNOSG2016COC SG Off Exchange
37 Cognitive rehabilitation is covered when the cognitive deficits have been acquired as a result of neurologic impairment due to trauma, stroke, or encephalopathy, and when the therapy is coordinated with Aetna as part of a treatment plan intended to restore previous cognitive function. Spinal Manipulation Care Benefit Services by a Participating Provider when Medically Necessary are covered. Services must be consistent with Aetna guidelines for spinal manipulation to correct a muscular skeletal problem which could be documented by diagnostic x-rays performed by an Aetna Participating radiologist. Habilitation Therapy Treatment Covered Benefits include habilitation therapy services your physician prescribes. The services have to be performed by: A licensed or certified physical, occupational or speech therapist A Hospital, Skilled Nursing Facility, or Hospice Facility A Home Health Care Agency A Physician Habilitation therapy services have to follow a specific treatment plan, ordered by your Physician, that: Details the treatment, and specifies frequency and duration, and Provides for ongoing reviews and is renewed only if continued therapy is appropriate. Allows therapy services, provided in your home, if you are homebound Outpatient Physical, Occupational, and Speech Therapy Covered Benefits under Habilitation Therapy Treatment include: Physical therapy, if it is expected to: - Develop any impaired function Occupational therapy (except for vocational rehabilitation or employment counseling), if it is expected to: - Develop any impaired function, or - Relearn skills to significantly develop your independence in the activities of daily living Speech therapy is covered provided the therapy is expected to: - Develop speech function as a result of delayed development (Speech function is the ability to express thoughts, speak words and form sentences). Short-Term Rehabilitation and Habilitation Therapy Services benefit limitations Unless specifically covered above, not covered under this benefit are charges for: Educational services for Down's Syndrome and Cerebral Palsy, for example, as they are considered both developmental and/or chronic in nature; Any services unless provided in accordance with a specific treatment plan; Services provided during a stay in a hospital, skilled nursing facility, or hospice facility except as stated above; Services not performed by a physician or under the direct supervision of a physician; Treatment covered as part of the Chiropractic Treatment. This applies whether or not benefits have been paid under that section; HI HMO-HNOSG2016COC SG Off Exchange
38 Special education to instruct a person whose speech has been lost or impaired, to function without that ability. This includes lessons in sign language. 7. Other Covered Benefits Acupuncture Benefit The plan covers charges made for acupuncture services provided by a physician, if the service is performed As a form of anesthesia in connection with a covered surgical procedure Administration of Blood and Blood Products Covered Benefits include the administration, cost, and processing of blood and blood products. Coverage also includes fees related to autologous blood donations. Ambulance Service Covered Benefits include charges made by a professional Ambulance, as follows: Ground Ambulance Covered Benefits include charges for transportation: To the first Hospital where treatment is given in a medical emergency. From one Hospital to another Hospital in a medical emergency when the first Hospital does not have the required services or facilities to treat your condition. From Hospital to home or to another facility when other means of transportation would be considered unsafe due to your medical condition. From home to Hospital for covered inpatient or outpatient treatment when other means of transportation would be considered unsafe due to your medical condition. When during a covered inpatient stay at a Hospital, Skilled Nursing Facility or acute rehabilitation Hospital, an Ambulance is required to safely and adequately transport you to or from inpatient or outpatient Medically Necessary treatment. Air or Water Ambulance Covered Benefits include charges for transportation to a Hospital by air or water Ambulance when: Ground Ambulance transportation is not available; and Your condition is unstable, and requires medical supervision and rapid transport; and In a medical emergency, transportation from one Hospital to another Hospital; when the first Hospital does not have the required services or facilities to treat your condition and you need to be transported to another Hospital; and the two conditions above are met. Benefit Limitations: Not covered under this benefit are charges incurred to transport you: If an Ambulance service is not required by your physical condition; or If the type of Ambulance service provided is not required for your physical condition; or By any form of transportation other than a professional Ambulance service. Non-emergency transport by fixed wing aircraft. HI HMO-HNOSG2016COC SG Off Exchange
39 Bariatric Surgery Covered Benefits for the treatment of morbid obesity include one bariatric surgical procedure including related outpatient services, within a two-year period, beginning with the date of the first bariatric surgical procedure, unless a multi-stage procedure is planned. Benefit Limitations: Unless specified above, not covered under this benefit are charges incurred for: Weight control services including open vertical banded gastroplasty, laparoscopic vertical banded gastroplasty, open sleeve gastrectomy, laparoscopic sleeve gastrectomy, open adjustable gastric banding, medical treatments, weight control/loss programs, dietary regimens and supplements, food or food supplements, appetite suppressants and other medications; exercise programs, exercise or other equipment; and other services and supplies that are primarily intended to control weight or treat obesity, including morbid obesity, or for the purpose of weight reduction, regardless of the existence of comorbid conditions; except as provided in the Certificate. Disposable Outpatient Supplies Covered benefits for medically necessary supplies, including ostomy supplies, which may be considered disposable are required for a Member in a course of treatment for a specific medical condition. Supplies must be obtained from a physician. Limitations Unless specified above, not covered under this benefit are charges incurred for: Over the counter supplies, such as band-aids and gauze. Durable Medical Equipment (DME) Benefit Durable Medical Equipment will be provided when precertified by Aetna. The wide variety of Durable Medical Equipment and continuing development of patient care equipment makes it impractical to provide a complete listing, therefore, the Aetna Medical Director has the authority to approve requests on a case-by-case basis. Covered Durable Medical Equipment includes those items covered by Medicare unless excluded in the Exclusions and Limitations section of this Certificate. Aetna reserves the right to provide the most cost efficient and least restrictive level of service or item which can be safely and effectively provided. The decision to rent or purchase is at the discretion of Aetna. Instruction and appropriate services required for the Member to properly use the item, such as attachment or insertion, is also covered upon precertification by Aetna. Replacement, repairs and maintenance are covered only if it is demonstrated to the Aetna that: It is needed due to a change in the Member s physical condition; or It is likely to cost less to buy a replacement than to repair the existing equipment or to rent like equipment. All maintenance and repairs that result from a misuse or abuse are a Member s responsibility. HI HMO-HNOSG2016COC SG Off Exchange
40 Family Planning Services - Other Covered Benefits include charges for the following family planning services, even though not provided to treat an illness or injury: Voluntary termination of pregnancy; and Voluntary sterilization for males. Benefit Limitations: Not covered under this benefit are charges incurred for: Reversal of voluntary sterilization procedures, for males and females including related follow-up care; Charges for services which are covered to any extent under any other part of this plan; and Charges incurred for family planning services while confined as an inpatient in a Hospital or other facility. Important Notes: Refer to the Schedule of Benefits for details about cost sharing and benefit maximums that apply to Family Planning Services - Other. For more information, see the sections on Family Planning Services - Female Contraceptives, Pregnancy Expenses and Treatment of Infertility in this Certificate. Hearing Aid Benefit Covered Benefits for hearing care includes charges for hearing exams, prescribed hearing aids and hearing aid expenses as described below. Hearing aid means: Any wearable, non-disposable instrument or device designed to aid or compensate for impaired human hearing; and Parts, attachments or accessories. Covered Benefits include the following: Charges for an audiometric hearing exam and evaluation for a hearing aid prescription performed by: - A Physician certified as an otolaryngologist or otologist; or - An audiologist who (1) is legally qualified in audiology; or (2) holds a certificate of Clinical Competence in Audiology from the American Speech and Hearing Association in the absence of any licensing requirements; and who performs the exam at the written direction of a legally qualified otolaryngologist or otologist. Charges for electronic hearing aids, installed in accordance with a Prescription written during a covered hearing exam; Any other related services necessary to access, select and adjust or fit a hearing aid. Covered Benefits for hearing aids will not include per 12 consecutive month period: Charges for more than one hearing aid per ear; and Charges in excess of any maximum amount shown on the Schedule of Benefits. HI HMO-HNOSG2016COC SG Off Exchange
41 Hearing Aids Alternate Treatment Rule Sometimes there are several types of hearing aids that can be used to treat a medical condition, all of which provide acceptable results. When alternate hearing aids can be used, the plan s coverage may be limited to the cost of the least expensive device that is: Customarily used nationwide for treatment, and Deemed by the medical profession to be appropriate for treatment of the condition in question. The device must meet broadly accepted standards of medical practice, taking into account your physical condition. You should review the differences in the cost of alternate treatment with your Physician. Of course, you and your Physician can still choose the more costly treatment method. You are responsible for any charges in excess of what the plan will cover. This Alternate Treatment Rule provision will not operate to deny benefits as mandated by any applicable state statute or regulation. Benefit Limitations: No benefits are payable under this benefit for charges incurred for: A service or supply which is received while the person is not a covered person under this Certificate; A replacement of: - A hearing aid installed within the prior 12 month period. Replacement parts or repairs for a hearing aid; Batteries or cords; A hearing aid that does not meet the specifications prescribed for correction of hearing loss: Any ear or hearing exam performed by a Physician who is not certified as an otolaryngologist or otologist; Any hearing aid furnished or ordered because of a hearing exam that was done before the date the person became covered under this Plan; Any hearing care service or supply which is a Covered Benefits in whole or in part under any other part of this Plan; Any hearing care service or supply which does not meet professionally accepted standards; Any hearing exam: - Required by an employer as a condition of employment; or - Which an employer is required to provide under a labor agreement; or - Which is required by any law of government. Hearing exams given during a stay in a Hospital or other facility, except those provided to newborns as part of the overall Hospital stay; and Any tests, appliances and devices for the improvement of hearing including hearing aid batteries and auxiliary equipment or to enhance other forms of communication to compensate for hearing loss or devices that simulate speech. HI HMO-HNOSG2016COC SG Off Exchange
42 Jaw Joint Disorder Treatment Covered Benefits include charges made by a Physician, Hospital or surgery center for the diagnosis and treatment of jaw joint disorder. A jaw joint disorder is defined as a painful condition: Temporomandibular joint dysfunction (TMJ) syndrome; or Involving the relationship between the jaw joint and related muscles and nerves such as myofacial pain dysfunction (MPD). resulting from accident, trauma, a congenital defect, a developmental defect, or a pathology. Covered benefits include: Surgical treatment of the jaw joint itself Treatment that is recognized by the medical or dental profession as effective and appropriate treatment for TMJ, including intra-oral splints that stabilize the jaw joint. Medical Foods to Treat Inherited Metabolic Disorders and Formulas to Treat Eosinophilic Gastrointestinal Disorders Covered Benefits include the expenses incurred for the purchase of: Medically Necessary Medical Foods used in the therapeutic treatment of Inherited Metabolic Disorders, including Modified Low Protein Foods and Metabolic Formula; and Medically Necessary amino acid-based formulas necessary for the treatment of Eosinophilic Gastrointestinal Disorders, when prescribed or ordered by the Member s Participating Physician. Any applicable Copayments are set forth in the Schedule of Benefits. Prosthetic Device Benefit The Member s initial provision and replacement of a prosthetic device that temporarily or permanently replaces all or part of an external body part lost or impaired as a result of disease or injury or congenital defects is covered, when such device is prescribed by a Participating Provider, administered through a Participating or designated prosthetic Provider and precertified by Aetna. Coverage includes repair and replacement when due to growth and development or a significant change in a Member s physical condition. Instruction and appropriate services required for the Member to properly use the item (such as attachment or insertion) are covered. Covered Benefits that are prosthetic devices include those items covered by Medicare unless excluded in the Exclusions and Limitations section of this Certificate. Aetna reserves the right to provide the most cost efficient and least restrictive level of service or item which can be safely and effectively provided. HI HMO-HNOSG2016COC SG Off Exchange
43 Benefit Limitations The plan will not cover expenses and charges for, or expenses related to: Orthopedic shoes, therapeutic shoes, foot orthotics, or other devices to support the feet, unless required for the treatment of or to prevent complications of diabetes; or if the orthopedic shoe is an integral part of a covered leg brace; or Trusses, corsets, and other support items; or Repair and replacement due to loss, misuse, abuse or theft. Any item listed in the Exclusions and Limitations section of this Certificate. Vision Care Benefits Pediatric Routine Vision Exams Covered Benefits include charges made by a legally qualified ophthalmologist or optometrist for a routine vision exam. The exam will include refraction and glaucoma testing. This benefit is subject to an age limit as shown on the Schedule of Benefits. Pediatric Vision Care Services and Supplies Covered Benefits include charges for the following vision care services and supplies: Preferred eyeglass frames, Prescription lenses or Prescription contact lenses identified by a vision Participating Provider. These are eyeglass frames, Prescription lenses, or Prescription contact lenses that are covered at 100% by a vision Participating Provider. Non-Preferred eyeglass frames, Prescription lenses or Prescription contact lenses that are not identified as Preferred by a vision Participating Provider. Coverage includes charges incurred for: Non-conventional Prescription contact lenses that are required to correct visual acuity to 20/40 or better in the better eye and that correction cannot be obtained with conventional lenses; Aphakic Prescription lenses prescribed after cataract surgery has been performed; and Low vision services. This benefit is subject to an age limit as shown on the Schedule of Benefits. A listing of the locations of the vision Participating Providers under this Plan can be accessed at the website. Be sure to look at the appropriate vision Participating Provider listing that applies to your plan, since different Aetna plans use different networks of providers. You must present your ID card to the vision Participating Provider at the time of service. This benefit is subject to the maximums shown on the Schedule of Benefits. As to coverage for Prescription lenses in a calendar year, this benefit will cover either Prescription lenses for eyeglass frames or Prescription contact lenses, but not both. Benefit Limitations: Unless specified above, not covered under this benefit are charges incurred for services and supplies: Office visits to an ophthalmologist, optometrist or optician related to the fitting of Prescription contact lenses. Eyeglass frames, Prescription lenses and Prescription contact lenses that are not identified as Preferred by a vision Participating Provider. Eyeglass frames, non-prescription lenses and non-prescription contact lenses that are for cosmetic purposes. HI HMO-HNOSG2016COC SG Off Exchange
44 Adult Routine Vision Exams Covered Benefits include charges made by a legally qualified ophthalmologist or optometrist for a routine vision exam. The exam will include refraction and glaucoma testing. Benefit Limitations: Unless specified above, not covered under this benefit are charges incurred for services and supplies: Office visits to an ophthalmologist, optometrist or optician related to the fitting of Prescription contact lenses. Eyeglass frames, Prescription lenses and Prescription contact lenses that are not identified as Preferred by a vision Participating Provider. Eyeglass frames, non-prescription lenses and non-prescription contact lenses that are for cosmetic purposes. Important Notes: Refer to the Schedule of Benefits for any cost-sharing, age limits, exam frequency limits and maximums that apply to vision exams, services and supplies. Pediatric Dental Services Covered Benefits include charges made by a Participating Dental Provider for the dental services listed in the Pediatric Dental Care Schedule below and provided to covered persons through the end of the month in which the person turns 19. The plan does not pay a benefit for all dental care expenses that you incur. Important Reminder: Your dental services and supplies must meet the following rules to be covered by the plan: The services and supplies must be Medically Necessary. The services and supplies must be covered by the plan. You must be covered by the plan when you incur the expense. About the Dental Plan The plan is a Dental Plan that covers a limited range of dental services and supplies. You can visit the Participating Dental Provider of your choice when you need dental care. You can choose a Participating Dental Provider who is in the dental network. Using Participating Providers You will receive the Plan s higher level of benefits when your care is provided by a Participating Dental Provider. The plan begins to pay benefits after you satisfy a Deductible. HI HMO-HNOSG2016COC SG Off Exchange
45 Participating Dental Providers have agreed to accept the Negotiated Charge. You will be reimbursed for a covered benefit received from a Participating Dental Provider, up to the Negotiated Charge and the maximum benefits under this plan, less any cost sharing required by you such as Deductibles and Copayments. Your Copayment is based on the Negotiated Charge. You will not have to pay any balance bills above the Negotiated Charge for that covered service or supply. You will not have to submit dental claims for treatment received from Participating Dental Providers. Your Participating Dental Provider will take care of claim submission. Aetna will directly pay the Participating Dental Provider less any cost sharing required by you. You will be responsible for Deductibles and Copayments, if any. You will receive notification of what the plan has paid toward your Covered Benefits. It will indicate any amounts you owe towards any Deductible, Copayment or other non-covered Benefits you have incurred. You may elect to receive this notification by , or through the mail. Contact Member Services by logging onto the Aetna website or calling the toll-free number on the back of your ID card if you have questions regarding your statement. Availability of Providers Aetna cannot guarantee the availability or continued participation of a particular Provider. Either Aetna or any Participating Dental Provider may terminate the Provider contract or a Participating Dental Provider may limit the number of patients accepted in a practice. Pediatric Dental Care Schedule If: A charge is made for an unlisted service given for the dental care of a specific condition; and The list includes one or more services that, under standard practices, are separately suitable for the dental care of that condition; then the charge will be considered to have been made for a service in the list that Aetna determines would have produced a professionally acceptable result. The Pediatric Dental Care Schedule is a list of dental benefits that are covered by the plan. There are several categories of Covered Benefits: Diagnostic and Preventive Care Basic Restorative Care Major Restorative Care Orthodontic Care These covered services and supplies are grouped as Type A, Type B, Type C and Orthodontic Expenses. Coverage is also provided for a Dental Emergency. For additional information, please refer later in this amendment to the In Case of a Dental Emergency section. Getting an Advance Claim Review The purpose of the advance claim review is to determine, in advance, the benefits the plan will pay for proposed services. Knowing ahead of time which services are covered by the plan, and the benefit amount payable, helps you and your Participating Dentist make informed decisions about the care you are considering. HI HMO-HNOSG2016COC SG Off Exchange
46 Important Note: The pre-treatment review process is not a guarantee of benefit payment, but rather an estimate of the amount or scope of benefits to be paid. When to Get an Advance Claim Review An advance claim review is recommended whenever a course of dental treatment is likely to cost more than $300. Ask your Participating Dentist to write down a full description of the treatment you need, using either an Aetna claim form or an ADA approved claim form. Then, before actually treating you, your Participating Dentist should send the form to Aetna. Aetna may request supporting images and other diagnostic records. Once all of the information has been gathered, Aetna will review the proposed treatment plan and provide you and your Participating Dentist with a statement outlining the benefits payable by the plan. You and your Participating Dentist can then decide how to proceed. The advance claim review is voluntary. It is a service that provides you with information that you and your Participating Dentist can consider when deciding on a course of treatment. It is not necessary for emergency treatment or routine care such as cleaning teeth or check-ups. In determining the amount of benefits payable, Aetna will take into account alternate procedures, services, or courses of treatment for the dental condition in question in order to accomplish the anticipated result. (See the Alternate Treatment Rule later in this amendment for more information on alternate dental procedures.) What Is a Course of Dental Treatment? A course of dental treatment is a planned program of one or more services or supplies. The services or supplies are provided by one or more Participating Dentists to treat a dental condition that was diagnosed by the attending Participating Dentist as a result of an oral examination. A course of treatment starts on the date your Participating Dentist first renders a service to correct or treat the diagnosed dental condition. In Case of a Dental Emergency If you need dental care for the palliative treatment (e.g., pain relieving, stabilizing) of a Dental Emergency, you are covered 24 hours a day, 7 days a week. A Dental Emergency is any dental condition which: Occurs unexpectedly; Requires immediate diagnosis and treatment in order to stabilize the condition; and Is characterized by symptoms such as severe pain and bleeding. You must follow the guidelines below when you believe that you have a Dental Emergency. Services provided for a Dental Emergency will be covered at the network level of benefits even if services and supplies are not provided by a Participating Dental Provider. If you have a Dental Emergency, you may get treatment from any dentist. You should consider calling your Participating Dental Provider, if possible. Your Participating Dental Provider may be more familiar with your dental needs. If you are not able to reach your Participating Dental Provider or you are away from home, you may get treatment from any Dentist. You may also call Aetna Member Services at the toll-free telephone number on your ID Card for help in finding a Dentist. HI HMO-HNOSG2016COC SG Off Exchange
47 Care received from a Non-Participating dental provider must be for the temporary relief of the dental emergency until you can be seen by your Participating Dental Provider. Care received from a dental Non-Participating provider for other than the temporary relief of the dental emergency may cost you more. To receive the maximum level of benefits, care should be provided by a Participating Dental Provider. The plan pays a benefit up to the Dental Emergency Maximum, shown in the Schedule of Benefits. Rules and Limits That Apply to the Dental Benefits Several rules apply to the dental benefits. Following these rules will help you use the plan to your advantage by avoiding expenses that are not covered by the plan. Waiting Period The plan has a waiting period for Orthodontic Treatment as follows Orthodontic treatment: Your coverage will take effect after 24 months of continuous coverage under the Plan. Orthodontic Treatment Rule Orthodontic treatment is covered when it is medically necessary for a covered person under the age of 19 with a severe, dysfunctional, handicapping condition such as: Cleft lip and palate, cleft palate, or cleft lip with alveolar process involvement The following craniofacial anomalies: - Hemifacial microsomia; - Craniosynostosis syndromes; - Cleidocranial dental dysplasia; - Arthrogryposis; or - Marfan syndrome Anomalies of facial bones and/or oral structures Facial trauma resulting in functional difficulties Reimbursable orthodontic services include: Pre-orthodontic treatment visit Comprehensive orthodontic treatment Orthodontic retention (removal of appliances, construction and placement of retainers(s) This benefit does not cover charges for the following: Replacement of broken appliances; Re-treatment of orthodontic cases; Changes in treatment necessitated by an accident; Maxillofacial surgery; Myofunctional therapy; Lingually placed direct bonded appliances and arch wires (i.e. invisible braces ); or Removable acrylic aligners (i.e. invisible aligners ). HI HMO-HNOSG2016COC SG Off Exchange
48 Replacement Rule Crowns, inlays, onlays and veneers, complete dentures, removable partial dentures, fixed partial dentures (bridges) and other prosthetic services are subject to the plan's replacement rule. That means certain replacements of, or additions to, existing crowns, inlays, onlays, veneers, dentures or bridges are covered only when you give proof to Aetna that: You had a tooth (or teeth) extracted after the existing denture or bridge was installed. As a result, you need to replace or add teeth to your denture or bridge. The present crown, inlay and onlay, veneer, complete denture, removable partial denture, fixed partial denture (bridge), or other prosthetic service was installed at least 5years before its replacement and cannot be made serviceable. Your present denture is an immediate temporary one that replaces that tooth (or teeth). A permanent denture is needed, and the temporary denture cannot be used as a permanent denture. Replacement must occur within 12 months from the date that the temporary denture was installed. Tooth Missing but Not Replaced Rule The first installation of complete dentures, removable partial dentures, fixed partial dentures (bridges), and other prosthetic services will be covered if: The dentures, bridges or other prosthetic items are needed to replace one or more natural teeth; and The tooth that was removed was not an abutment to a removable or fixed partial denture installed during the prior 5 years. The extraction of a third molar does not qualify. Any such appliance or fixed bridge must include the replacement of an extracted tooth or teeth. Alternate Treatment Rule Sometimes there are several ways to treat a dental problem, all of which provide acceptable results. When alternate services or supplies can be used, the plan's coverage will be limited to the cost of the least expensive service or supply that is: Customarily used nationwide for treatment; and Deemed by the dental profession to be appropriate for treatment of the condition in question. The service or supply must meet broadly accepted standards of dental practice, taking into account your current oral condition. You should review the differences in the cost of alternate treatment with your Participating Dental Provider. Of course, you and your Participating Dental Provider can still choose the more costly treatment method. You are responsible for any charges in excess of what the plan will cover. Coverage for Dental Work Completed After Termination of Coverage Your dental coverage may end while you or your covered dependent is in the middle of treatment. The plan does not cover dental services that are given after your coverage terminates. There is an exception. The plan will cover the following services if they are ordered while you were covered by the plan, and installed within 30days after your coverage ends. Inlays; Onlays; Crowns; Removable bridges; Cast or processed restorations; Dentures; Fixed partial dentures (bridges); and Root canals. HI HMO-HNOSG2016COC SG Off Exchange
49 "Ordered" means: For a denture: the impressions from which the denture will be made were taken. For a root canal: the pulp chamber was opened. For any other item: the teeth which will serve as retainers or supports, or the teeth which are being restored: - Must have been fully prepared to receive the item; and - Impressions have been taken from which the item will be prepared. Pediatric Dental Plan Exclusions Not every dental care service or supply is covered by the plan, even if prescribed, recommended, or approved by your Physician or Dental Provider. The plan covers only those services and supplies that are Medically Necessary. Charges made for the following are not covered except to the extent listed under the Covered Benefits section of the Certificate or by amendment attached to the Certificate. In addition, some services are specifically limited or excluded. This section describes services and supplies that are not covered or subject to special limitations. These dental exclusions are in addition to the exclusions that apply to health coverage. Acupuncture, acupressure and acupuncture therapy, except as provided in the Covered Benefits section of the Certificate. Any charges in excess of the benefit, dollar, day, visit, or supply limits stated in the Certificate. Any instruction for diet, plaque control and oral hygiene. Charges submitted for services: - By an unlicensed Hospital, Physician or other provider; or - By a licensed Hospital, Physician or other provider that are not within the scope of the provider s license. Charges submitted for services that are not rendered, or not rendered to a person not eligible for coverage under the plan. Cosmetic services and supplies including plastic surgery, reconstructive surgery, Cosmetic surgery, personalization or characterization of dentures or other services and supplies which improve alter or enhance appearance, augmentation and vestibuloplasty, and other substances to protect, clean, whiten bleach or alter the appearance of teeth; whether or not for psychological or emotional reasons; except to the extent coverage is specifically provided in the Covered Benefits section of the Certificate. Facings on molar crowns and pontics will always be considered Cosmetic. Court ordered services, including those required as a condition of parole or release. Crown, inlays and onlays, and veneers unless: - It is treatment for decay or traumatic injury and teeth cannot be restored with a filling material; or - The tooth is an abutment to a covered partial denture or fixed bridge. HI HMO-HNOSG2016COC SG Off Exchange
50 Dental Examinations that are: - Required by a third party, including examinations and treatments required to obtain or maintain employment, or which an employer is required to provide under a labor agreement; - Required by any law of a government, securing insurance or school admissions, or professional or other licenses; - Required to travel, attend a school, camp, or sporting event or participate in a sport or other recreational activity; and - Any special medical reports not directly related to treatment except when provided as part of a covered service. Dental implants, braces (that are determined not to be Medically Necessary), mouth guards, and other devices to protect, replace or reposition teeth and removal of implants. Dental services and supplies that are covered in whole or in part under any other part of this plan. Dentures, crowns, inlays, onlays, bridges, or other appliances or services used for the purpose of splinting, to alter vertical dimension, to restore occlusion, or correcting attrition, abrasion, abfraction or erosion. Except as covered in the Covered Benefits section of the Certificate, treatment of any Jaw Joint Disorder and treatments to alter bite or the alignment or operation of the jaw, including temporomandibular joint disorder (TMJ) treatment, orthognathic surgery, and treatment of malocclusion or devices to alter bite or alignment. Experimental or Investigational drugs, devices, treatments or procedures, except as described in the What the Medical Benefit Covers section of the Certificate. General anesthesia and intravenous sedation, unless specifically covered and only when done in connection with another Medically Necessary covered service or supply. Medicare: Payment for that portion of the charge for which Medicare is the primary payer. Miscellaneous charges for services or supplies including: - Annual or other charges to be in a Physician s practice; - Charges to have preferred access to a Physician s services such as boutique or concierge Physician practices; - Cancelled or missed appointment charges or charges to complete claim forms; - Charges the recipient has no legal obligation to pay; or the charges would not be made if the recipient did not have coverage (to the extent exclusion is permitted by law) including: Care in charitable institutions; Care for conditions related to current or previous military service; Care while in the custody of a governmental authority; Any care a public Hospital or other facility is required to provide; or Any care in a Hospital or other facility owned or operated by any federal, state or other governmental entity, except to the extent coverage is required by applicable laws. HI HMO-HNOSG2016COC SG Off Exchange
51 Non-Medically Necessary services, including but not limited to, those treatments, services, Prescription Drugs and supplies which are not Medically Necessary, as determined by Aetna, for the diagnosis and treatment of illness, injury, restoration of physiological functions, or covered preventive services. This applies even if they are prescribed, recommended or approved by your Physician or Dentist. Orthodontic treatment except as covered in this agreement and in the Covered Benefits section of the Certificate. Pontics, crowns, cast or processed restorations made with high noble metals (gold). Prescribed drugs; pre-medication; or analgesia. Replacement of a device or appliance that is lost, missing or stolen, and for the replacement of appliances that have been damaged due to abuse, misuse or neglect and for an extra set of dentures. Replacement of teeth beyond the normal complement of 32. Routine dental exams and other preventive services and supplies, except as specifically provided in this amendment and in the Covered Benefits section of the Certificate. Services and supplies done where there is no evidence of pathology, dysfunction, or disease other than covered preventive services. Services and supplies provided for your personal comfort or convenience, or the convenience of any other person, including a provider. Services and supplies provided in connection with treatment or care that is not covered under the plan. Services rendered before the effective date or after the termination of coverage. Space maintainers except when needed to preserve space resulting from the premature loss of deciduous teeth. Surgical removal of impacted wisdom teeth only for orthodontic reasons. Treatment by other than a Dentist or dental provider that is legally qualified to furnish dental services or supplies Work related: Any illness or injury related to employment or self-employment including any injuries that arise out of (or in the course of) any work for pay or profit, unless no other source of coverage or reimbursement is available to you for the services or supplies. Sources of coverage or reimbursement may include your employer, workers compensation, or an occupational illness or similar program under local, state or federal law. A source of coverage or reimbursement will be considered available to you even if you waived your right to payment from that source. If you are also covered under a workers compensation law or similar law, and submit proof that you are not covered for a particular illness or injury under such law, that illness or injury will be considered non-occupational regardless of cause. HI HMO-HNOSG2016COC SG Off Exchange
52 EXCLUSIONS AND LIMITATIONS Medical Exclusions The following are not Covered Benefits except as described in the Covered Benefits section of this Certificate or by amendment(s) attached to this Certificate: Acupuncture, acupressure and acupuncture therapy, except as provided in the Covered Benefits section of the Certificate. Ambulance services, for routine transportation to receive outpatient or inpatient services. Any non-emergency charges for Covered Benefits incurred outside of the United States. Behavioral health services that are not primarily aimed at treatment of illness, injury, restoration of physiological functions or that do not have a physiological or organic basis. Biofeedback, except as precertified by Aetna. Any related services including processing, storage or replacement costs, and the services of blood donors, apheresis or plasmapheresis are not covered. For autologous blood donations, only administration and processing costs are covered. Care for conditions that state or local laws require to be treated in a public facility, including but not limited to, mental illness commitments. Care furnished to provide a safe surrounding, including the charges for providing a surrounding free from exposure that can worsen the disease or injury. Clinical trial therapies - Services and supplies related to data collection and record-keeping that is solely needed due to the clinical trial (i.e. protocol-induced costs) - Services and supplies provided by the trial sponsor without charge to you - The experimental intervention itself (except Medically Necessary Category B investigational devices and promising experimental and investigational interventions for terminal Illnesses in certain clinical trials in accordance with Aetna s claim policies). Contraception, except as specifically described in the Covered Benefit section including, but not limited to, over the counter contraceptive supplies such as condoms, contraceptive foams, jellies and ointments. Cosmetic Surgery, or treatment relating to the consequences of, or as a result of, Cosmetic Surgery, other than Medically Necessary Services. This exclusion includes, but is not limited to, surgery to correct gynecomastia and breast augmentation procedures, and otoplasties. Reduction mammoplasty, except when determined to be Medically Necessary by an Aetna Medical Director, is not covered. This exclusion does not apply to surgery to correct the results of injuries causing the impairment, or as a continuation of a staged reconstruction procedure, or congenital defects necessary to restore normal bodily functions, including but not limited to, cleft lip and cleft palate or surgery required for post-mastectomy reconstruction. HI HMO-HNOSG2016COC SG Off Exchange
53 Court ordered services, or those required by court order as a condition of parole or probation. Custodial Care. Dental services except as specifically covered in the Covered Benefits section including but not limited to, services related to the care, filling, removal or replacement of teeth and treatment of injuries to or diseases of the teeth, dental services related to the gums, apicoectomy (dental root resection), orthodontics, root canal treatment, soft tissue impactions, bony impacted teeth, alveolectomy, augmentation and vestibuloplasty treatment of periodontal disease, false teeth, prosthetic restoration of dental implants, and dental implants. This exclusion does not include bone fractures, removal of tumors, and odontogenic cysts. Educational services except as specifically covered in the Covered Benefits section and treatment of behavioral disorders, together with services for remedial education including evaluation or treatment of learning disabilities, minimal brain dysfunction, developmental and learning disorders, behavioral training, and cognitive rehabilitation. This includes services, treatment or educational testing and training related to behavioral (conduct) problems, learning disabilities, or developmental delays. Special education, including lessons in sign language to instruct a Member, whose ability to speak has been lost or impaired, to function without that ability, are not covered. Experimental or Investigational Procedures, or ineffective surgical, medical, psychiatric, or dental treatments or procedures, research studies, or other experimental or investigational health care procedures or pharmacological regimes as determined by Aetna, unless precertified by Aetna. This exclusion will not apply with respect to drugs: - That have been granted treatment investigational new drug (IND) or Group c/treatment IND status; - That are being studied at the Phase III level in a national clinical trial sponsored by the National Cancer Institute; or - Aetna has determined that available scientific evidence demonstrates that the drug is effective or the drug shows promise of being effective for the disease. E-Visits Non-Participating Providers. Any services that are given by Providers that are not contracted with Aetna as E-visit Providers. Any services that are not provided during an internet-based consult or via telephone. Foot orthotics unless required for the treatment of, or to prevent, complications of diabetes. Habilitation Therapy Services -- Physical, Occupational and Speech Therapy Services for the treatment of delays in development, including speech development, unless as a result of a gross anatomical defect present at birth, including: Therapies to treat delays in development and/or chronic conditions. Examples of noncovered diagnoses that are considered both developmental and/or chronic in nature are: - Down syndrome Any service unless provided in accordance with a specific treatment plan Services you get from a Home Health Care Agency. HI HMO-HNOSG2016COC SG Off Exchange
54 Services not given by a Physician (or under the direct supervision of a Physician), physical, occupational or speech therapist. This exclusion does not apply to physical therapy, occupational therapy or speech therapy provided for the treatment of Autism Spectrum Disorder. Hair analysis. Hearing aids. Related services and supplies, except as specifically described in this Certificate. Home births. Home uterine activity monitoring. Household equipment, including but not limited to, the purchase or rental of exercise cycles, water purifiers, hypo-allergenic pillows, mattresses or waterbeds, whirlpool or swimming pools, exercise and massage equipment, central or unit air conditioners, air purifiers, humidifiers, dehumidifiers, escalators, elevators, ramps, stair glides, emergency alert equipment, handrails, heat appliances, improvements made to a Member s house or place of business, and adjustments made to vehicles. Hypnotherapy, except when precertified by Aetna. Implantable drugs. Infertility. Any services, treatments, procedures or supplies that are designed to enhance fertility or the likelihood of conception, such as: - Drugs, and drugs related to the treatment of non-covered benefits. - Injectable infertility medication, including but not limited to menotropins, hcg, and GnRH agonists. - Reversal of voluntary sterilization including related procedures, services and supplies. - The purchase of donor sperm and any charges for the storage of sperm. - All charges associated with surrogacy for you or the surrogate. A surrogate is a female carrying her own genetically related child where the child is conceived with the intention of turning the child over to be raised by others, including the biological father. - Home ovulation prediction kits or home pregnancy tests. - Medication that is experimental and investigational in relation to infertility. - The purchase of donor embryos, donor oocytes, or donor sperm. - Charges associated with cryopreservation or storage of cryopreserved eggs and embryos (e.g., office, hospital, ultrasounds, laboratory tests, etc.), including thawing charges. - All charges associated with the care of the donor in a donor egg cycle. This includes, but is not limited to, any payments to the donor, donor screening fees, fees for lab tests, and any charges associated with care of the donor required for donor egg retrievals or transfers. - All charges associated with the use of a gestational carrier for the female acting as the gestational carrier. A gestational carrier is a female carrying an embryo to which she is not genetically related. - Comprehensive infertility services and ART services. - Any charges associated with obtaining sperm for ART services. - Ovulation induction with menotropins, Intrauterine insemination and any related services, products or procedures. HI HMO-HNOSG2016COC SG Off Exchange
55 - In vitro fertilization (IVF), Zygote intrafallopian transfer (ZIFT), Gamete intra-fallopian transfer (GIFT), Cryopreserved embryo transfers and any related services, products or procedures (such as Intracytoplasmic sperm injection (ICSI) or ovum microsurgery). Mental health treatment Mental health services for the following categories (or equivalent terms as listed in the most recent version of the International Classification of Diseases (ICD): - Dementias and amnesias without behavioral disturbances - Sexual deviations and disorders except for gender identity disorders - Tobacco use disorders - Specific disorders of sleep - Antisocial or dissocial personality disorder - Pathological gambling, kleptomania, pyromania - Specific delays in development (learning disorders, academic underachievement) - Intellectual disability - Wilderness Treatment Programs or any such related or similar programs, school and/or education services. Military service related diseases, disabilities or injuries for which the Member is legally entitled to receive treatment at government facilities and which facilities are reasonably available to the Member. Missed appointment charges. Non-medically necessary services, including but not limited to, those services and supplies: - Which are not Medically Necessary, as determined by Aetna, for the diagnosis and treatment of illness, injury, restoration of physiological functions, or covered preventive services; - That do not require the technical skills of a medical, mental health or a dental professional; - Furnished mainly for the personal comfort or convenience of the Member, or any person who cares for the Member, or any person who is part of the Member s family, or any Provider; - Furnished solely because the Member is an inpatient on any day in which the Member s disease or injury could safely and adequately be diagnosed or treated while not confined; - Furnished solely because of the setting if the service or supply could safely and adequately be furnished in a Physician s or a dentist s office or other less costly setting. Non-prescription drugs and medicines, except as provided on an inpatient basis or as specifically covered in the Covered Benefits section. Non-surgical treatment of temporomandibular joint disorder (TMJ), including but not limited to, treatment performed by prosthesis placed directly on the teeth, surgical and non-surgical medical and dental services, and diagnostic or therapeutics services related to TMJ. Nursing and aide services provided outside of the home (such as in conjunction with school, vacation, work or recreational activities). HI HMO-HNOSG2016COC SG Off Exchange
56 Outpatient supplies, including but not limited to, medical consumable or disposable supplies such as syringes, incontinence pads, elastic stockings, and reagent strips except as described in the Covered Benefits section. Outpatient prescription contraceptive drugs and devices - Oral drugs that are Brand-Name Prescription Drugs and Biosimilar Prescription Drugs. - Injectable drugs that are Brand-Name Prescription Drugs and Biosimilar Prescription Drugs. - Vaginal rings that are Generic Prescription Drugs, Brand-Name Prescription Drugs and Biosimilar Prescription Drugs. - Transdermal contraceptive patches that are Generic Prescription Drugs, Brand-Name Prescription Drugs and Biosimilar Prescription Drugs. - Female contraceptive devices that are brand-name devices. - FDA-approved female brand-name and biosimilar emergency contraceptives and brandname over-the-counter (OTC) emergency contraceptives. - Other FDA-approved female and male brand-name over-the-counter (OTC) contraceptives. Payment for that portion of the benefit for which Medicare or another party is the primary payer. Personal comfort or convenience items, including those services and supplies not directly related to medical care, such as guest meals and accommodations, barber services, telephone charges, radio and television rentals, homemaker services, travel expenses, take-home supplies, and other like items and services. Private Duty Nursing except as described in Hospital and Other Facility Benefit (See the Home Health Benefits and Hospital and Other Facility Care section regarding coverage of nursing services). Recreational, educational, and sleep therapy, including any related diagnostic testing. Religious, marital and sex counseling, including services and treatment related to religious counseling, marital/relationship counseling, and sex therapy. Reversal of voluntary sterilizations, including related follow-up care and treatment of complications of such procedures. Routine foot/hand care, including routine reduction of nails, calluses and corns. Services for which a Member is not legally obligated to pay in the absence of this coverage. Services for the treatment of sexual dysfunctions or inadequacies, including therapy, supplies, or counseling for sexual dysfunctions or inadequacies that do not have a physiological or organic basis. Services, including those related to pregnancy, rendered before the effective date or after the termination of the Member s coverage, unless coverage is continued under the Continuation section of this Certificate. HI HMO-HNOSG2016COC SG Off Exchange
57 Services performed by a relative of a Member for which, in the absence of any health benefits coverage, no charge would be made. Services required by third parties, including but not limited to, physical examinations, diagnostic services and immunizations in connection with obtaining or continuing employment, obtaining or maintaining any license issued by a municipality, state, or federal government, securing insurance coverage, travel, school admissions or attendance, including examinations required to participate in athletics, except when such examinations are considered to be part of an appropriate schedule of wellness services. Services which are not a Covered Benefit under this Certificate, even when a prior Referral has been issued by a PCP. Short-Term Rehabilitation Services -- Outpatient Cognitive Rehabilitation, Physical, Occupational and Speech Therapy Services for the treatment of delays in development, including speech development, unless as a result of a gross anatomical defect present at birth, including: Therapies to treat delays in development and/or chronic conditions. Examples of non-covered diagnoses that are considered both developmental and/or chronic in nature are: - Down syndrome - Cerebral palsy Any service unless provided in accordance with a specific treatment plan Services you get from a Home Health Care Agency. Services provided by a Physician, or treatment covered as part of the spinal manipulation benefit. This applies whether or not benefits have been paid under the spinal manipulation section. Services not given by a Physician (or under the direct supervision of a Physician), physical, occupational or speech therapist. This exclusion does not apply to physical therapy, occupational therapy or speech therapy provided for the treatment of Autism Spectrum Disorder. Specific non-standard allergy services and supplies, including but not limited to, skin titration (wrinkle method), cytotoxicity testing (Bryan's Test), treatment of non-specific candida sensitivity, and urine autoinjections. Specific injectable drugs, except as provided in the Covered Benefits section of the Certificate, including: - Experimental drugs or medications, or drugs or medications that have not been proven safe and effective for a specific disease or approved for a mode of treatment by the Food and Drug Administration (FDA) and the National Institutes of Health (NIH); - Needles, syringes and other injectable aids; - Drugs related to the treatment of non-covered services; and - Drugs related to the treatment of Infertility, contraception, and performance enhancing steroids. Special medical reports, including those not directly related to treatment of the Member, e.g., employment or insurance physicals, and reports prepared in connection with litigation. HI HMO-HNOSG2016COC SG Off Exchange
58 Telemedicine: Any services that are given by providers that are not contracted with Aetna as telemedicine providers. Any services that are provided other than during an internet-based consult or via telephone. Therapy or rehabilitation, including but not limited to, primal therapy, chelation therapy, rolfing, psychodrama, megavitamin therapy, purging, bioenergetic therapy, vision perception training, and carbon dioxide. Thermograms and thermography. Treatment in a federal, state, or governmental entity, including care and treatment provided in a non-participating Hospital owned or operated by any federal, state or other governmental entity, except to the extent required by applicable laws. Treatment of mental retardation, defects, and deficiencies. This exclusion does not apply to mental health services or to medical treatment of mentally retarded Members in accordance with the benefits provided in the Covered Benefits section of this Certificate. Treatment of occupational injuries and occupational diseases, including those injuries that arise out of (or in the course of) any work for pay or profit, or in any way results from a disease or injury which does. If a Member is covered under a Workers' Compensation law or similar law, and submits proof that the Member is not covered for a particular disease or injury under such law, that disease or injury will be considered "non-occupational" regardless of cause. Unauthorized services, including any services obtained by, or on behalf of a, Member that require precertification by Aetna. Participating Providers are responsible for obtaining precertification of Covered Benefits from Aetna. This exclusion does not apply in a Medical Emergency, in an Urgent Care situation, or when it is a direct access benefit. Vision: Vision-related services and supplies, except as described in the Covered Benefits section. In addition, the plan does not cover: - Special supplies such as non-prescription sunglasses; - Vision service or supply which does not meet professionally accepted standards; - Special vision procedures, such as orthoptics or vision training; - Eye exams during your stay in a Hospital or other facility for health care; - Eyeglasses or duplicate or spare eyeglasses or lenses or frames; - Replacement of lenses or frames that are lost or stolen or broken; - Acuity tests; - Eye Surgery for the correction of vision, including radial keratotomy, LASIK and similar procedures; - Services to treat errors of refraction. Weight control services including surgical procedures, medical treatments, weight control/loss programs, dietary regimens and supplements, food or food supplements, appetite suppressants and other medications; exercise programs, exercise or other equipment; and other services and supplies that are primarily intended to control weight or treat obesity, including Morbid Obesity, or for the purpose of weight reduction, regardless of the existence of comorbid conditions except as provided by this Certificate. HI HMO-HNOSG2016COC SG Off Exchange
59 Limitations In the event there are 2 or more alternative Medical Services which in the sole judgment of Aetna are equivalent in quality of care, Aetna reserves the right to provide coverage only for the least costly Medical Service, as determined by Aetna, provided that Aetna pre-authorizes the Medical Service or treatment. Determinations regarding eligibility for benefits, coverage for services, benefit denials and all other terms of this Certificate are at the sole discretion of Aetna, subject to the terms of this Certificate. Wilderness treatment programs (whether or not the program is part of a licensed residential treatment facility, or otherwise licensed institution), educational services, schooling or any such related or similar program, including therapeutic programs within a school setting. HI HMO-HNOSG2016COC SG Off Exchange
60 8. Outpatient Prescription Drugs How the Pharmacy Plan Works It is important that you have the information and useful resources to help you get the most out of your Aetna Prescription Drug plan. This Certificate explains: How to access Network Pharmacies and procedures you need to follow; What Prescription Drug expenses are covered and what limits may apply; What Prescription Drug expenses are not covered by the plan; How you share the cost of your covered Prescription Drug benefit; and Other important information such as eligibility, complaints and appeals, termination, and general administration of the plan. A few important notes to consider before moving forward: Unless otherwise indicated, you refers to you and your covered dependents. Your Prescription Drug plan pays benefits only for Prescription Drug expenses described in this Certificate as Covered Benefits that are Medically Necessary. This Certificate applies to coverage only and does not restrict your ability to receive Prescription Drugs that are not or might not be covered benefits under this Prescription Drug plan. Store this Certificate in a safe place for future reference. Notice The plan does not cover all Prescription Drugs, medications and supplies. Refer to the Limitations section of this coverage and Exclusions section of your Certificate. Covered Benefits are subject to cost sharing requirements as described in the cost sharing sections of this coverage and in your Schedule of Benefits. Specialty Prescription Drug refills will only be covered when obtained through Aetna s Specialty Pharmacy. This plan covers only certain Prescription Drugs in accordance with the plan and the Preferred Drug Guide (Formulary). This plan does not cover all Prescription Drugs. Accessing Pharmacies and Benefits This plan provides access to Covered Benefits through a network of pharmacies, vendors or suppliers. Aetna has contracted for these Network Pharmacies to provide Prescription Drugs and other supplies to you. Obtaining your benefits through Network Pharmacies has many advantages. Benefits and cost sharing may vary by the type of network pharmacy where you obtain your Prescription Drug and whether or not you purchase a brand-name or generic drug. Network pharmacies include retail, mail order and specialty Pharmacies. To better understand the choices that you have with your plan, please carefully review the following information. HI HMO-HNOSG2016COC SG Off Exchange
61 Accessing Network Pharmacies and Benefits You may select a Network Pharmacy from the Aetna Network Pharmacy Directory or by logging on to Aetna s website at You can search Aetna s online directory, DocFind, for names and locations of Network Pharmacies. If you cannot locate a Network Pharmacy in your area call Member Services. You must present your ID card to the Network Pharmacy every time you get a Prescription filled to be eligible for network Covered Benefits. The Network Pharmacy will calculate your claim online. You will pay any deductible, copayment or coinsurance directly to the Network Pharmacy. You do not have to complete or submit claim forms. The Network Pharmacy will take care of claim submission. Emergency Prescriptions When you need a Prescription filled in an emergency or urgent care situation, or when you are traveling, you can obtain network benefits by filling your Prescription at any Network Retail Pharmacy. The Network Pharmacy will fill your Prescription and only charge you your plan s cost sharing amount. If you access an Non-Participating Pharmacy you will pay the full cost of the prescription and will need to file a claim for reimbursement. You will be reimbursed for your Covered Benefits up to the cost of the Prescription less your plan s cost sharing for network benefits. This network level of coverage for Prescription Drugs obtained from a Non-Participating Pharmacy is limited to those obtained in connection with Emergency Care and out-of-area Urgent Care services. Availability of Providers Aetna cannot guarantee the availability or continued network participation of a particular Pharmacy. Either Aetna or any Network Pharmacy may terminate the provider contract. Cost Sharing for Network Benefits You share in the cost of your benefits. Cost Sharing amounts and provisions are described in the Schedule of Benefits. You will be responsible for the Copayment for each Prescription or refill as specified in the Schedule of Benefits. The Copayment is payable directly to the Network Pharmacy at the time the Prescription is dispensed. What the Pharmacy Benefit Covers The plan covers charges for outpatient Prescription Drugs for the treatment of an illness or injury, subject to the Limitations section of this coverage and the Medical Benefit and Pharmacy Benefit Exclusions sections of the Certificate. Prescriptions must be written by a Prescriber licensed to prescribe federal legend prescription drugs. This plan covers only certain Prescription Drugs in accordance with the plan and the Preferred Drug Guide (Formulary). This plan does not cover all Prescription Drugs. HI HMO-HNOSG2016COC SG Off Exchange
62 You may minimize your out-of-pocket expenses by selecting a Generic Prescription Drug when available. Prescription drugs that are not listed on the Preferred Drug Guide (Formulary) are excluded from coverage unless a medical exception is approved by Aetna. Refer to the Medical Exceptions described below for details. If it is Medically Necessary for you to use a Prescription Drug not on the Preferred Drug Guide (Formulary), you or your Prescriber must request coverage as a medical exception. Your Prescription Drug benefit may be subject to pharmacy management programs including, but not limited to Precertification, Step Therapy, quantity limits and drug utilization review. Refer to Understanding Pharmacy Precertification for further information. Covered Prescription Drugs are subject to drug and narcotic utilization review by Aetna, your provider and/or your Preferred Network Pharmacy. This may include limiting access of Prescription Drugs prescribed by a specific Provider. Such limitation may be enforced in the event that Aetna identifies an unusual pattern of claims for Covered Benefits. Retail Pharmacy Benefit Outpatient Prescription Drugs are covered when dispensed by a retail pharmacy. Each Prescription is limited to the maximums shown in the Schedule of Benefits. Mail Order Pharmacy Benefit Outpatient prescription drugs are covered when dispensed by a mail order pharmacy that is a network pharmacy. Each prescription is limited to a maximum 90-day supply. Prescriptions less than a 31- day supply or more than a 90-day supply are not eligible for coverage when dispensed by a mail order pharmacy that is a network pharmacy. See the Schedule of Benefits for details on supply limits and cost sharing. After you obtain your second refill at a network retail pharmacy you must notify us of whether you want to use your mail order pharmacy benefit or continue to obtain your prescriptions at a network retail pharmacy by calling the number on the back of your ID card. If you fail to inform us of your choice, then the next prescription refill (and any subsequent refills) at a network retail pharmacy will not be covered. You may contact us at any time to let us know that you intend to use a network retail pharmacy for future prescription refills. Injectable, Self-Injectable and Specialty Care Drug Benefits Injectable drugs, self-injectable drugs and specialty care drugs are covered at the network level of benefits only when dispensed through a retail network pharmacy or Aetna s specialty pharmacy network pharmacy. Specialty care drugs often include typically high-cost drugs that require special handling, special storage or monitoring and include but are not limited to oral, topical, inhaled and injected routes of administration. Refer to Aetna s website, to review the list of injectable drugs, self-injectable drugs and specialty care drugs required to be dispensed through a retail network pharmacy or a specialty pharmacy network pharmacy. The list may be updated from time to time. HI HMO-HNOSG2016COC SG Off Exchange
63 The initial prescription for injectable drugs, self-injectable drugs and specialty care drugs must be filled at a retail network pharmacy or at a specialty pharmacy network pharmacy. Over-the-Counter Prescription Drug Benefit Covered Benefits include certain over-the-counter medications, as determined by Aetna, in an equivalent Prescription dosage strength for the non-preferred, preferred generic or brand-name Prescription Drug appropriate member responsibility. Coverage of the selected over-the-counter medications requires a Prescription. You can access the list by logging onto Orally administered anti-cancer drugs, including chemotherapy drugs. Orally administered anti-cancer drugs, including chemotherapy drugs may be covered when the drug is recognized for treatment of that indication in a standard reference compendium or recommended in the medical literature even if the drug is not approved by the FDA for a particular indication. Other Covered Pharmacy Benefits The following Prescription Drugs, medications and supplies are also Covered Benefits under this Coverage. Off-Label Use U.S. Food and Drug Administration (FDA) approved Prescription Drugs may be covered when the offlabel use of the drug has not been approved by the FDA for your symptom(s) subject to the following: The drug must be accepted as safe and effective to treat your symptom(s) in one of the following standard compendia: American Society of Health-System Pharmacists Drug Information (AHFS Drug Information); Thomson Micromedex DrugDex System (DrugDex); Clinical Pharmacology (Gold Standard, Inc.); or The National Comprehensive Cancer Network (NCCN) Drug and Biologics Compendium; or Use for your symptom(s) has been proven as safe and effective by at least one well-designed controlled clinical trial. Such a trial must be published in a peer reviewed medical journal known throughout the U.S. and either: The dosage of a drug for your symptom(s) is equal to the dosage for the same symptom(s) as suggested in the FDA-approved labeling or by one of the standard compendia noted above; or The dosage has been proven to be safe and effective for your symptom(s) by one or more well-designed controlled clinical trials. Such a trial must be published in a peer reviewed medical journal. Coverage of off-label use of these drugs may, in Aetna s discretion, be subject to Precertification, Step Therapy or other requirements or limitations. Diabetic Supplies Covered Benefits include, but are not limited to the following diabetic supplies upon Prescription by a Physician: Diabetic needles and syringes. Test strips for glucose monitoring and/or visual reading. Diabetic test agents. HI HMO-HNOSG2016COC SG Off Exchange
64 Lancets/lancing devices. Alcohol swabs. Preventive Care Drugs and Supplements Covered Benefits include preventive care drugs and supplements (including over-the-counter drugs and supplements) obtained at a pharmacy. They are covered when they are: prescribed by a Physician; obtained at a pharmacy; and submitted to a pharmacist for processing. The preventive care drugs and supplements covered under this plan include, but may not be limited to: Aspirin: Benefits are available to adults. Oral Fluoride Supplements: Benefits are available to children whose primary water source is deficient in fluoride. Folic Acid Supplements: Benefits are available to adult females planning to become pregnant or capable of pregnancy. Iron Supplements: Benefits are available to children without symptoms of iron deficiency. Coverage is limited to children who are at increased risk for iron deficiency anemia. Vitamin D Supplements: Benefits are available to adults to promote calcium absorption and bone growth in their bodies Reimbursement of Preventive Care Drugs and Supplements at a Pharmacy You will be reimbursed by Aetna for the cost of the preventive care drugs and supplements when you submit proof of loss to Aetna that you purchased a preventive care drug or supplement at a pharmacy. Proof of loss means a copy of the receipt that contains the Prescription information provided by the pharmacist (it is attached to the bag that contains the preventive care OTC drug or supplement). Refer to the provisions Reporting of Claims and Payment of Benefits later in this booklet-certificate for information. You can also contact Member Services by logging onto the Aetna website at or calling the toll-free number on the back of the ID card. Risk Reducing Breast Cancer Prescription Drugs Covered Benefits include Prescription Drugs when prescribed by a Prescriber and the Prescription is submitted to the pharmacist for processing for a woman who is at: Increased risk for breast cancer, and Low risk for adverse medication side effects Coverage of preventive care drugs and supplements will be subject to any sex, age, medical condition, family history, and frequency guidelines in the recommendations of the United States Preventive Services Task Force. Important Note: For details on the guidelines and the current list of covered preventive care drugs and supplements, including risk reducing breast cancer Prescription Drugs, contact Member Services by logging on to your Aetna Navigator secure member website at www. Aetna.com or at the toll-free number on your ID card. Refer to the Schedule of Benefits for the cost-sharing and supply limits that apply to these benefits. HI HMO-HNOSG2016COC SG Off Exchange
65 Contraceptives Covered Benefits include charges made by a Pharmacy for the following contraceptive methods when prescribed by a Prescriber and the Prescription is submitted to the pharmacist for processing: Female oral and injectable contraceptives that are generic prescription drugs, brand-name prescription drugs and biosimilar prescription drugs. Female contraceptive devices that are generic devices and brand-name devices. FDA-approved female: - Generic, brand-name and biosimilar emergency contraceptives; and - Generic and brand-name over-the-counter (OTC) emergency contraceptives obtained without a prescription. Coverage is limited to 1 emergency contraceptive per month. FDA-approved female generic and brand-name over-the-counter (OTC) contraceptives; and FDA-approved male generic and brand-name over-the-counter (OTC) contraceptives. Coverage is limited to one per day and a 30-day supply per prescription. Important Note: This Plan does not cover all contraceptives. For a current listing, contact Member Services by logging onto the Aetna website at or calling the toll-free number on the back of the ID card. Contraceptives can be paid either under your medical plan or pharmacy plan depending on the type of expense and how and where the expense is incurred. Benefits are paid under your medical plan for female contraceptive prescription drugs and devices (including any related services and supplies) when they are provided, administered, or removed, by a physician during an office visit. Refer to the Copay and Deductible Waiver section of your Schedule of Benefits for cost-sharing information. Reimbursement of Contraceptives at an Out-of-Network Pharmacy The FDA-approved contraceptives described above are covered under this Plan when they are: prescribed by a physician; obtained at a pharmacy; and submitted to a pharmacist for processing. You will be reimbursed by Aetna for the cost of the contraceptive when you submit proof of loss to Aetna that you purchased the contraceptive at an out-of-network pharmacy. Proof of loss means a copy of the receipt that contains the prescription information provided by the pharmacist (that is attached to the bag that contains the contraceptive). Refer to the provisions Reporting of Claims and Payment of Benefits later in this Booklet-Certificate for information on submitting claims. You can also contact Member Services by logging onto the Aetna website at www. aetna.com or calling the toll-free number on the back of the ID card. HI HMO-HNOSG2016COC SG Off Exchange
66 Oral Infertility Drugs The following prescription drugs used for the purpose of treating infertility including, but not limited to Progesterone. Understanding Pharmacy Precertification Precertification is required for certain outpatient Prescription Drugs. Prescribers must contact Aetna to request and obtain coverage for such Prescription Drugs. The list of drugs requiring Precertification is subject to periodic review and change by Aetna. For the most up to date information, call the toll-free Member Services number on your member ID card or log on to your Aetna Navigator secure member website at Benefits will be reduced or denied if Aetna does not precertify your prescription drug. So ask your prescriber or pharmacist if your prescription drug needs to be precertified. How to Obtain Precertification If an outpatient Prescription drug requires Precertification and you use a Network Pharmacy the Prescriber is required to obtain Precertification for you. Aetna will let your Prescriber know if the Prescription Drug is Precertified. If Precertification is denied Aetna will notify you how the decision can be appealed. Step Therapy Step Therapy is another form of Precertification. With Step Therapy, certain medications will be excluded from coverage unless one or more prerequisite therapy medications are tried first or unless the Prescriber obtains a medical exception. The plan will not cover the step therapy drug if you do not try a prerequisite therapy prescription drug first or if your prescriber does not get a medical exception. Lists of the Step Therapy drugs and prerequisite drugs are included in the Preferred Drug Guide (Formulary) available upon request or on your Aetna Navigator secure member website at The list of step therapy drugs are subject to change by Aetna. Prescribing Units Depending on the form and packing of the product, some prescription drugs are limited to 100 units dispensed per prescription order or refill. Drugs that are allowed to be filled with greater than 30 day supply are excluded from the 100 unit limitation dispensed per prescription order or refill. Any prescription drug that has duration of action extending beyond one (1) month shall require the number of copayments per prescribing unit that is equal to the anticipated duration of the medication. For example, a single injection of a drug that is effective for three (3) months would require three (3) copayments. Specialty Care Prescription Drugs may have limited access or distribution and are limited to no more than a 30 day supply subject to supply limits. HI HMO-HNOSG2016COC SG Off Exchange
67 Medical Exceptions You or your prescriber may seek a medical exception to obtain coverage for drugs listed on the formulary exclusions list or for which coverage is denied through precertification or step therapy brand-name prescription drugs or biosimilar prescription drugs. You or your prescriber must submit such exception requests to Aetna. Aetna will make a coverage determination within 72 hours after receipt of your request and will notify you or your designee and your prescriber of the decision. Coverage granted as a result of a medical exception shall be based on an individual, case by case medical necessity determination and coverage will not apply or extend to other covered persons. If approved by Aetna, you will receive the non-preferred drug benefit level and the exception will be granted for the duration of the prescription. You, your designee or your prescriber may seek an expedited medical exception process to obtain coverage for non-covered prescription drugs in exigent circumstances. An exigency exists when you are suffering from a health condition that may seriously jeopardize your life, health, or ability to regain maximum function or when you are undergoing a current course of treatment using a non-formulary drug. You, your designee, or your prescriber may submit a request for an expedited review for an exigency as described below by contacting Aetna's Precertification Department at , faxing the request to or submitting the request in writing to CVS Health ATTN: Aetna PA 1300 E Campbell Road Richardson, TX We will make a coverage determination within 24 hours after receipt of your request and will notify you or your designee and your prescriber of our decision. If approved by Aetna the exception will be granted for the duration of the exigency. If you are denied a medical exception based on the above processes, you may have the right to a third party review by an independent external review organization. If our claim decision is one for which you can seek external review, we will say that in the notice of adverse benefit determination we send you. That notice also will describe the external review process. We will notify you, your designee or your prescriber of the coverage determination of the external review no later than 72 hours after receiving your request. If the medical exception is approved, coverage will be provided for the duration of the prescription. For expedited medical exceptions in exigent circumstances, we will notify you, your designee or your prescriber of the coverage determination no later than 24 hours after receiving your request. If the expedited medical exception is approved, coverage will be provided for the duration of the exigency. Pharmacy Benefit Limitations and Exclusions Limitations The plan will not cover expenses for any Prescription Drug for which the actual charge to you is less than the required Copayment, or for any Prescription Drug for which no charge is made to you. Aetna retains the right to review all requests for reimbursement and in its sole discretion make reimbursement determinations subject to the Complaint and Appeals section(s) of the Certificate. Aetna reserves the right to include only one manufacturer s product on the preferred drug list when the same or similar drug (that is, a drug with the same active ingredient), supply or equipment is made by two or more different manufacturers. HI HMO-HNOSG2016COC SG Off Exchange
68 Aetna reserves the right to include only one dosage or form of a drug on the preferred drug list when the same drug (that is, a drug with the same active ingredient) is available in different dosages or forms from the same or different manufacturers. The product in the dosage or form that is listed on our preferred drug list will be covered at the applicable copayment or coinsurance. The number of Copayments you are responsible for per vial of Depo-Provera and/or Medroxyprogesterone, an injectable contraceptive, or similar type contraceptive dispensed for more than a 30 day supply, will be based on the 90 day supply level. Coverage is limited to a maximum of 5 vials per calendar year. The plan will not pay charges for any Prescription Drug dispensed by a Mail Order Pharmacy for the treatment of erectile dysfunction, impotence or sexual dysfunction or inadequacy. Compounded prescriptions will be subject to non-preferred cost sharing Some prescription drugs are subject to quantity limits. These quantity limits help your prescriber and pharmacist check that your prescription drug is used correctly and safely. Aetna relies on medical guidelines, FDA-approved recommendations from drug makers and other criteria developed by Aetna to set these quantity limits. The quantity limit may restrict either the amount dispensed per prescription order or refill. Depending on the form and packing of the product, some prescription drugs are limited to 100 units dispensed per prescription order or refill. Drugs that are allowed to be filled with greater than 30 day supply at a retail pharmacy are limited to 300 units dispensed per prescription order or refill. Any prescription drug that has duration of action extending beyond one (1) month shall require the number of copayments per prescribing unit that is equal to the anticipated duration of the medication. For example, a single injection of a drug that is effective for three (3) months would require three (3) copayments. Specialty care prescription drugs may have limited access or distribution and are limited to no more than a 30-day supply. Plan approved blood glucose meters, asthma holding chambers and peak flow meters are eligible health services, but are limited to one (1) prescription order per calendar year. Prescribed contraceptive diaphragms are limited to two (2) per calendar year. Exclusions Not every health care service or supply is covered by the plan. Even if prescribed, recommended, or approved by your Physician or Dental Provider it may not be covered. The plan covers only those services and supplies that are Medically Necessary and included in the Covered Benefits section. Charges made for the following are not covered except to the extent listed under the Covered Benefits section or by amendment attached to this Certificate. In addition, some services are specifically limited or excluded. This section describes expenses that are not covered or subject to special limitations. These Prescription Drug exclusions are in addition to the exclusions listed under your medical coverage. HI HMO-HNOSG2016COC SG Off Exchange
69 The plan does not cover the following expenses: Abortion drugs Administration or injection of any drug. Any charges in excess of the benefit, day, or supply limits stated in this Certificate. All drugs or medications in a therapeutic drug class if one of the drugs in that Therapeutic Drug Class is not a Prescription Drug, unless Medically Necessary. Allergy sera and extracts. Any non-emergency charges incurred outside of the United States if you traveled to such location to obtain Prescription Drugs, or supplies, even if otherwise covered under this Certificate. This also includes Prescription Drugs or supplies if: - Such prescription drug or supplies are unavailable or illegal in the United States; or - The purchase of such Prescription Drugs or supplies outside the United States is considered illegal. Any drugs or medications, services and supplies that are not Medically Necessary, as determined by Aetna, for the diagnosis, care or treatment of the illness or injury involved. This applies even if they are prescribed, recommended or approved by your Physician. Any Prescription Drug or supply used for the treatment of sexual dysfunction/ enhancement in any form. Any Prescription Drug in any form that is in a similar or identical class; has a similar or identical mode of action; or exhibits similar or identical outcomes. Brand-name prescription drugs and devices when a generic prescription drug equivalent, biosimilar prescription drug or generic prescription drug alternative is available, unless otherwise covered by medical exception. Biological sera, blood, blood plasma, blood products or substitutes or any other blood products. Certain Prescription Drugs but only to the extent such coverage is excluded under the plan and the Preferred Drug Guide (Formulary). Contraceptives, except as specifically described in the Covered Benefits section including, but not limited to, over the counter contraceptive supplies such as condoms, contraceptive foams, jellies and ointments. Cosmetic drugs, medications or preparations used for cosmetic purposes or to promote hair growth, including but not limited to: - Health and beauty aids; - Chemical peels; - Dermabrasion; - Treatments; - Bleaching; HI HMO-HNOSG2016COC SG Off Exchange
70 - Creams; - Ointments or other treatments or supplies, to remove tattoos, scars or to alter the appearance or texture of the skin. Devices and appliances that do not have the National Drug Code (NDC) Dietary supplements including medical foods Drugs for which the cost is recoverable under any federal, state, or government agency or any medication for which there is no charge made to the recipient. Drugs given by, or while the person is an inpatient in, any healthcare facility; or for any drugs provided on an outpatient basis in any such institution to the extent benefits are payable for it. Drugs given or entirely consumed at the time and place it is prescribed or dispensed. Drugs or medications that include the same active ingredient or a modified version of an active ingredient and: - Is therapeutically equivalent or therapeutically alternative to a covered Prescription Drug (unless medical exception is approved), or - Is therapeutically equivalent or therapeutically alternative to an over-the-counter (OTC) product (unless medical exception is approved). Drugs recently approved by the U.S. Food and Drug Administration (FDA), but which have not yet been reviewed by Aetna's Pharmacy and Therapeutic Committee. Drugs that include vitamins and minerals, both over-the counter (OTC) and legend, except legend pre-natal vitamins for pregnant or nursing females, liquid or chewable legend pediatric vitamins for children under age 13, and potassium supplements to prevent/treat low potassium and legend vitamins that are medically necessary for the treatment of renal disease, hyperparathyroidism or other covered conditions with prior approval from us unless recommended by the United States Preventive Services Task Force (USPSTF) Drugs used for methadone maintenance medications used for drug detoxification Drugs, services and supplies given in connection with treatment of an occupational injury or occupational illness. Drugs used primarily for the treatment of infertility, or for or related to artificial insemination, in vitro fertilization, or embryo transfer procedures, except as described in the Covered Benefits section. Drugs used for the purpose of weight gain or reduction, including but not limited to: - Stimulants; - Preparations; - Foods or diet supplements; - Dietary regimens and supplements; - Food or food supplements; - Appetite suppressants; and HI HMO-HNOSG2016COC SG Off Exchange
71 - Other medications. Drugs used for the treatment of obesity. Drugs used for the treatment of sexual dysfunction/enhancement All drugs or growth hormones used to stimulate growth and treat idiopathic short stature unless there is evidence that the member meets one or more clinical criteria detailed in our precertification and clinical policies. Drugs or medications that include the same active ingredient or a modified version of an active ingredient. Drug or medication that is therapeutically equivalent or therapeutically alternative to a covered prescription drug. Drug or medication that is therapeutically equivalent or therapeutically alternative to an over-thecounter (OTC) product. Duplicative drug therapy (e.g. two antihistamine drugs) Durable medical equipment, monitors and other equipment except as described in the Covered Benefits section. Experimental or investigational drugs or devices, except as described in the Covered Benefits section. This exclusion will not apply with respect to drugs that: - Have been granted treatment investigational new drug (IND); or Group c/treatment IND status; or - Are being studied at the Phase III level in a national clinical trial sponsored by the National Cancer Institute; and - Aetna determines, based on available scientific evidence, are effective or show promise of being effective for the illness. Food items: Except as described in the Covered Benefits section, any food item, including infant formulas, nutritional supplements, vitamins, medical foods and other nutritional items, even if it is the sole source of nutrition.. This limitation will not apply to formulas and special modified food products as specifically stated in this Certificate. Genetics: Any treatment, device, drug, or supply to alter the body s genes, genetic make-up, or the expression of the body s genes except for the correction of congenital birth defects. Immunization or immunological agents except as described in the Covered Benefits section. Immunizations related to work. Implantable drugs and associated devices, except for injectable generic contraceptives and as described in the Covered Benefits section. HI HMO-HNOSG2016COC SG Off Exchange
72 Injectables or infused drugs, except for injectable generic contraceptives and as described in the Covered Benefits section. - Any charges for the administration of an infused or injected Prescription Drug or injectable insulin and other infused or injected drugs covered by Aetna; - Certain injectable agents such as injectable contrasts/dyes used for imaging (e.g., MRI, CT, Bone Scans), except insulin; - Needles and syringes except diabetic needles and syringes, or for a covered drug; and - Injectable drugs if an alternative oral drug is available. - For any drug, which due to its characteristics as determined by us must typically be administered or supervised by a qualified provider or licensed certified health professional in an outpatient setting. This exception does not apply to Depo Provera and other injectable drugs used for contraception. Insulin pumps or tubing or other ancillary equipment and supplies for insulin pumps. Prescription drugs dispensed by a mail order pharmacy that include prescription drugs that cannot be shipped by mail due to state or federal laws or regulations, or when the plan considers shipment through the mail to be unsafe. Examples of these types of drugs include, but are not limited to, narcotics, amphetamines, DEA controlled substances and anticoagulants. Prescription drugs that include an active metabolite, stereoisomer, prodrug (precursor) or altered formulation of another drug and is no clinically superior to that drug as determined by the plan. Prescription drugs that are ordered by a dentist or prescribed by an oral surgeon in relation to the removal of teeth, or prescription drugs for the treatment of a dental condition. Prescription drugs that are considered oral dental preparations and fluoride rinses, except pediatric fluoride tablets or drops as specified on the preferred drug guide. Prescription drugs that are non-preferred drugs, unless non-preferred drugs are specifically covered as described in your schedule of benefits. However, a non-preferred drug will be covered if in the judgment of the prescriber there is no equivalent prescription drug on the preferred drug guide or the product on the preferred drug guide is ineffective in treating your disease or condition or has caused or is likely to cause an adverse reaction or harm you. That are not considered covered or related to a non-covered service. Prescription drugs that are being used or abused in a manner that is determined to be furthering an addiction to a habit-forming substance, the use of or intended use of which would be illegal, unethical, imprudent, abusive, not medically necessary, or otherwise improper; and drugs obtained for use by anyone other than the member identified on the ID card. Prescription Drugs for which there is an over-the-counter (OTC) product which has the same active ingredient even if a Prescription is written, unless Medically Necessary. Prescription Drugs, medications, injectables or supplies given through a third party vendor contract with the employer. Prescription drugs unless the drug is included on the Preferred Drug Guide (Formulary) or a medical exception is granted. HI HMO-HNOSG2016COC SG Off Exchange
73 Prescription orders filled prior to the effective date or after the termination date of coverage under this Certificate. Progesterone for the treatment of premenstrual syndrome (PMS) and compounded natural hormone therapy replacement. Prophylactic drugs for travel. Refills over the amount specified by the Prescription order. Before recognizing charges, Aetna may require a new Prescription or proof as to need, if a Prescription or refill appears excessive under accepted medical practice standards. Refills dispensed more than one year from the date the latest Prescription order was written, or as otherwise allowed by applicable law of the jurisdiction in which the drug is dispensed. Replacement of lost or stolen Prescriptions. Strength and performance: Drugs or preparations, devices and supplies to enhance strength, physical condition, endurance or physical performance, including performance enhancing steroids. Supplies, devices or equipment of any type, except as specifically provided in the Covered Benefits section. Test agents except diabetic test agents. HI HMO-HNOSG2016COC SG Off Exchange
74 TERMINATION OF COVERAGE A Member s coverage under this Certificate will terminate upon the earliest of any of the conditions listed below and termination will be effective on the date indicated on the Schedule of Benefits. Termination of Subscriber Coverage A Subscriber s coverage will terminate for any of the following reasons: Employment terminates; The Group Agreement terminates; The Subscriber is no longer eligible as outlined in this Certificate; The Subscriber becomes covered under an alternative health benefit plan or under any other plan which is offered by, through, or in connection with, the Contract Holder in lieu of coverage under this Certificate. Termination of Dependent Coverage A Covered Dependent s coverage will terminate for any of the following reasons: A Covered Dependent is no longer eligible, as outlined in this Certificate; The Group Agreement terminates; or The Subscriber s coverage terminates; Coverage of a dependent will not terminate if the Subscriber becomes enrolled under a group Medicare + Choice plan offered by Aetna or one of its affiliates. However, the dependent s coverage will terminate if the Subscriber s coverage terminates under the Medicare + Choice plan. Termination For Cause Aetna may terminate coverage for cause: Upon 60 days advance written notice, if the Contract Holder or Member has failed to make any required premium payment which the Contract Holder or Member is obligated to pay. Upon the effective date of such termination, prepayments received by Aetna on account of such terminated Member or Members for periods after the effective date of termination shall be refunded to Contract Holder. Upon 60 days advance written notice upon discovering a material misrepresentation by the Contract Holder in applying for or obtaining coverage or benefits under this Certificate or discovering that the Contract Holder has committed fraud against Aetna. A Member may register a Complaint with Aetna, as described in the Complaints and Appeals, External Review and Dispute Resolution sections of the Certificate, after receiving notice that Aetna has or will terminate the Member s coverage as described in the Termination For Cause subsection of the Certificate. Aetna will continue the Member s coverage in force until a final decision on the Complaint is rendered, provided the Premium is paid throughout the period prior to the issuance of that final decision. Aetna may rescind coverage, to the date coverage would have terminated had the Member not registered a Complaint with Aetna, if the final decision is in favor of Aetna. If coverage is rescinded, HI HMO-HNOSG2016COC SG Off Exchange
75 Aetna will provide the Member with a 60 day advance written notice prior to the date of the rescission, and refund any Premiums paid for any period after the termination date, minus the cost of Covered Benefits provided to a Member during this period. Coverage will not be terminated on the basis of a Member s health status or health care needs, nor if a Member has exercised the Member s rights under the Certificate s Complaints and Appeals, External Review, and Dispute Resolution sections to register a Complaint with Aetna. The Complaint process described in the preceding paragraph applies only to those terminations affected pursuant to the Termination for Cause subsection of the Certificate. Aetna shall have no liability or responsibility under this Certificate for services provided on or after the date of termination of coverage. The fact that Members are not notified by the Contract Holder of the termination of their coverage due to the termination of the Group Agreement shall not continue the Members' coverage beyond the date coverage terminates. CONTINUATION COBRA Continuation Coverage COBRA is the Consolidated Omnibus Budget Reconciliation Act of 1985, and related amendments ( COBRA ). The description of COBRA which follows is intended only to summarize the Member s rights under the law. Coverage provided under this Certificate offers no greater COBRA rights than COBRA requires and should be construed accordingly. COBRA permits eligible Members or eligible Covered Dependents to elect to continue group coverage as follows: Employees and their Covered Dependents will not be eligible for the continuation of coverage provided by this section if the Contract Holder is exempt from the provisions of COBRA. Minimum Size of Group: The Contract Holder must have normally employed 20 or more employees on a typical business day during the preceding calendar year. This refers to the number of employees employed, not the number of employees covered by a health plan, and includes full-time and part-time employees. Loss of coverage due to termination (other than for gross misconduct) or reduction of hours of employment: Member may elect to continue coverage for 18 months after eligibility for coverage under this Certificate would otherwise cease. Loss of coverage due to: - Divorce or legal separation, or - Subscriber's death, or - Subscriber's entitlement to Medicare benefits, or, - Cessation of Covered Dependent child status under the Eligibility and Enrollment section of this Certificate: The Member may elect to continue coverage for 36 months after eligibility for coverage under this Certificate would otherwise cease. HI HMO-HNOSG2016COC SG Off Exchange
76 Continuation coverage ends at the earliest of the following events: - The last day of the 18 month period. - The last day of the 36 month period. - The first day on which timely payment of Premium is not made subject to the Premiums section of the Group Agreement. - The first day on which the Contract Holder ceases to maintain any group health plan. - The first day, after the day COBRA coverage has been elected, on which a Member is actually covered by any other group health plan. - the date, after COBRA coverage has been elected, when the Member is entitled to Medicare. Extensions of Coverage Periods: - The 18 month coverage period may be extended if an event which would otherwise qualify the Member for the 36 month coverage period occurs during the 18 month period, but in no event may coverage be longer than 36 months from the event which qualified the Member for continuation coverage initially. - In the event that a Member is determined, within the meaning of the Social Security Act, to be disabled and notifies the Contract Holder within 60 days of the Social Security determination and before the end of the initial 18 month period, continuation coverage for the Member and other qualified beneficiaries may be extended up to an additional 11 months for a total of 29 months. The Member must have become disabled during the first 60 days of the COBRA continuation coverage. Responsibility of the Contract Holder to provide Member with notice of Continuation Rights: The Contract Holder is responsible for providing the necessary notification to Members, within the defined time period, as required by COBRA. Responsibility to pay Premiums to Aetna: The Subscriber or Member will only have coverage for the 60 day initial enrollment period if the Subscriber or Member pays the applicable Premium charges due within 60 days of submitting the application to the Contract Holder. Premiums due Aetna for the continuation of coverage under this section shall be due in accordance with the procedures of the Premiums section of the Group Agreement and shall be calculated in accordance with applicable federal law and regulations. Extension of Benefits While Member is Receiving Inpatient Care Any Member who is receiving inpatient care in a Hospital or Skilled Nursing Facility on the date coverage under this Certificate terminates is covered in accordance with the Certificate only for the specific medical condition causing that confinement or for complications arising from the condition causing that confinement, until the earlier of: The date of discharge from such inpatient stay; Determination by the Aetna Medical Director in consultation with the attending Physician, that care in the Hospital or Skilled Nursing Facility is no longer Medically Necessary; HI HMO-HNOSG2016COC SG Off Exchange
77 The date the contractual benefit limit has been reached; The date the Member becomes covered for similar coverage from another health benefits plan; or 12 months of coverage under this extension of benefits provision. The extension of benefits shall not extend the time periods during which a Member may enroll for continuation of coverage, expand the benefits for such coverage, nor waive the requirements concerning the payment of Premium for such coverage. Extension of Benefits Upon Total Disability Any Member who is Totally Disabled on the date coverage under this Certificate terminates is covered in accordance with the Certificate. This extension of benefits shall only: Provide Covered Benefits that are necessary to treat medical conditions causing or directly related to the disability as determined by Aetna; and Remain in effect until the earlier of the date that: - The Member is no longer Totally Disabled; - The Member has exhausted the Covered Benefits available for treatment of that condition; - The Member has become eligible for coverage from another health benefit plan which does not exclude coverage for the disabling condition; or - After a period of 12 months in which benefits under such coverage are provided to the Member. The extension of benefits shall not extend the time periods during which a Member may enroll for continuation coverage, expand the benefits for such coverage, nor waive the requirements concerning the payment of Premium for such coverage. HI HMO-HNOSG2016COC SG Off Exchange
78 CLAIMS PROCEDURE, COMPLAINTS AND APPEALS AND EXTERNAL REVIEW/DISPUTE RESOLUTION CLAIM PROCEDURES A claim occurs whenever a Member or the Member s authorized representative requests precertification as required by the plan from Aetna, or requests payment for services or treatment received. As an Aetna Member, most claims do not require forms to be submitted. However, if a Member receives a bill for Covered Benefits, the bill must be submitted promptly to the Aetna for payment. Send the itemized bill for payment with the Member s identification number clearly marked to the address shown on the Member s ID card. Aetna will make a decision on the Member s claim. Notice of the benefit determination on the claim will be provided to the Member within the below timeframes. Under certain circumstances, these time frames may be extended. If Aetna makes an adverse benefit determination, notice will be provided in writing to the Member, or in the case of a concurrent care claim, to the Participating Provider. The notice will provide important information about making an Appeal of the adverse benefit determination. Please see the Certificate for more information about Appeals. Adverse benefit determinations are decisions made by Aetna that result in denial, reduction, or termination of a benefit or the amount paid for it. It also means a decision not to provide a benefit or service or termination of a Member's coverage back to the original effective date (rescission). Such adverse benefit determination may be based on: Your eligibility for coverage. Coverage determinations, including plan limitations or exclusions. The results of any Utilization Review activities. A decision that the service or supply is an Experimental or Investigational Procedure. A decision that the service or supply is not Medically Necessary. A final adverse benefit determination is an adverse benefit determination that has been upheld by Aetna at the exhaustion of the appeals process. Aetna Timeframe for Notification of a Benefit Determination Type of Claim Urgent Care Claim. A claim for medical care or treatment where delay could seriously jeopardize the life or health of the Member, the ability of the Member to regain maximum function; or subject the Member to severe pain that cannot be adequately managed without the requested care or treatment. Response Time from Receipt of Claim As soon as possible, but not later than 72 hours after the claim is made. If more information is needed to make an Urgent Care Claim decision, Aetna will notify the claimant within 72 hours of receipt of the claim. The claimant has 48 hours after receiving such notice to provide Aetna with the additional information. Aetna will notify the claimant within 48 hours of the earlier to occur: the receipt of the additional information; or the end of the 48 hour period given the Physician to provide Aetna with the information. HI HMO-HNOSG2016COC SG Off Exchange
79 Pre-Service Claim. A claim for a benefit that requires precertification of the benefit in advance of obtaining medical care. Concurrent Care Claim Extension. A request to extend a course of treatment previously precertified by Aetna. Concurrent Care Claim Reduction or Termination. Decision to reduce or terminate a course of treatment previously precertified by Aetna. Post-Service Claim. A claim for a benefit that is not a pre-service claim. Within 15 calendar days. Aetna may determine that due to matters beyond its control an extension of this 15 calendar day claim decision period is required. Such an extension, of no longer than 15 additional calendar days, will be allowed if Aetna notifies the Member within the first 15 calendar day period. If this extension is needed because Aetna needs more information to make a claim decision, the notice of the extension shall specifically describe the required information. The Member will have 45 calendar days, from the date of the notice, to provide Aetna with the required information. If an urgent care claim as soon as possible, but not later than 24 hours provided the request is received at least 24 hours prior to the expiration of the approved course of treatment. A decision will be provided not later than 15 calendar days with respect to all other care, following a request for a Concurrent Care Claim Extension. With enough advance notice to allow the Member to file an Appeal. If the Member files an Appeal, Covered Benefits under the Certificate will continue for the previously approved course of treatment until a final Appeal decision is rendered. During this continuation period, the Member is responsible for any Copayments and Deductibles that apply to the services; supplies; and treatment; that are rendered in connection with the claim that is under Appeal. If Aetna's initial claim decision is upheld in the final Appeal decision, the Member will be responsible for all charges incurred for services; supplies; and treatment; received during this continuation period. Within 30 calendar days. Aetna may determine that due to matters beyond its control an extension of this 30 calendar day claim decision period is required. Such an extension, of not longer than 15 additional calendar days, will be allowed if Aetna notifies the Member within the first 30 calendar day period. If this extension is needed because Aetna needs more information to make a claim decision, the notice of the extension shall specifically describe the required information. The Member will have 45 calendar days, from the date of the notice, to provide Aetna with the required information. HI HMO-HNOSG2016COC SG Off Exchange
80 COMPLAINTS AND APPEALS Aetna has procedures for Members to use if they are dissatisfied with a decision that the Aetna has made or with the operation of the Aetna. The procedure the Member needs to follow will depend on the type of issue or problem the Member has. Appeal. An Appeal is a request to the Aetna to reconsider an adverse benefit determination. The Appeal procedure for an adverse benefit determination has two level(s). Complaint. A Complaint is an expression of dissatisfaction about the quality of care or the operation of the Aetna. External Review. A review of an adverse benefit determination or a final adverse benefit determination by an Independent Review Organization/External Review Organization (ERO) that is Federally approved and made up of Physicians or other appropriate Providers. The ERO must have expertise in the problem or question involved. Complaints If the Member is dissatisfied with the administrative services the Member receives from the Aetna or wants to complain about a Participating Provider, call or write Member Services. The Member will need to include a detailed description of the matter and include copies of any records or documents that the Member thinks are relevant to the matter. The Aetna will review the information and provide the Member with a written response within 30 calendar days of the receipt of the Complaint, unless additional information is needed and it cannot be obtained within this time frame. The response will tell the Member what the Member needs to do to seek an additional review. Full and Fair Review of Claim Determinations and Appeals Aetna will provide the Member with any new or additional evidence considered and rationale, relied upon, or generated by us in connection with the claim at issue. This will be provided to the Member in advance of the date on which the notice of the final adverse benefit determination is required to be provided so that the Member may respond prior to that date. Prior to issuing a final adverse benefit determination based on a new or additional rationale, the Member must be provided, free of charge, with the rationale; the rationale must be provided as soon as possible and sufficiently in advance of the date on which notice of final adverse determination is required. Appeals of Adverse Benefit Determinations The Member will receive written notice of an adverse benefit determination from the Aetna. The notice will include the reason for the decision and it will explain what steps must be taken if the Member wishes to Appeal. The notice will also identify the Member s rights to receive additional information that may be relevant to an Appeal. Requests for an Appeal must be made in writing within 180 calendar days from the date of the notice. A Member may also choose to have another person (an authorized representative) make the Appeal on the Member s behalf by providing the Aetna with written consent. However, in case of an urgent care claim or a pre-service claim, a Physician may represent the Member in the Appeal. A Member may be allowed to provide evidence or testimony during the Appeal process in accordance with the guidelines established by the Federal Department of Health and Human Services. HI HMO-HNOSG2016COC SG Off Exchange
81 The Aetna provides for two level(s) of Appeal of the adverse benefit determination. A final adverse benefit determination notice may provide an option to request an External Review (if available). If the Member decides to Appeal to the second level, the request must be made in writing within 60 calendar days from the date of the notice. The following chart summarizes some information about how the Appeals are handled for different types of claims. Aetna Timeframe for Responding to an Adverse Benefit Determination Appeal Type of Claim Urgent Care Claim. A claim for medical care or treatment where delay could seriously jeopardize the life or health of the Member, the ability of the Member to regain maximum function; or subject the Member to severe pain that cannot be adequately managed without the requested care or treatment. Level One Appeal Aetna Response Time from Receipt of Appeal Within 36 hours Review provided by Aetna personnel not involved in making the adverse benefit determination. Level Two Appeal Aetna Response Time from Receipt of Appeal Within -36 hours Review provided by Aetna Appeals Committee. Review provided by Aetna personnel not involved in making the adverse benefit determination or Level One Appeal decision. Pre-Service Claim. A claim for a benefit that requires approval of the benefit in advance of obtaining medical care. Concurrent Care Claim Extension. A request to extend or a decision to reduce a previously approved course of treatment. Post-Service Claim. Any claim for a benefit that is not a pre-service claim. Within 15 calendar days Review provided by Aetna personnel not involved in making the adverse benefit determination. Treated like an urgent care claim or a preservice claim depending on the circumstances. Within 30 calendar days Review provided by Aetna personnel not involved in making the adverse benefit determination. Within 15 calendar days Review provided by Aetna Appeals Committee. Review provided by Aetna personnel not involved in making the adverse benefit determination or Level One Appeal decision. Treated like an urgent care claim or a preservice claim depending on the circumstances Within 30 calendar days Review provided by Aetna Appeals Committee. Review provided by Aetna personnel not involved in making the adverse benefit determination or Level One Appeal decision. HI HMO-HNOSG2016COC SG Off Exchange
82 A Member and/or an authorized representative may attend the Level Two Appeal hearing and question the representative of Aetna and/or any other witnesses, and present their case. The hearing will be informal. A Member s Physician or other experts may testify. Aetna also has the right to present witnesses. Exhaustion of Process The foregoing procedures and process are mandatory and must be exhausted prior to: Any investigation of a Complaint or Appeal by the Arizona Department of Insurance; or The filing of a Complaint or Appeal with the Arizona Department of Insurance; or The establishing of any litigation or arbitration, or any administrative proceeding regarding either any alleged breach of the Group Agreement or Certificate by Aetna, or any matter within the scope of the Complaints and Appeals process. Under certain circumstances a Member may seek simultaneous review through the internal Appeals Procedure and External Review processes these include Urgent Care Claims and situations where the Member is receiving an ongoing course of treatment. Exhaustion of the applicable process of the Appeal Procedure is not required under these circumstances. Important Note: If Aetna does not adhere to all claim determination and Appeal requirements of the Federal Department of Health and Human Services, the Member is considered to have exhausted the Appeal requirements and may proceed with External Review or any of the actions mentioned above. There are limits, though, on what sends a claim or an appeal straight to an External Review. A Member's claim or internal Appeal will not go straight to External Review if: A rule violation was minor and isn't likely to influence a decision or harm the Member; It was for a good cause or was beyond Aetna's control; and It was part of an ongoing, good faith exchange between the Member and Aetna. Record Retention Aetna shall retain the records of all Complaints and Appeals for a period of at least 10 years. Fees and Costs Nothing herein shall be construed to require Aetna to pay counsel fees or any other fees or costs incurred by a Member in pursuing a Complaint or Appeal. HI HMO-HNOSG2016COC SG Off Exchange
83 EXTERNAL REVIEW The Member may receive an adverse benefit determination or final adverse benefit determination notice because Aetna determines that: The claim involves medical judgment; The service or supply is not Medically Necessary or appropriate; The service or supply is an Experimental or Investigational Procedure;. In of these situations, Members may request an External Review if the Member or the Member s Provider disagrees with Aetna s decision. To request an External Review, any of the following requirements must be met: The Member received an adverse benefit determination notice by Aetna, and Aetna did not adhere to all claim determination and appeal requirements of the Federal Department of Health and Human services. The Member has received a final adverse benefit determination notice of the denial of a claim by Aetna. The Member s claim was denied because Aetna determined that the care was not Medically Necessary or appropriate or was an Experimental or Investigational Procedure. The Member qualifies for a faster review as explained below. Aetna s notice of adverse benefit determination or final adverse benefit determination describes the process to follow if the Member wishes to pursue an External Review and includes a copy of the Request for External Review Form. The Member must submit the Request for External Review Form: To Aetna Within 4 months of the date you received the decision from us And you must include a copy of the notice from us and all other important information that supports your request They will contact the ERO that will conduct the review of the Member s claim. The ERO will select one or more independent clinical reviewers with appropriate expertise to perform the review. In making a decision, the external reviewer may consider any appropriate credible information that the Member sends along with the Request for External Review Form, and will follow Aetna s contractual documents and plan criteria governing the benefits. The ERO will notify you of the decision within 45 calendar days of Aetna s receipt of the Member s request form and all the necessary information. A faster review is possible if the Member s Physician certifies (by telephone or on a separate Request for External Review Form) that a delay in receiving the service would: Seriously jeopardize the Member s life or health; or Jeopardize the Member s ability to regain maximum function; or If the Adverse Benefit Determination relates to an Experimental or Investigational Procedure treatment, if the Physician certifies that the recommended or requested health care service, supply or treatment would be significantly less effective if not promptly initiated. HI HMO-HNOSG2016COC SG Off Exchange
84 The Member may also receive a faster review if the final adverse benefit determination relates to an admission; availability of care; continued inpatient confinement; or health service for which the Member received Emergency Service, but has not been discharged from a facility. Within one business day after receiving a request for this type of expedited external independent review we shall acknowledge receipt of the request to you and your treating provider. We will forward the request and all the required documentation to the director to initiate the expedited review. Faster reviews are decided within 72 hours after the external reviewer receives the request. Aetna will abide by the decision of the ERO, except where Aetna can show conflict of interest, bias or fraud. The Member is responsible for the cost of compiling and sending the information that they wish to be reviewed by the ERO to Aetna. Aetna is responsible for the cost of sending this information to the ERO and for the cost of the external review. For more information about the Complaints and Appeals or External Review processes, call the Member Services telephone number shown on the Member s ID card. HI HMO-HNOSG2016COC SG Off Exchange
85 DISPUTE RESOLUTION Any controversy, dispute or claim between Aetna on the one hand and one or more Interested Parties on the other hand arising out of or relating to the Group Agreement or Group Policy, whether stated in tort, contract, statute, claim for benefits, bad faith, professional liability or otherwise ("Claim"), shall be settled by confidential binding arbitration administered by the American Arbitration Association ("AAA") before a sole arbitrator ("Arbitrator"). Judgment on the award rendered by the Arbitrator ("Award") may be entered by any court having jurisdiction thereof. If the AAA declines to administer the case and the parties do not agree on an alternative administrator, a sole neutral arbitrator shall be appointed upon petition to a court having jurisdiction. Aetna and Interested Parties hereby give up their rights to have Claims decided in a court before a jury. Any Claim alleging wrongful acts or omissions of Participating or non-participating Providers shall not include Aetna. A Member must exhaust all Complaint, Appeal and independent external review procedures prior to the commencement of an arbitration hereunder. No person may recover any damages arising out of or related to the failure to approve or provide any benefit or coverage beyond payment of or coverage for the benefit or coverage where (i) Aetna has made available independent external review and (ii) Aetna has followed the reviewer's decision. Punitive damages may not be recovered as part of a Claim under any circumstances. No Interested Party may participate in a representative capacity or as a member of any class in any proceeding arising out of or related to the Group Agreement or Group Policy. This agreement to arbitrate shall be specifically enforced even if a party to the arbitration is also a party to another proceeding with a third party arising out of the same matter. COORDINATION OF BENEFITS Definitions. When used in this provision, the following words and phrases have the following meaning: Allowable Expense. A health care service or expense, including Deductibles, coinsurance and Copayments, that is covered at least in part by any of the Plans covering the Member. When a Plan provides benefits in the form of services the reasonable cash value of each service will be considered an Allowable Expense and a benefit paid. This Plan limits coordination of healthcare services or expenses with those services or expenses that are covered under similar types of Plans, e.g. coordination with Medical/Pharmacy coverage is coordinated with Medical/Pharmacy Plans. An expense or service that is not covered by any of the Plans is not an Allowable Expense. The following are examples of expenses and services that are not Allowable Expenses: If a Member is confined in a private Hospital room, the difference between the cost of a semiprivate room in the Hospital and the private room (unless the Member s stay in the private Hospital room is Medically Necessary in terms of generally accepted medical practice, or one of the Plans routinely provides coverage of Hospital private rooms) is not an Allowable Expense. If a Member is covered by 2 or more Plans that compute their benefit payments on the basis of Reasonable Charge, any amount in excess of the highest of the Reasonable Charges for a specific benefit is not an Allowable Expense. If a Member is covered by 2 or more Plans that provide benefits or services on the basis of negotiated fees, an amount in excess of the highest of the negotiated fees is not an Allowable Expense, unless the Secondary Plan s provider s contract prohibits any billing in excess of the provider s agreed upon rates. HI HMO-HNOSG2016COC SG Off Exchange
86 The amount a benefit is reduced by the Primary Plan because a Member does not comply with the Plan provisions. Examples of these provisions are second surgical opinions, precertification of admissions, and preferred provider arrangements. If a Member is covered by 1 Plan that calculates its benefits or services on the basis of Reasonable Charges and another Plan that provides its benefits or services on the basis of negotiated fees, the Primary Plan s payment arrangements shall be the Allowable Expense for all the Plans. Claim Determination Period(s). Usually, the calendar year. Closed Panel Plan(s). A Plan that provides health benefits to Members primarily in the form of services through a panel of Providers that have contracted with or are employed by the Plan, and that limits or excludes benefits for services provided by other Providers, except in cases of Emergency Services or Referral by a panel Provider. Coordination of Benefits (COB). A provision that is intended to avoid claims payment delays and duplication of benefits when a person is covered by 2 or more Plans. It avoids claims payment delays by establishing an order in which Plans pay their claims and providing the authority for the orderly transfer of information needed to pay claims promptly. It may avoid duplication of benefits by permitting a reduction of the benefits of a Plan when, by the rules established by this provision, it does not have to pay its benefits first. Custodial Parent. A parent awarded custody by a court decree. In the absence of a court decree, it is the parent with whom the child resides more than one half of the calendar year without regard to any temporary visitation. Medicare. The health insurance provided by Title XVIII of the Social Security Act, as amended. It includes Aetna or similar coverage that is an authorized alternative to Parts A and B of Medicare. Plan(s). Any Plan providing benefits or services by reason of medical or dental care or treatment, which benefits or services are provided by one of the following: Group, blanket, or franchise health insurance policies issued by insurers, including health care service contractors; Other prepaid coverage under service plan contracts, or under group or individual practice; Uninsured arrangements of group or group-type coverage; Labor-management trusteed plans, labor organization plans, employer organization plans, or employee benefit organization plans; Medical benefits coverage in a group, group-type, and individual automobile no-fault and traditional automobile fault type contracts; Medicare or other governmental benefits; Other group-type contracts. Group type contracts are those which are not available to the general public and can be obtained and maintained only because membership in or connection with a particular organization or group. If the Plan includes both medical and dental coverage, those coverages will be considered separate Plans. The Medical/Pharmacy coverage will be coordinated with other Medical/Pharmacy Plans. In turn, the dental coverage will be coordinated with other dental Plans. HI HMO-HNOSG2016COC SG Off Exchange
87 Plan Expenses. Any necessary and reasonable health expenses, part or all of which are covered under this Plan. Primary Plan/Secondary Plan. The order of benefit determination rules state whether coverage under this Certificate is a Primary Plan or Secondary Plan as to another Plan covering the Member. When coverage under this Certificate is a Primary Plan, its benefits are determined before those of the other Plan and without considering the other Plan s benefits. When coverage under this Certificate is a Secondary Plan, its benefits are determined after those of the other Plan and may be reduced because of the other Plan s benefits. When there are more than 2 Plans covering the person, coverage under this Certificate may be a Primary Plan as to 1 or more other Plans, and may be a Secondary Plan as to a different Plan(s). This Coordination of Benefits (COB) provision applies to this Certificate when a Subscriber or the Covered Dependent has medical and/or dental coverage under more than 1 Plan. The Order of Benefit Determination Rules below determines which Plan will pay as the Primary Plan. The Primary Plan pays first without regard to the possibility that another Plan may cover some expenses. A Secondary Plan pays after the Primary Plan and may reduce the benefits it pays. Order of Benefit Determination When 2 or more Plans pay benefits, the rules for determining the order of payment are as follows: The Primary Plan pays or provides its benefits as if the Secondary Plan(s) did not exist. A Plan that does not contain a COB provision that is consistent with this provision is always primary. There is one exception: coverage that is obtained by virtue of membership in a group that is designed to supplement a part of a basic package of benefits may provide that the supplementary coverage shall be excess to any other parts of the Plan provided by the Contract Holder. Examples of this type of exception are major medical coverage s that are superimposed over base plan providing Hospital and surgical benefits, and insurance type coverage s that are written in connection with a Closed Panel Plan to provide out-of-network benefits. A Plan may consider the benefits paid or provided by another Plan in determining its benefits only when it is secondary to that other Plan. The first of the following rules that describes which Plan pays its benefits before another Plan is the rule which will govern: Non-Dependent or Dependent. The Plan that covers the person other than as a dependent, for example as an employee, Subscriber or retiree is primary and the Plan that covers the person as a dependent is secondary. However, if the person is a Medicare beneficiary and, as a result of federal law, Medicare is secondary to the Plan covering the person as a dependent; and primary to the Plan covering the person as other than a dependent (e.g. a retired employee); then the order of benefits between the 2 Plans is reversed so that the Plan covering the person as an employee, Subscriber or retiree is secondary and the other Plan is primary. Dependent Child Covered Under More Than One Plan. The order of benefits when a child is covered by more than one Plan is: The Primary Plan is the Plan of the parent whose birthday is earlier in the year if: HI HMO-HNOSG2016COC SG Off Exchange
88 - The parents are married; - The parents are not separated (whether or not they ever have been married); or - A court decree awards joint custody without specifying that 1 party has the responsibility to provide health care coverage. If both parents have the same birthday, the Plan that covered either of the parents longer is primary. If the specific terms of a court decree state that one of the parents is responsible for the child s health care expenses or health care coverage and the Plan of that parent has actual knowledge of those terms, that Plan is primary. This rule applies to Claim Determination Periods or Plan years commencing after the Plan is given notice of the court decree. If the parents are not married, or are separated (whether or not they ever have been married) or are divorced, the order of benefits is: - The Plan of the Custodial Parent; - The Plan of the spouse of the Custodial Parent; - The Plan of the non-custodial parent; and then - The Plan of the spouse of the non-custodial parent. Active or Inactive Employee. The Plan that covers a person as an employee who is neither laid off nor retired, is the Primary Plan. The same holds true if a person is a dependent of a person covered as a retiree and an employee. If the other Plan does not have this rule, and if, as a result, the Plans do not agree on the order of benefits, this rule is ignored. Coverage provided to an individual as a retired worker and as a dependent of an actively working spouse will be determined under this section. Continuation Coverage. If a person whose coverage is provided under a right of continuation provided by federal or state law also is covered under another Plan, the Plan covering the person as an employee, Subscriber or retiree (or as that person s dependent) is primary, and the continuation coverage is secondary. If the other Plan does not have this rule, and if, as a result, the Plans do not agree on the order of benefits, this rule is ignored. Longer or Shorter Length of Coverage. The Plan that covered the person as an employee, Member or Subscriber longer is primary. If the preceding rules do not determine the Primary Plan, the Allowable Expenses shall be shared equally between the Plan s meeting the definition of Plan under this section. In addition, this Plan will not pay more than it would have paid had it been primary. Effect on Benefits of this Certificate When this Plan is secondary, it may reduce its benefits so that the total benefits paid or provided by all Plans during a Claim Determination Period are not more than 100% of total Allowable Expenses. The difference between the benefit payments that this Plan would have paid had it been the Primary Plan, and the benefit payments that it actually paid or provided shall be recorded as a benefit reserve for the Member and used by this Plan to pay any Allowable Expenses, not otherwise paid during the claim determination period. As each claim is submitted, this Plan will: Determine its obligation to pay or provide benefits under its contract; Determine whether a benefit reserve has been recorded for the Member; and HI HMO-HNOSG2016COC SG Off Exchange
89 Determine whether there are any unpaid Allowable Expenses during that Claim Determination Period. If a Member is enrolled in 2 or more Closed Panel Plans and if, for any reason, including the provision of service by a non-panel provider, benefits are not payable by 1 Closed Panel Plan, COB shall not apply between that Plan and other Closed Panel Plans. Effect of Medicare The following provisions explain how the benefits under this Certificate interact with benefits available under Medicare. A Member is eligible for Medicare if Member: Is covered under Medicare by reason of age, disability, or End Stage Renal Disease; If a Member is enrolled in for Medicare, coverage under this Certificate will be determined as follows: If a Member s coverage under this Certificate is based on current employment with the Contract Holder, coverage under this Certificate will act as the primary payor for the Medicare beneficiary who is eligible for Medicare: Solely due to age if this Plan is subject to the Social Security Act requirements for Medicare with respect to working aged (i.e., generally a plan of an employer with 20 or more employees); Due to diagnosis of End Stage Renal Disease, but only during the first 30 months of such eligibility for Medicare benefits. But this does not apply if at the start of such eligibility the Member was already eligible for Medicare benefits and this Plan s benefits were payable on a Secondary Plan basis; Solely due to any disability other than End Stage Renal Disease; but only if this Plan meets the definition of a large group health plan in the Internal Revenue Code (i.e., generally a plan of an employer with 100 or more employees). Otherwise, coverage under this Certificate will cover the benefits as the Secondary Plan. Coverage under this Certificate will pay the difference between the benefits of this Plan and the benefits that Medicare pays, up to 100% of Plan Expenses. Charges used to satisfy a Member s Part B deductible under Medicare will be applied under this Plan in the order received by Aetna. Two or more charges received at the same time will be applied starting with the largest first. Any rule for coordinating other plan benefits with those under this Plan will be applied after this Plan s benefits have been figured under the above rules. Those charges for non-emergency care or treatment furnished by a Member s Physician under a Private Contract are excluded. A Private Contract is a contract between a Medicare beneficiary and a Physician who has decided not to provide services through Medicare. HI HMO-HNOSG2016COC SG Off Exchange
90 This exclusion applies to services an opt out Physician has agreed to perform under a Private Contract signed by the Member. Physicians who have decided not to provide services through Medicare must file an opt out affidavit with all carriers who have jurisdiction over claims the Physician would otherwise file with Medicare and be filed no later than 10 days after the first private contract to which the affidavit applies is entered into with a Medicare beneficiary. Multiple Coverage Under this Plan If a Member is covered under this Plan both as a Subscriber and a Covered Dependent or as a Covered Dependent of 2 Subscribers, the following will also apply: The Members coverage in each capacity under this Plan will be set up as a separate Plan. The order in which various Plans will pay benefits will apply to the Plans set up above and to all other Plans. This provision will not apply more than once to figure the total benefits payable to the person for each claim under this Plan. Right to Receive and Release Needed Information Certain facts about health care coverage and services are needed to apply these COB rules and to determine benefits under this Plan and other Plans. Aetna has the right to release or obtain any information and make or recover any payments it considers necessary in order to administer this provision. Facility of Payment Any payment made under another Plan may include an amount which should have been paid under coverage under this Certificate. If so, Aetna may pay that amount to the organization, which made that payment. That amount will then be treated as though it were a benefit paid under this Certificate. Aetna will not have to pay that amount again. The term payment made means reasonable cash value of the benefits provided in the form of services. Right of Recovery If the amount of the payments made by Aetna is more than it should have paid under this COB provision, it may recover the excess from one or more of the persons it has paid or for whom it has paid; or any other person or organization that may be responsible for the benefits or services provided for the Member. The amount of the payments made includes the reasonable cash value of any benefits provided in the form of services. RECOVERY RIGHTS RELATED TO WORKERS COMPENSATION If medical benefits are provided by Aetna for illness or injuries to a Member and Aetna determines the Member received Workers Compensation benefits for the same incident that resulted in the illness or injuries, Aetna has the right to recover as described under the Subrogation and Right of Recovery provision. Workers Compensation benefits includes benefits paid in connection with a Workers Compensation claim, whether paid by an employer directly, a workers compensation insurance carrier, or any fund designed to provide compensation for workers compensation claims. Aetna will exercise its Recovery Rights against the Member. HI HMO-HNOSG2016COC SG Off Exchange
91 The Recovery Rights will be applied even though: The Workers Compensation benefits are in dispute or are paid by means of settlement or compromise; No final determination is made that bodily injury or sickness was sustained in the course of or resulted from the Member s employment; but the Member receives a lump sum payment The amount of Workers Compensation benefits due to medical or health care is not agreed upon or defined by the Member or the Workers Compensation carrier and the Member receives a lump sum payment; or The medical or health care benefits are specifically excluded from the Workers Compensation settlement or compromise. By accepting benefits under this Plan, the Member or the Member s representatives agree to notify Aetna of any Workers Compensation claim made, and to reimburse Aetna as described above. Aetna may exercise its Recovery Rights against the Provider in the event: a) the employer or carrier is found liable or responsible according to a final adjudication of the claim; or b) an order of the Arizona Workers Compensation Board approving a settlement agreement is entered; or the Provider has previously been paid by the carrier directly, resulting in duplicate payment. RESPONSIBILITY OF MEMBERS Members or applicants shall complete and submit to Aetna such application or other forms or statements as Aetna may reasonably request. Members represent that all information contained in such applications, forms and statements submitted to Aetna incident to enrollment under this Certificate or the administration herein shall be true, correct, and complete to the best of the Member s knowledge and belief. The Member shall notify Aetna immediately of any change of address for the Member or any of the Subscriber s Covered Dependents, unless a different notification process is agreed to between Aetna and Contract Holder. The Member understands that Aetna is acting in reliance upon all information provided to it by the Member at time of enrollment and afterwards and represents that information so provided is true and accurate. By electing coverage pursuant to this Certificate, or accepting benefits hereunder, all Members who are legally capable of contracting, and the legal representatives of all Members who are incapable of contracting, at time of enrollment and afterwards, represent that all information so provided is true and accurate and agree to all terms, conditions and provisions in this Certificate. Members are subject to and shall abide by the rules and regulations of each Provider from which benefits are provided. HI HMO-HNOSG2016COC SG Off Exchange
92 GENERAL PROVISIONS Identification Card The identification card issued by Aetna to Members pursuant to this Certificate is for identification purposes only. Possession of an Aetna identification card confers no right to services or benefits under this Certificate, and misuse of such identification card may be grounds for termination of Member s coverage pursuant to the Termination of Coverage section of this Certificate. If the Member who misuses the card is the Subscriber, coverage may be terminated for the Subscriber as well as any of the Covered Dependents. To be eligible for services or benefits under this Certificate, the holder of the card must be a Member on whose behalf all applicable Premium charges under this Certificate have been paid. Any person receiving services or benefits which such person is not entitled to receive pursuant to the provisions of this Certificate shall be charged for such services or benefits at billed charges. If any Member permits the use of the Member s Aetna identification card by any other person, such card may be retained by Aetna, and all rights of such Member and their Covered Dependents, if any, pursuant to this Certificate shall be terminated immediately, subject to the Claim Procedures/Complaints and Appeals/Dispute Resolution in this Certificate. Reports and Records Aetna is entitled to receive from any Provider of services to Members, information reasonably necessary to administer this Certificate subject to all applicable confidentiality requirements as defined in the General Provisions section of this Certificate. By accepting coverage under this Certificate, the Subscriber, for himself or herself, and for all Covered Dependents covered hereunder, authorizes each and every Provider who renders services to a Member hereunder to: Disclose all facts pertaining to the care, treatment and physical condition of the Member to Aetna, or a medical, dental, or mental health professional that Aetna may engage to assist it in reviewing a treatment or claim; Render reports pertaining to the care, treatment and physical condition of the Member to Aetna, or a medical, dental, or mental health professional that Aetna may engage to assist it in reviewing a treatment or claim; and Permit copying of the Member s records by Aetna. Refusal of Treatment A Member may, for personal reasons, refuse to accept procedures, medicines, or courses of treatment recommended by a Participating Provider. If the Participating Provider (after a second Participating Provider s opinion, if requested by Member) believes that no professionally acceptable alternative exists, and if after being so advised, Member still refuses to follow the recommended treatment or procedure, neither the Participating Provider, nor Aetna, will have further responsibility to provide any of the benefits available under this Certificate for treatment of such condition or its consequences or related conditions. Aetna will provide written notice to Member of a decision not to provide further benefits for a particular condition. This decision is subject to the Claim Procedures/Complaints and Appeals/Dispute Resolution in this Certificate. Coverage for treatment of the condition involved will be resumed in the event Member agrees to follow the recommended treatment or procedure. HI HMO-HNOSG2016COC SG Off Exchange
93 Assignment of Benefits All rights of the Member to receive benefits hereunder are personal to the Member and may not be assigned. Legal Action No action at law or in equity may be maintained against Aetna for any expense or bill unless and until the appeal process has been exhausted, and in no event prior to the expiration of 60 days after written submission of claim has been furnished in accordance with requirements set forth in the Group Agreement. No action shall be brought after the expiration of 3 years after the time written submission of claim is required to be furnished. Independent Contractor Relationship Participating Providers, non-participating Providers, institutions, facilities or agencies are neither agents nor employees of Aetna. Neither Aetna nor any Member of Aetna is an agent or employee of any Participating Provider, non-participating Provider, institution, facility or agency. Neither the Contract Holder nor a Member is the agent or representative of Aetna, its agents or employees, or an agent or representative of any Participating Provider or other person or organization with which Aetna has made or hereafter shall make arrangements for services under this Certificate. Participating Physicians maintain the physician-patient relationship with Members and are solely responsible to Member for all Medical Services which are rendered by Participating Physicians. Aetna cannot guarantee the continued participation of any Provider or facility with Aetna. In the event a Participating Provider terminates its contract or is terminated by Aetna, Aetna shall provide notification to Members in the following manner: - Within 30 days of the termination of a Participating Provider contract to each affected Subscriber, if the Subscriber or any Dependent of the Subscriber is currently enrolled in the Participating Provider s office; and - Services rendered by a PCP or Hospital to an enrollee after the date of termination of the Provider Agreement are Covered Benefits only if the services or supplies were furnished during a Member s confinement and the confinement began prior to the date of the termination. Restriction on Choice of Providers: Unless otherwise approved by Aetna, Members must utilize Participating Providers and facilities who have contracted with Aetna to provide services. HI HMO-HNOSG2016COC SG Off Exchange
94 Inability to Provide Service If due to circumstances not within the reasonable control of Aetna, including but not limited to, major disaster, epidemic, complete or partial destruction of facilities, riot, civil insurrection, disability of a significant part of the Participating Provider Network, the provision of medical or Hospital benefits or other services provided under this Certificate is delayed or rendered impractical, Aetna shall not have any liability or obligation on account of such delay or failure to provide services, except to refund the amount of the unearned prepaid Premiums held by Aetna on the date such event occurs. Aetna is required only to make a good-faith effort to provide or arrange for the provision of services, taking into account the impact of the event. Confidentiality Information contained in the medical records of Members and information received from any Provider incident to the provider-patient relationship shall be kept confidential in accordance with applicable law. Information may be used or disclosed by Aetna when necessary for a Member s care or treatment, the operation of Aetna and administration of this Certificate, or other activities, as permitted by applicable law. Members can obtain a copy of Aetna s Notice of Information Practices by calling the Member Services toll-free telephone number listed on the Member s identification card. Limitation on Services Except in cases of Emergency Services or Urgent Care, or as otherwise provided under this Certificate, services are available only from Participating Providers and Aetna shall have no liability or obligation whatsoever on account of any service or benefit sought or received by a Member from any Physician, Hospital, Skilled Nursing Facility, home health care agency, or other person, entity, institution or organization unless prior arrangements are made by Aetna. Incontestability In the absence of fraud, all statements made by a Member shall be considered representations and not warranties, and no statement shall be the basis for voiding coverage or denying a claim after the Group Agreement has been in force for 2 years from its effective date, unless the statement was material to the risk and was contained in a written application. Additional Provisions The following additional provisions apply to your coverage: This Certificate applies to coverage only, and does not restrict a Member s ability to receive health care benefits that are not, or might not be, Covered Benefits. Contract Holder hereby makes Aetna coverage available to persons who are eligible under the Eligibility and Enrollment section of this Certificate. However, this Certificate shall be subject to amendment, modification or termination in accordance with any provision hereof, by operation of law. This can also be done by mutual written agreement between Aetna and Contract Holder without the consent of Members. However, any and all amendments initialed by Aetna will be done after 60 days written notice is provided to Contract Holder. HI HMO-HNOSG2016COC SG Off Exchange
95 Aetna may adopt policies, procedures, rules and interpretations to promote orderly and efficient administration of this Certificate. No agent or other person, except an authorized representative of Aetna, has authority to waive any condition or restriction of this Certificate, to extend the time for making a payment, or to bind Aetna by making any promise or representation or by giving or receiving any information. No change in this Certificate shall be valid unless evidenced by an endorsement to it signed by an authorized representative of Aetna. This Certificate, including the Schedule of Benefits and any amendments, endorsements, inserts, or attachments, constitutes the entire Certificate between the parties hereto pertaining to the subject matter hereof and supersedes all prior and contemporaneous arrangements, understandings, negotiations and discussions of the parties with respect to the subject matter hereof, whether written or oral. There are no warranties, representations, or other agreements between the parties in connection with the subject matter hereof, except as specifically set forth in this Certificate. No supplement, modification or waiver of this Certificate shall be binding unless executed in writing by authorized representatives of the parties. This Certificate has been entered into and shall be construed according to applicable state and federal law. From time to time Aetna may offer or provide Members access to discounts on health care related goods or services. While Aetna has arranged for access to these goods, services and/or third party provider discounts, the third party service providers are liable to the Members for the provision of such goods and/or services. Aetna is not responsible for the provision of such goods and/or services nor is it liable for the failure of the provision of the same. Further, Aetna is not liable to the Members for the negligent provision of such goods and/or services by third party service providers. These discounts are subject to modification or discontinuance without notice. Wellness and Other Incentives We may encourage and incent you to access certain medical services, to use online tools that enhance your coverage and services, and to continue participation as an Aetna member. You and your doctor can talk about these medical services and decide if they are right for you. We may also encourage and incent you in connection with participation and outcome related thereto in a wellness or health improvement program. Incentives include but are not limited to: modifications to copayment, deductible, or coinsurance amounts; premium discounts or rebates; contributions to a health savings account; fitness center membership reimbursement; merchandise; coupons; gift cards; debit cards; or any combination of thereof. The award of any such incentive shall not depend upon the result of a wellness or health improvement activity or upon a member's health status. HI HMO-HNOSG2016COC SG Off Exchange
96 Proof of Loss and Claims Payment The following provisions apply only as they relate to breast pump services and supplies obtained from a Non-Participating Provider under the Preventive Care Benefit. For more information refer to the Preventive Care Benefit earlier in this amendment. Proof of Loss: Written proof of loss must be furnished to Aetna within 90 days after a Member incurs expenses for Covered Benefits. Failure to furnish the proof of loss within the time required will not invalidate nor reduce any claim if it is not reasonably possible to give the proof of loss within 90 days, provided the proof of loss is furnished as soon as reasonably possible. However, except in the absence of legal capacity of the claimant, the proof of loss may not be furnished later than one year from the date when the proof of loss was originally required. A proof of loss form may be obtained from Aetna or the Contract Holder. If the Member does not receive such form before the expiration of 15 working days after Aetna receives the request, the Member shall be deemed to have complied with the requirements of this Certificate upon submitting within the time fixed in this Certificate written proof covering the occurrence, character and extent of the loss for which claim is made. Time for Payment of Claim: Benefits payable under this Certificate will be paid promptly after the receipt by Aetna of satisfactory proof of loss. If any portion of a claim is contested by Aetna, the uncontested portion of the claim will be paid promptly after the receipt of proof of loss by Aetna. Financial Sanctions Exclusions: If coverage provided under this policy violates or will violate any economic or trade sanctions, the coverage is immediately considered invalid. For example, Aetna companies cannot make payments for health care or other claims or services if it violates a financial sanction regulation. This includes sanctions related to a blocked person or a country under sanction by the United States, unless it is permitted under a written license from the Office of Foreign Asset Control (OFAC). For more information visit HI HMO-HNOSG2016COC SG Off Exchange
97 DEFINITIONS The following words and phrases when used in this Certificate shall have, unless the context clearly indicates otherwise, the meaning given to them below: Aetna Aetna Health Inc., is a Pennsylvania corporation licensed by the Arizona Department of Insurance to operate as a Health Maintenance Organization. Ambulance A vehicle that is staffed with medical personnel and equipped to transport an ill or injured person. Autism Spectrum Disorder This means one of the following disorders as defined in the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association: Autistic Disorder; Rett s Disorder; Childhood Disintegrative Disorder; Asperger's Syndrome; and Pervasive Developmental Disorder--Not Otherwise Specified. Behavioral Health Provider A licensed organization or professional providing diagnostic, therapeutic or psychological services for behavioral health conditions. Behavioral Therapy Any interactive behavioral therapies derived from evidence-based research, including but not limited to: Applied Behavior Analysis; cognitive behavioral therapy; or other therapies supported by evidence of the effective treatment of individuals diagnosed with Autism Spectrum Disorder. Biosimilar Prescription Drug(s) A biological prescription drug that is highly similar to a U.S. Food and Drug Administration (FDA) licensed reference biological Prescription Drug notwithstanding minor differences for which there are no clinically meaningful differences between the highly similar biological Prescription Drug and the reference biological Prescription Drug in terms of the safety, purity, and potency of the drug. As defined in accordance with U.S. Food and Drug Administration (FDA) regulations. Body Mass Index A practical marker that is used to assess the degree of obesity and is calculated by dividing the weight in kilograms by the height in meters squared. Brand-name Prescription Drug(s) Prescription drugs and insulin with a proprietary name assigned to it by the manufacturer or distributor and so indicated by MediSpan or any other similar publication designated by Aetna. HI HMO-HNOSG2016COC SG Off Exchange
98 Calendar Year A period of 1 year commencing on January 1 st and ending at 12:00 midnight on December 31 st. Certificate This Certificate, including the Schedule of Benefits and any amendments, endorsements, inserts, or attachments, which outlines coverage for a Subscriber and Covered Dependents according to the Group Agreement. Contract Holder An employer or organization who agrees to remit the Premiums for coverage under the Group Agreement payable to Aetna. The Contract Holder shall act only as an agent of Aetna Members in the Contract Holder's group, and shall not be the agent of Aetna for any purpose. Copayment The specified dollar amount or percentage required to be paid by or on behalf of a Member in connection with benefits, if any, as set forth in the Schedule of Benefits. Copayments may be changed by Aetna upon 60 days written notice to the Contract Holder prior to the annual renewal date. Cosmetic Services or supplies that alter, improve or enhance appearance. Cosmetic Surgery Any non-medically necessary surgery or procedure whose primary purpose is to improve or change the appearance of any portion of the body to improve self-esteem, but which does not restore bodily function, correct a diseased state, physical appearance, or disfigurement caused by an accident, birth defect, or correct or naturally improve a physiological function. Cosmetic Surgery includes, but is not limited to, ear piercing, rhinoplasty, lipectomy, surgery for sagging or extra skin, any augmentation or reduction procedures (e.g., mammoplasty, liposuction, keloids, rhinoplasty and associated surgery) or treatment relating to the consequences or as a result of Cosmetic Surgery. Covered Dependent Any person in a Subscriber s family who meets all the eligibility requirements of the Eligibility and Enrollment section of this Certificate has enrolled in Aetna, and is subject to Premium requirements set forth in the Premiums section of the Group Agreement. Covered Benefits Those Medically Necessary Services and supplies set forth in this Certificate, which are covered subject to all of the terms and conditions of the Group Agreement and this Certificate. Custodial Care Services and supplies that are primarily intended to help a Member meet their personal needs. Care can be Custodial Care even if it is prescribed by a Physician, delivered by trained medical personnel, or even if it involves artificial methods (or equipment) such as feeding tubes, monitors, or catheters. Examples of Custodial Care include, but are not limited to: Changing dressings and bandages, periodic turning and positioning in bed, administering oral medication, watching or protecting a Member. Care of a stable tracheostomy, including intermittent suctioning. HI HMO-HNOSG2016COC SG Off Exchange
99 Care of a stable colostomy/ileostomy. Care of stable gastrostomy/jejunostomy/nasogastric tube (intermittent or continuous) feedings. Care of a stable indwelling bladder catheter, including emptying/changing containers and clamping tubing. Respite care, adult (or child) day care, or convalescent care. Helping a Member perform an activity of daily living, such as: walking, grooming, bathing, dressing, getting in and out of bed, toileting, eating, or preparing food. Any services that an individual without medical or paramedical training can perform or be trained to perform. Deductible The first payments up to a specified dollar amount which a Member must make in the applicable calendar year for Covered Benefits. Dentist A legally qualified Dentist or a Physician licensed to do the dental work he or she performs. Dental Provider This is: Any dentist; Group; Organization; Dental facility; or Other institution or person; that is legally qualified to furnish dental services or supplies. Detoxification The process whereby an alcohol or drug intoxicated or alcohol or drug dependent person is assisted, in a facility licensed by the appropriate regulatory authority, through the period of time necessary to eliminate, by metabolic or other means, the intoxicating alcohol or drug, alcohol or drug dependent factors or alcohol in combination with drugs as determined by a licensed Physician, while keeping the physiological risk to the patient at a minimum. Durable Medical Equipment (DME) Equipment, as determined by Aetna, which is a) made for and mainly used in the treatment of a disease or injury; b) made to withstand prolonged use; c) suited for use while not confined as an inpatient in the Hospital; d) not normally of use to persons who do not have a disease or injury; e) not for use in altering air quality or temperature; and f) not for exercise or training. Effective Date of Coverage The commencement date of coverage under this Certificate as shown on the records of Aetna. Emergency Service Professional health services that are provided to treat a Medical Emergency. HI HMO-HNOSG2016COC SG Off Exchange
100 E-visit A telephone or internet-based consult with a Provider that has contracted with Aetna to offer these services. Experimental or Investigational Procedures Services or supplies that are, as determined by Aetna, experimental. A drug, device, procedure or treatment will be determined to be experimental if: There are insufficient outcomes data available from controlled clinical trials published in the peerreviewed literature to substantiate its safety and effectiveness for the illness or injury involved; or Approval required by the U. S. Food and Drug Administration (FDA) has not been granted for marketing; or A recognized national medical or dental society or regulatory agency has determined, in writing, that it is experimental or investigational, or for research purposes; or It is a type of drug, device, procedure, or treatment that is the subject of a Phase I or Phase II clinical trial or the experimental or research arm of a Phase III clinical trial, using the definition of phases indicated in regulations and other official actions and publications of the FDA and Department of Health and Human Services; or The written protocol or protocols used by the treating facility, or the protocol or protocols of any other facility studying substantially the same drug, device, procedure, or treatment, or the written informed consent used by the treating facility or by another facility studying the same drug, device, procedure, or treatment states that it is experimental or investigational, or for research purposes. Generic Prescription Drug(s) Prescription drugs and insulin, whether identified by its chemical, proprietary, or non-proprietary name, that is accepted by the U.S. Food and Drug Administration as therapeutically equivalent and interchangeable with drugs having an identical amount of the same active ingredient and so indicated by MediSpan or any other similar publication designated by Aetna. Group Agreement The Group Agreement between Aetna and the Contract Holder, including the Group Application, this Certificate, including the Schedule of Benefits and any amendments, endorsements, inserts, or attachments, as subsequently amended by operation of law and as filed with and approved by the applicable public authority. Habilitation Health care services that help a person keep, learn, or improve skills and functioning for daily living. Examples include therapy for a child who isn't walking or talking at the expected age. These services may include physical and occupational therapy, speech-language pathology and other services for people with disabilities in a variety of inpatient and/or outpatient settings. Health Professional(s) A Physician or other professional who is properly licensed or certified to provide medical care under the laws of the state where the individual practices, and who provides Medical Services which are within the scope of the individual s license or certificate. HI HMO-HNOSG2016COC SG Off Exchange
101 Homebound Member A Member who is confined to their place of residence due to an illness or injury which makes leaving the home medically contraindicated or if the act of transport would be a serious risk to their life or health. Examples where a Member would not be considered homebound are: A Member who does not often travel from home because of feebleness and/or insecurity brought on by advanced age (or otherwise). A wheelchair bound Member who could safely be transported via wheelchair accessible transport. Home Health Services Those items and services provided by Participating Providers as an alternative to hospitalization, and coordinated and precertified by Aetna. Hospice Care A program of care that is provided by a Hospital, Skilled Nursing Facility, hospice, or a duly licensed Hospice Care agency, and is approved by Aetna, and is focused on a palliative rather than curative treatment for Members who have a medical condition and a prognosis of less than 12 months to live. Hospital(s) An institution rendering inpatient and outpatient services, accredited as a Hospital by the Joint Commission on Accreditation of Health Care Organizations, the Bureau of Hospitals of the American Osteopathic Association, or as otherwise determined by Aetna as meeting reasonable standards. A Hospital may be a general, acute care, rehabilitation or specialty institution. Infertile or Infertility A disease defined by the failure to conceive a pregnancy after 12 months or more of timed intercourse or egg-sperm contact for women under age 35 (or 6 months for women age 35 or older). Institute of Excellence TM (IOE) One of a network of facilities specifically contracted with by Aetna to provide certain Transplants to Members. A facility is considered a Participating Provider only for those types of Transplants for which it has been specifically contracted. Interested Parties Means Contract Holder and Members, including any and all affiliates, agents, assigns, employees, heirs, personal representatives or subcontractors of an Interested Party. Jaw Joint Disorder This is: A Temporomandibular Joint (TMJ) dysfunction or any similar disorder of the jaw joint; or A Myofacial Pain Dysfunction (MPD); or Any similar disorder in the relationship between the jaw joint and the related muscles and nerves. L.P.N. A licensed practical or vocational nurse. HI HMO-HNOSG2016COC SG Off Exchange
102 Mail Order Pharmacy An establishment where prescription drugs are legally given out by mail or other carrier. Medical Foods This means Modified Low Protein Foods and Metabolic Formula. Medical Community A majority of Physicians who are Board Certified in the appropriate specialty. Medical Emergency The existence of a medical condition manifesting itself by acute symptoms of sufficient severity (including severe pain) such that a prudent layperson, who possesses an average knowledge of health and medicine, could reasonably expect the absence of immediate medical attention to result in (i) placing the health of the individual (or, with respect to a pregnant woman, the health of the woman and her unborn child) in serious jeopardy; (ii) serious impairment to bodily functions; or (iii) serious dysfunction of any bodily organ or part. Medical Services The professional services of Health Professionals, including medical, surgical, diagnostic, therapeutic, preventive care and birthing facility services. Medically Necessary, Medically Necessary Services, or Medical Necessity These are health care or dental services that we determine a Physician, other health care provider or Dental Provider, exercising prudent clinical judgment, would give to a patient for the purpose of: preventing; evaluating; diagnosing; or treating: an Illness; an Injury; a disease; or its symptoms. The provision of the service, supply or Prescription Drug must, as we determine, be: In accordance with generally accepted standards of medical or dental practice; Clinically appropriate, in terms of type, frequency, extent, site and duration, and considered effective for the patient's Illness, Injury or disease; and Not mostly for the convenience of the patient, Physician, other health care or Dental Provider; and And do not cost more than an alternative service or sequence of services at least as likely to produce the same therapeutic or diagnostic results as to the diagnosis or treatment of that patient's Illness, Injury, or disease. Generally accepted standards of medical or dental practice means: Standards that are based on credible scientific evidence published in peer-reviewed medical literature. They must be generally recognized by the relevant medical or dental community; Standards set forth in policy issues involving clinical judgment HI HMO-HNOSG2016COC SG Off Exchange
103 Member(s) A Subscriber or Covered Dependent as defined in this Certificate. Mental Disorders This is an illness commonly understood to be a Mental Disorder, whether or not it has a physiological basis, and for which treatment is generally provided by or under the direction of a Behavioral Health Provider such as a Psychiatrist, a psychologist or a psychiatric social worker. The following conditions are considered a Mental Disorder under this plan: Anorexia/Bulimia Nervosa. Bipolar disorder. Major depressive disorder. Obsessive compulsive disorder. Panic disorder. Pervasive Mental Developmental Disorder (including Autism). Psychotic Disorders/Delusional Disorder. Schizo-affective Disorder. Schizophrenia. Also included is any other mental condition which requires Medically Necessary treatment. Metabolic Formula Foods that are all of the following: formulated to be consumed or administered internally under the supervision of the Member s Participating Physician. processed or formulated to be deficient in one or more of the nutrients present in typical foodstuffs. administered for the medical and nutritional management of a Member who has limited capacity to metabolize foodstuffs or certain nutrients contained in the foodstuffs or who has other specific nutrient requirements as established by medical evaluation. essential to a Member s optimal growth, health and metabolic homeostasis. Modified Low Protein Foods Foods that encompass those foods described in bullets 1, 3 and 4 under the definition of Metabolic Formula, and also the following: processed or formulated to contain less than one gram of protein per unit of serving, but does not include a natural food that is naturally low in protein. Morbid Obesity A Body Mass Index that is: greater than 40 kilograms per meter squared; or equal to or greater than 35 kilograms per meter squared with a high risk comorbid medical condition, including significant cardiovascular disease, sleep apnea, or uncontrolled type-2 diabetes. National Medical Excellence Program Coordinating Aetna services team for Transplant services and other specialized care. HI HMO-HNOSG2016COC SG Off Exchange
104 Negotiated Charge As to Health Coverage, (other than Prescription Drug Coverage): The Negotiated Charge is the maximum charge a Participating Provider has agreed to make as to any service or supply for the purpose of the benefits under this plan. As to Prescription Drug Coverage: The Negotiated Charge is the amount Aetna has established for each Prescription Drug obtained from a Participating Pharmacy under this plan. This Negotiated Charge may reflect amounts Aetna has agreed to pay directly to the Participating Pharmacy or to a third party vendor for the Prescription Drug, and may include an additional service or risk charge set by Aetna. The Negotiated Charge does not include or reflect any amount Aetna, an affiliate, or a third party vendor, may receive under a rebate arrangement between Aetna, an affiliate or a third party vendor and a drug manufacturer for any Prescription Drug, including Prescription Drugs on the Preferred Drug Guide (Formulary). Based on its overall drug purchasing, Aetna may receive rebates from the manufacturers of Prescription Drugs and may receive or pay additional amounts from or to third parties under price guarantees. These amounts will not change the Negotiated Charge under this plan. Network Pharmacy Is a retail Pharmacy, mail order Pharmacy or Specialty Pharmacy that has entered into a contractual agreement with Aetna, an affiliate, or a third party vendor, to furnish services and supplies for this plan. Non-Hospital Facility A facility, licensed by the appropriate regulatory authority, for the care or treatment of alcohol or drug dependent persons, except for transitional living facilities. Non-Participating Providers These are Providers that are not Participating Providers. Non-Preferred Drug (Non-Formulary) This is a Prescription Drug or device that is not listed in the Preferred Drug Guide (Formulary). This includes prescription drugs and devices that might initially be excluded from coverage but may be approved by medical exception. Open Enrollment Period A period each calendar year, when eligible enrollees of the Contract Holder may enroll in Aetna without a waiting period or exclusion or limitation based on health status or, if already enrolled in Aetna, may transfer to an alternative health plan offered by the Contract Holder. HI HMO-HNOSG2016COC SG Off Exchange
105 Orthodontic Treatment This is any: Medical service or supply; or Dental service or supply; furnished to prevent or to diagnose or to correct a misalignment: Of the teeth; or Of the bite; or Of the jaws or jaw joint relationship; whether or not for the purpose of relieving pain. The following are not considered orthodontic treatment: The installation of a space maintainer; or A surgical procedure to correct malocclusion. Partial Hospitalization The provision of medical, nursing, counseling or therapeutic services on a planned and regularly scheduled basis in a Hospital or Non-Hospital Facility which is licensed as an alcohol or drug abuse or mental illness treatment program by the appropriate regulatory authority, and which is designed for a patient or client who would benefit from more intensive services than are offered in outpatient treatment but who does not require inpatient care. Participating A description of a Provider that has entered into a contractual agreement with Aetna for the provision of services to Members. Participating providers are shown in the directory and in DocFind. Participating Dental Provider A Dental Provider that has entered into a contractual agreement with HMO or an affiliate for the provision of services to you. Participating Dentist A Dentist that has entered into a contractual agreement with HMO or an affiliate for the provision of services to you. Participating Infertility Specialist A Specialist who has entered into a contractual agreement with Aetna for the provision of Infertility services to Members. Physician(s) A duly licensed member of a medical profession, who has an M.D. or D.O. degree, who is properly licensed or certified to provide medical care under the laws of the state where the individual practices, and who provides Medical Services which are within the scope of the individual s license or certificate Also any practitioner who performs a service for which coverage is provided when it is performed by a Physician. HI HMO-HNOSG2016COC SG Off Exchange
106 Premium(s) The amount the Contract Holder or Member is required to pay to Aetna to continue coverage. Preferred Drug (Formulary) A Prescription Drug or device that is listed on the Preferred Drug Guide (Formulary). Preferred Drug Guide (Formulary) A listing of Prescription Drugs established by Aetna or an affiliate, which does not cover all Prescription Drugs. This list is subject to periodic review and modification by Aetna or an affiliate. A copy of the Preferred Drug Guide (Formulary) will be available upon your request or may be accessed on the Aetna website at Preferred Drug Guide Exclusions List A list of Prescription Drugs in the Preferred Drug Guide (Formulary) that are identified as excluded under the plan. This list is subject to periodic review and modification by Aetna or an affiliate. Preferred Network Pharmacy A network retail pharmacy that has contracted with Aetna, an affiliate, or a third party vendor, to provide outpatient prescription drugs to you. Prescriber Any physician or dentist, acting within the scope of his or her license, who has the legal authority to write an order for a prescription drug. Prescription As to Prescription Drugs: A written order for the dispensing of a Prescription Drug by a Provider. If it is a verbal order, it must promptly be put in writing by the Pharmacy. As to vision care: A written order for the dispensing of Prescription lenses or Prescription contact lenses by an ophthalmologist or optometrist. Prescription Drug A drug, biological, or compounded Prescription which, by State and Federal Law, may be dispensed only by Prescription. This includes: An injectable drug prescribed to be self-administered or administered by any other person except one who is acting within his or her capacity as a paid healthcare professional. Primary Care Physician (PCP) A Participating Physician who supervises, coordinates and provides initial care and basic Medical Services as a general or family care practitioner, or in some cases, as an internist or a pediatrician to Members, and maintains continuity of patient care. HI HMO-HNOSG2016COC SG Off Exchange
107 Provider(s) A Physician, Health Professional, Hospital, Skilled Nursing Facility, Dental Provider, home health agency or other recognized entity or person licensed to provide Hospital Services, Medical Services, or dental services to Members. Psychiatric Hospital This is an institution that meets all of the following requirements. Mainly provides a program for the diagnosis, evaluation, and treatment of Substance Abuse or mental disorders. Is not mainly a school or a custodial, recreational or training institution. Provides infirmary-level medical services. Also, it provides, or arranges with a Hospital in the area for, any other medical service that may be required. Is supervised full-time by a Psychiatrist who is responsible for patient care and is there regularly. Is staffed by Psychiatrists involved in care and treatment. Has a Psychiatrist present during the whole treatment day. Provides, at all times, Psychiatric social work and nursing services. Provides, at all times, Skilled Nursing Services by licensed nurses who are supervised by a full-time R.N. Prepares and maintains a written plan of treatment for each patient based on medical, psychological and social needs. The plan must be supervised by a Psychiatrist. Makes charges. Meets licensing standards. Psychiatric Physician This is a physician who: Specializes in psychiatry; or Has the training or experience to do the required evaluation and treatment of Substance Abuse or Mental Disorders. Psychiatrist This is a Physician who: Specializes in psychiatry; or Has the training or experience to do the required evaluation and treatment of Substance Abuse or Mental Disorders. Referral Specific directions or instructions from a Member s PCP, in conformance with Aetna s policies and procedures, that direct a Member to a Participating Provider for Medically Necessary care. Residential Treatment Facility (Mental Disorders) This is an institution that meets all of the following requirements: Is accredited by one of the following agencies, commissions or committees for the services being provided: The Joint Commission (TJC), Committee on Accreditation of Rehabilitation Facilities (CARF), American Osteopathic Association s Healthcare Facilities Accreditation Program (HFAP) or the Council on Accreditation (COA); or is credentialed by Aetna; Meets all applicable licensing standards established by the jurisdiction in which it is located; HI HMO-HNOSG2016COC SG Off Exchange
108 Performs a comprehensive patient assessment preferably before admission, but at least upon admission; Creates individualized active treatment plans directed toward the alleviation of the impairment that caused the admission; Has the ability to involve family/support systems in the therapeutic process; Has the level of skilled intervention and provision of care must be consistent with the patient s illness and risk; Provides access to psychiatric care by a psychiatrist as necessary for the provision of such care; Provides treatment services that are managed by a behavioral health provider who functions under the direction/supervision of a medical director; and Is not a wilderness treatment program (whether or not the program is part of a licensed residential treatment facility, or otherwise licensed institution), educational services, schooling or any such related or similar program, including therapeutic programs within a school setting. In addition to the above requirements, for Mental Health Residential Treatment Programs: A behavioral health provider must be actively on duty 24 hours per day for 7 days a week; The patient is treated by a psychiatrist at least once per week; and The medical director must be a psychiatrist. Residential Treatment Facility (Substance Abuse) This is an institution that meets all of the following requirements: Is accredited by one of the following agencies, commissions or committees for the services being provided: The Joint Commission (TJC), Committee on Accreditation of Rehabilitation Facilities (CARF), American Osteopathic Association s Healthcare Facilities Accreditation Program (HFAP), or the Council on Accreditation (COA); or is credentialed by Aetna; Meets all applicable licensing standards established by the jurisdiction in which it is located; Performs a comprehensive patient assessment preferably before admission, but at least upon admission; Creates individualized active treatment plans directed toward the alleviation of the impairment that caused the admission; Has the ability to involve family and/or support systems in the therapeutic process; Has the level of skilled intervention and provision of care that is consistent with the patient s illness and risk; Provides access to psychiatric care by a psychiatrist as necessary for the provision of such care; Provides treatment services that are managed by a behavioral health provider who functions under the direction/supervision of a medical director; and Is not a wilderness treatment program (whether or not the program is part of a licensed residential treatment facility, or otherwise licensed institution), educational services, schooling or any such related or similar program, including therapeutic programs within a school setting. In addition to the above requirements, for Chemical Dependence Residential Treatment Programs: Is a behavioral health provider or an appropriately state certified professional (for example, CADC, CAC); Is actively on duty during the day and evening therapeutic programming; and The medical director must be a physician who is an addiction specialist. In addition to the above requirements, for Chemical Dependence Detoxification Programs within a residential setting: An R.N. is onsite 24 hours per day for 7 days a week; and The care must be provided under the direct supervision of a physician. HI HMO-HNOSG2016COC SG Off Exchange
109 Retail Pharmacy A community pharmacy which has contracted with Aetna, an affiliate, or a third party vendor, to provide covered outpatient Prescription Drugs to you. Self-injectable Drug(s) Prescription drugs that are intended to be self-administered by injection to a specific part of the body to treat certain chronic medical conditions. Service Area The geographic area established by Aetna and approved by the appropriate regulatory authority. Skilled Care Medical care that requires the skills of technical or professional personnel. Skilled Nursing Services that require the medical training of and are provided by a licensed nursing professional and are not Custodial Care. Skilled Nursing Facility An institution or a distinct part of an institution that is licensed or approved under state or local law, and which is primarily engaged in providing Skilled Nursing care and related services for residents who require medical or nursing care, or rehabilitation services for the rehabilitation of injured, disabled, or sick persons. Skilled Nursing Facility does not include institutions which provide only minimal care, Custodial Care services, ambulatory or part-time care services, or institutions which primarily provide for the care and treatment of Mental Disorder and Substance Abuse. The facility must qualify as a Skilled Nursing Facility under Medicare or as an institution accredited by the Joint Commission on Accreditation of Health Care Organizations, the Bureau of Hospitals of the American Osteopathic Association, the Commission on the Accreditation of Rehabilitative Facilities, or as otherwise determined by the health insurer to meet the reasonable standards applied by any of the aforesaid authorities. Examples of Skilled Nursing Facilities include Rehabilitation Hospitals (all levels of care, e.g. acute) and portions of a Hospital designated for Skilled or Rehabilitation services. Specialist(s) A Physician who provides medical care in any generally accepted medical or surgical specialty or subspecialty. Specialty Care Health care services or supplies that require the services of a specialist. Specialty Care Prescription Drugs These are Prescription Drugs that include self- injectable, infusion and oral drugs prescribed to address complex, chronic diseases with associated co-morbidities such as: Cancer Rheumatoid arthritis Hemophilia Human immunodeficiency virus infection HI HMO-HNOSG2016COC SG Off Exchange
110 Multiple sclerosis You can access the list of these Specialty care Prescription Drugs by calling the toll-free Member Services number on your member ID card or by logging on to your Aetna Navigator secure member website at The list also includes Biosimilar Prescription Drugs. Specialty Pharmacy Pharmacies designated to fill Prescriptions for Self-injectable Drugs and Specialty Care Prescription Drugs. Step Therapy Program A form of precertification under which certain prescription drugs will be excluded from coverage, unless a first-line therapy drug(s) is used first by the Member. The list of step therapy drugs is subject to change by Aetna. An updated copy of the list of drugs subject to step therapy shall be available upon request by the Member or may be accessed at the Aetna website, at Subscriber A person who meets all applicable eligibility requirements as described in this Certificate has enrolled in Aetna, and is subject to Premium requirements as set forth in the Premiums section of the Group Agreement. Substance Abuse Any use of alcohol and/or drugs which produces a pattern of pathological use causing impairment in social or occupational functioning or which produces physiological dependency evidenced by physical tolerance or withdrawal. Substance Abuse Rehabilitation Services, procedures and interventions to eliminate dependence on or abuse of legal and/or illegal chemical substances, according to individualized treatment plans. Surgery or Surgical Procedure The diagnosis and treatment of injury, deformity and disease by manual and instrumental means, such as cutting, abrading, suturing, destruction, ablation, removal, lasering, introduction of a catheter (e.g., heart or bladder catheterization) or scope (e.g., colonoscopy or other types of endoscopy), correction of fracture, reduction of dislocation, application of plaster casts, injection into a joint, injection of sclerosing solution, or otherwise physically changing body tissues and organs. Telemedicine A telephone or internet-based consult with a Provider that has contracted with Aetna to offer these services. Therapeutic Drug Class A group of drugs or medications that have a similar or identical mode of action or exhibit similar or identical outcomes for the treatment of a disease or injury. HI HMO-HNOSG2016COC SG Off Exchange
111 Tier 1 A group of medications determined by us that may be available at a reduced copayment/coinsurance and are noted on the Preferred Drug Guide (Formulary) on the Aetna website at Totally Disabled or Total Disability A Member shall be considered Totally Disabled if: The Member is a Subscriber and is prevented, because of injury or disease, from performing any occupation for which the Member is reasonably fitted by training, experience, and accomplishments; or The Member is a Covered Dependent and is prevented because of injury or disease, from engaging in substantially all of the normal activities of a person of like age and sex in good health. Transplant Replacement of solid organs; stem cells; bone marrow or tissue. Transplant Occurrence Considered to begin at the point of authorization for evaluation for a Transplant, and end: (1) 180 days from the date of the Transplant; or (2) upon the date the Member is discharged from the Hospital or outpatient facility for the admission or visit(s) related to the Transplant, whichever is later. Urgent Care Non-preventive or non-routine health care services which are Covered Benefits and are required in order to prevent serious deterioration of a Member s health following an unforeseen illness, injury or condition if: (a) the Member is temporarily absent from the Aetna Service Area and receipt of the health care service cannot be delayed until the Member returns to the Aetna Service Area; or, (b) the Member is within the Aetna Service Area and receipt of the health care services cannot be delayed until the Member s Primary Care Physician is reasonably available. Urgent Care Facility A facility licensed as a freestanding medical facility by applicable state and federal laws to treat an urgent condition. Walk-in Clinic A Participating free-standing health care facility. Neither of the following should be considered a Walk-in Clinic: An emergency room; nor The outpatient department of a Hospital; HI HMO-HNOSG2016COC SG Off Exchange
112 PCP and PCP referred coverage (in-network) under the Health Maintenance Organization (HMO) plan Schedule of Benefits If this is an ERISA plan, Members have certain rights under this plan. If the Contract Holder is a church group or a government group this may not apply. Please contact the Contract Holder for additional information. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [1] AZ SG-off HNO AZ Silver HNOption R
113 Schedule of Benefits This Schedule of Benefits lists the Deductibles and Copayments or Coinsurance, if any, that apply to the services Members receive under this plan. Members should review this schedule to become familiar with Deductibles and Copayments or Coinsurance and any limits that apply to the services. How to read the Schedule of Benefits Members are responsible to pay any Deductibles and Copayments or Coinsurance. Members are responsible for full payment of any health care services received that are not a Covered Benefit. This plan has limits for specific Covered Benefits. For example, these could be visit, day or dollar limits. They may be combined limits between or separate limits for Participating Providers and Non- Participating Providers unless we state otherwise. Important note: All Covered Benefits are subject to the Deductible and Copayment or Coinsurance unless otherwise noted in the Schedule of Benefits below. For answers to any questions, contact Member Services by logging onto the Aetna Navigator secure member website at or at the toll-free number on the Member s ID card. The coverage described in this Schedule of Benefits will be provided under Aetna Health Inc. s Group Agreement. This Schedule of Benefits replaces any Schedule of Benefits previously in effect under the Group Agreement. Keep this Schedule of Benefits with the Certificate. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [2] AZ SG-off HNO AZ Silver HNOption R
114 Plan features Cost share/deductible/limits In-network coverage* Deductible Members have to meet their Deductible before this plan pays for benefits. Individual Family $1,500 per Calendar Year $3,000 per Calendar Year Deductible waiver The Deductible is waived for all of the following Eligible Health Services: Preventive care and wellness Family planning services - female contraceptives Nutritional supplements including Medical Foods to Treat Inherited Metabolic Disorders and Formulas to Treat Eosinophilic Gastrointestinal Disorders Maximum Out-of-Pocket Limit Maximum Out-of-Pocket Limit per Calendar Year Individual Family $6,850 per Calendar Year $13,700 per Calendar Year General coverage provisions This section provides detailed explanations about the: Deductible Maximum Out-of-Pocket Limits Limits that are listed in this Schedule of Benefits. Deductible Provisions Covered Benefits applied to the out-of-network Deductibles will not be applied to satisfy the innetwork Deductibles. Covered Benefits applied to the in-network Deductibles will not be applied to satisfy the out-of-network Deductibles. The Deductible may not apply to certain Covered Benefits. You must pay any applicable Copayments or Coinsurance for Covered Benefits to which the Deductible does not apply. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [3] AZ SG-off HNO AZ Silver HNOption R
115 Individual This is the amount you owe for Covered Benefits each Calendar Year before the plan begins to pay for Covered Benefits. This Calendar Year Deductible applies separately to you and each Covered Dependent. After the amount you pay for Covered Benefits reaches the Calendar Year Deductible, this plan will begin to pay for Covered Benefits for the rest of the Calendar Year. Family This is the amount you owe for Covered Benefits each Calendar Year before the plan begins to pay the Covered Benefits. After the amount you pay for Covered Benefits reaches this family Calendar Year Deductible, this plan will begin to pay for Covered Benefits that the you and your Covered Dependents incur for the rest of the Calendar Year. To satisfy this family Deductible limit for the rest of the Calendar Year, the following must happen: The combined Covered Benefits that you and each Covered Dependent incur towards the individual Calendar Year Deductibles must reach this family Deductible limit in a Calendar Year. When this occurs in a Calendar Year, the individual Calendar Year Deductibles for you and your Covered Dependents will be considered to be met for the rest of the Calendar Year. Copayments Copayment As it applies to in-network coverage, this is a specified dollar amount or percentage that you must pay at the time Covered Benefits are received from a Participating Provider. As it applies to in-network coverage, if Aetna compensates Participating Providers on the basis of the reasonable amount, your cost share is based on this amount. Per admission Copayment A per admission Copayment is an amount required to be paid when you have a stay as an inpatient in an inpatient facility. Separate Copayments and Deductibles may apply per facility. These Copayments and Deductibles are in addition to any other Copayments and Deductibles applicable under this plan. They may apply to each inpatient stay or they may apply on a per day basis up to a per admission limit amount. If you are in the same type of facility more than once, and the inpatient stay is separated by less than 48 hours (regardless of cause), only one per admission Copayment or Deductible will apply. Not more than three per admission Copayments or Deductibles will apply for each facility type during a Calendar Year. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [4] AZ SG-off HNO AZ Silver HNOption R
116 Coinsurance The specific percentage you have to pay for a health care service listed in the Schedule of Benefits. Separate Coinsurance and Deductibles may apply per facility. These Coinsurance and Deductibles are in addition to any other Coinsurance and Deductibles applicable under this plan. They may apply to each inpatient stay or they may apply on a per day basis up to a per admission limit amount. If you are in the same type of facility more than once, and the inpatient stay is separated by less than 48 hours (regardless of cause), only one per admission Coinsurance and Deductibles will apply. Not more than three per admission Coinsurance and Deductibles will apply for each facility type during a Calendar Year. Maximum Out-of-Pocket Limits Provisions Covered Benefits that are subject to the Maximum Out-of-Pocket Limit include Prescription Drug Covered Benefits provided under the medical plan and the Outpatient Prescription Drug plan. Covered Benefits applied to the Out-of-Network Maximum Out-of-Pocket Limit will not be applied to satisfy the in-network Maximum Out-of-Pocket Limit and Covered Benefits applied to the in-network Maximum Out-of-Pocket Limit will not be applied to satisfy the Out-of-Network Maximum Out-of- Pocket Limit. The Maximum Out-of-Pocket Limit is the maximum amount you are responsible to pay for Copayments, Coinsurance and Deductibles for Covered Benefits during the Calendar Year. This plan has an individual and family Maximum Out-of-Pocket Limit. As to the individual Maximum Out-of- Pocket Limit, each covered person must meet their Maximum Out-of-Pocket Limit separately. Individual Once the amount of the Copayments, Coinsurance and Deductibles you or your Covered Dependents have paid for Covered Benefits during the Calendar Year meets the individual Maximum Out-of- Pocket Limit, this plan will pay 100% of the Covered Benefits that apply toward the limit for the rest of the Calendar Year for that person. Family Once the amount of the Copayments or Coinsurance and Deductibles you or your Covered Dependents have paid for Covered Benefits during the Calendar Year meets this family Maximum Out-of-Pocket Limit, this plan will pay 100% of the Covered Benefits that apply toward the limit for the remainder of the Calendar Year for all covered family members. The Maximum Out-of-Pocket Limit may not apply to certain Covered Benefits. If the Maximum Outof-Pocket Limit does not apply to a Covered Benefits, your Copayment or Coinsurance for that Covered Benefit will not count toward satisfying the Maximum Out-of-Pocket Limit amount. Certain costs that you incur do not apply toward the Maximum Out-of-Pocket Limit. These include: As it applies to Out-of-Network coverage: Charges, expenses or costs in excess of the Recognized Charge All costs for non-covered services Certain other Covered Benefits in the Schedule of Benefits Calculations; Determination of Recognized Charge; determination of Benefits Provisions Your responsibility for the costs of services will be calculated on the basis of when the service or supply is provided, not when payment is made. Benefits will be pro-rated to account for treatment or portions of stays that occur in more than one Calendar Year. Determinations regarding when benefits are covered are subject to the terms and conditions of the plan. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [5] AZ SG-off HNO AZ Silver HNOption R
117 Eligible Health Services In-network coverage* 1. Preventive care and wellness Routine physical exams- Performed at a Physician, PCP office Preventive care immunizations- Performed in a facility or at a Physician office Well woman preventive visits-- routine gynecological exams (including pap smears)- Performed at a Physician, PCP, obstetrician (OB), gynecologist (GYN) or OB/GYN office Screening and counseling services - Includes obesity and/or healthy diet counseling, misuse of alcohol and/or drugs, use of tobacco products, sexually transmitted infection counseling, genetic risk counseling for breast and ovarian cancer - Office visits Tobacco Cessation Prescription and Over-the-Counter Drugs, for each thirty day supply filled at a retail pharmacy Routine cancer screenings - (applies whether performed at a Physician, PCP, Specialist office or facility) Prenatal Care - (provided by an obstetrician (OB), gynecologist (GYN), and/or OB/GYN) Comprehensive lactation support and counseling services - Facility or office visits Family planning services Female Contraceptives Preventive care and wellness (as described above) 0% per visit Preventive care and wellness benefit limitations Routine physical exams Limitations-Child Subject to any age and visit limits provided for in the comprehensive guidelines supported by the American Academy of Pediatrics/Bright Futures/Health Resources and Services Administration guidelines for children and adolescents. For details, contact the Physician. Limitations - Adult Preventive care immunizations Limitations 1 visit Subject to any age limits provided for in the comprehensive guidelines supported by Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention For details, contact the Physician. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [6] AZ SG-off HNO AZ Silver HNOption R
118 Well woman preventive visits Routine gynecological exams (including pap smears) Limitations Subject to any age limits provided for in the comprehensive guidelines supported by the Health Resources and Services Administration. Screening and counseling services: limitations are per Calendar Year unless stated Obesity and/or healthy diet Coverage is limited to: age 0-22, unlimited visits; age 22+, 26 visits every 12 months, of which up to 10 visits may be used for healthy diet counseling. Misuse of alcohol and/or drugs Use of tobacco products Sexually transmitted infection Coverage is limited to 5 visits every 12 months. Coverage is limited to 8 visits every 12 months. Coverage is limited to 2 visits every 12 months. Genetic risk counseling for breast and ovarian cancer Not subject to any age or frequency limitations Tobacco Cessation Prescription and Over-the-Counter Drugs For each 30 day supply filled at a retail pharmacy 0% per prescription or refill Maximums: Coverage is permitted for two, 90-day treatment regimens only. Any additional treatment regimens will be paid according to the tier of drug per the schedule of benefits, above. Coverage only includes generic drug when a brand-name drug is available. Coverage will be subject to any sex, age, medical condition, family history, and frequency guidelines in the recommendations of the United States Preventive Services Task Force. For details on the guidelines and the current list of covered tobacco cessation Prescription Drugs and OTC drugs, contact Member Services by logging onto the Aetna Navigator secure member website at or calling the number on the back of the Member ID card. Routine cancer screenings Limitations: Subject to any age; family history; and frequency guidelines as set forth in the most current: Evidence-based items that have in effect a rating of A or B in the current recommendations of the United States Preventive Services Task Force; and The comprehensive guidelines supported by the Health Resources and Services Administration. Any lung cancer screenings that exceed the lung cancer screening maximum above are covered under the Outpatient diagnostic testing section. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [7] AZ SG-off HNO AZ Silver HNOption R
119 Comprehensive lactation support and counseling services Lactation counseling services maximum visits per Calendar Year either in a group or individual setting Any visits that exceed the lactation counseling services maximum are covered under Physician services office visits. Coverage is limited to 6 visits Breast feeding durable medical equipment Important note: Members should review the Maternity and related newborn care section. This will give more information on coverage levels for maternity care under this plan. See the Breast feeding durable medical equipment section of the Certificate for limitations on breast pump and supplies. Family planning services female contraceptives Contraceptive counseling services maximum visits per Calendar Year either in a group or individual setting Coverage is limited to 2 visits Eligible Health Services In-network coverage* 2. Physicians and other health professionals Physician services Office hours visits (non-surgical) $30 per visit non preventive care No Deductible applies Allergy injections Without Physician, PCP or Specialist office Allergy testing and treatment Performed at a Physician, PCP or Specialist office Covered according to the type of benefit and the place where the service is received. Covered according to the type of benefit and the place where the service is received. Immunizations when not part of the physical exam Immunizations when not part of the physical exam Covered according to the type of benefit and the place where the service is received. Injectable medications Performed at a Physician, PCP or Specialist office Covered according to the type of benefit and the place where the service is received. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [8] AZ SG-off HNO AZ Silver HNOption R
120 Physician surgical services Performed at a Physician or Specialist office Alternatives to Physician office visits Walk-in clinic visits Walk-In Clinic non-emergency visit (includes coverage for immunizations.) Limitations Covered according to the type of benefit and the place where the service is received. $30 per visit No Deductible applies Subject to any age limits provided for in the comprehensive guidelines supported by Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention For details, contact the Physician. Individual screening and counseling services* Includes obesity and/or healthy diet counseling, use of tobacco products and stress management services Individual screening and counseling services $0 per visit No Deductible applies Refer to the Preventive care and wellness section earlier in this Schedule of Benefits for limits that may apply to these types of services. *Important note: Not all preventive care and stress management services are available at all Walk-in Clinics. The types of services offered will vary by the Provider and location of the clinic. These services may also be obtained from a Participating Physician. E-Visits and Telemedicine consultations E-visit online consultation by a Physician, PCP Telemedicine consultation by a Physician, PCP E-visit online consultation by a Specialist Telemedicine consultation by a Specialist Specialist office visits Office hours visit (non-surgical) Covered according to the type of benefit and the place where the service is received. $30 per visit No Deductible applies Covered according to the type of benefit and the place where the service is received. $30 per visit No Deductible applies $60 per visit No Deductible applies *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [9] AZ SG-off HNO AZ Silver HNOption R
121 Eligible Health Services 3. Hospital and other facility care Hospital care Inpatient Hospital Skilled nursing facility Inpatient facility Day limit per Calendar Year Outpatient surgery Performed in Hospital outpatient department Performed in facility other than Hospital outpatient department Home health care Outpatient In-network coverage* 30% (of the Negotiated Charge) per admission 30% (of the Negotiated Charge) per admission 90 days 40% (of the Negotiated Charge) per visit 30% (of the Negotiated Charge) per visit $60 per visit No Deductible applies Hospice Inpatient facility and other Hospice benefits during a stay Hospice Outpatient 30% (of the Negotiated Charge) per admission $60 per visit No Deductible applies Eligible Health Services In-network coverage* 4. Emergency Care and Urgent Care A separate Hospital emergency room or Urgent Care Deductible or Copayment will apply for each visit to an emergency room or an Urgent Care Facility. Hospital emergency room $250 per visit No Deductible applies Non-emergency care in a Hospital emergency room Not Covered *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [10] AZ SG-off HNO AZ Silver HNOption R
122 Important note: As Non-Participating Providers do not have a contract with Aetna the Provider may not accept payment of the Member s cost share, (Deductible, Copayment and Coinsurance), as payment in full. The Member may receive a bill for the difference between the amount billed by the Provider and the amount paid by this plan. If the Provider bills the Member for an amount above the Member s cost share, the Member is not responsible for paying that amount. The Member should send the bill to the address listed on the back of the Member ID card, and Aetna will resolve any payment dispute with the Provider over that amount. Make sure the Member's ID number is on the bill. If the Member is admitted to a Hospital as an inpatient right after a visit to an emergency room, the Member s emergency room Deductible or Copayment will be waived and the inpatient Deductible or Copayment will apply. Urgent medical care at a non-hospital free standing facility Non-urgent use of Urgent Care Facility at a non- Hospital free standing facility $70 per visit No Deductible applies Not Covered *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [11] AZ SG-off HNO AZ Silver HNOption R
123 Eligible Health Services 5. Specific conditions Maternity and related newborn care Inpatient and other maternity and related newborn care services and supplies In-network coverage* 30% (of the Negotiated Charge) per admission For in-network services, any Copayment that is collected applies to the delivery and postpartum care services provided by an OB's, GYN's, or OB/GYN s only. No Copayment that is collected applies to prenatal care services provided by an OB's, GYN's, or OB/GYN s. See the Prenatal care sections for cost-sharing and limits that apply to these services. Delivery services and postpartum care services Performed in a facility or at a Physician office Covered according to the type of benefit and the place where the service is received. Other prenatal care services Reconstructive breast surgery Reconstructive breast surgery Covered according to the type of benefit and the place where the service is received. Covered according to the type of benefit and the place where the service is received. Reconstructive or cosmetic services and supplies Reconstructive surgery and supplies Mental Disorders Covered according to the type of benefit and the place where the service is received. Coverage is provided under the same terms, conditions as any other illness. Inpatient facility and other inpatient services and 30% (of the Negotiated Charge) per admission supplies Residential treatment Coverage is provided under the same terms, conditions as any other illness. Inpatient facility and other inpatient services and 30% (of the Negotiated Charge) per admission supplies Mental Disorders Coverage is provided under the same terms, conditions as any other illness. Outpatient visits to a PCP - Physician Office visits $30 per visit (non-surgical) No Deductible applies *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [12] AZ SG-off HNO AZ Silver HNOption R
124 Outpatient visits to a Specialist or Behavioral Health Provider Office visits (non-surgical) $60 per visit No Deductible applies Partial Hospitalization Treatment (at least 4 hours, but less than 24 hours per day of clinical treatment) Intensive Outpatient Program (at least 2 hours per day and at least 6 hours per week of clinical treatment). Substance Abuse Detoxification Coverage is provided under the same terms, conditions as any other illness. Outpatient $60 per visit No Deductible applies Partial hospitalization Treatment (at least 4 hours, but less than 24 hours per day of clinical treatment) Intensive Outpatient Program (at least 2 hours per day and at least 6 hours per week of clinical treatment) Rehabilitation Coverage is provided under the same terms, conditions as any other illness. Inpatient and other inpatient services and supplies 30% (of the Negotiated Charge) per admission Residential treatment Coverage is provided under the same terms, conditions as any other illness. Inpatient facility and other inpatient services and 30% (of the Negotiated Charge) per admission supplies Rehabilitation Coverage is provided under the same terms, conditions as any other illness. Outpatient visits to a PCP - Physician Office visits $30 per visit (non-surgical) No Deductible applies Outpatient visits to a Specialist or Behavioral Health Provider Office visits (non-surgical) $60 per visit No Deductible applies Partial Hospitalization Treatment (at least 4 hours, but less than 24 hours per day of clinical treatment) provided in a facility or program for treatment of Substance Abuse provided under the direction of a Physician. Intensive Outpatient Program (at least 2 hours per day and at least 6 hours per week of clinical treatment) provided in a facility or program for treatment of Substance Abuse provided under the direction of a Physician. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [13] AZ SG-off HNO AZ Silver HNOption R
125 Autism spectrum disorders, including Applied behavior analysis Outpatient visits to a PCP - Physician Office visits (non-surgical) $30 per visit No Deductible applies Outpatient visits to a Specialist or Behavioral Health Provider Office visits (non-surgical) Diabetes Diabetic equipment Diabetic supplies Diabetic education by PCP Diabetic education by Specialist Treatment of basic infertility Basic infertility $60 per visit No Deductible applies 30% (of the Negotiated Charge) per visit 30% (of the Negotiated Charge) per visit $30 per visit No Deductible applies $60 per visit No Deductible applies Covered according to the type of benefit and the place where the service is received Eligible health services Network (IOE facility) Transplant services facility and non-facility Inpatient and other inpatient services and supplies 30% (of the Negotiated Charge) per admission Outpatient Coverage at the in-network cost share is limited to IOE only. Physician services Coverage at the in-network cost share is limited to IOE only. Transplant travel and lodging expenses (expenses are for transplant recipient and companion only) Maximum benefit for travel and lodging expenses for any one transplant, including tandem transplants $10,000 $10,000 *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [14] AZ SG-off HNO AZ Silver HNOption R
126 Eligible Health Services 6. Specific therapies and tests Diagnostic and preoperative testing Diagnostic complex imaging services Complex imaging services Outpatient diagnostic lab work Lab work In-network coverage* 30% (of the Negotiated Charge) per visit $35 per visit No Deductible applies Outpatient diagnostic radiological services X-ray $65 per visit No Deductible applies Outpatient preoperative testing Performed in the outpatient department of a Hospital Performed at an outpatient facility other than outpatient department of a Hospital Covered according to the type of benefit and the place where the service is received. Covered according to the type of benefit and the place where the service is received. Clinical trial therapies (experimental or investigational treatment) Clinical trial therapies (including routine patient costs) Covered according to the type of benefit and the place where the service is received. Outpatient therapies Infusion therapy Performed in a Physician office or in a person s home Performed at outpatient facility Chemotherapy Chemotherapy Radiation therapy Radiation therapy Specialty Care Prescription Drugs Performed in a Physician office or in the home Performed at outpatient facility 30% (of the Negotiated Charge) per visit 30% (of the Negotiated Charge) per visit Covered according to the type of benefit and the place where the service is received. Covered according to the type of benefit and the place where the service is received. Covered according to the type of benefit and the place where the service is received. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [15] AZ SG-off HNO AZ Silver HNOption R
127 Short-term cardiac and pulmonary rehabilitation services Cardiac and pulmonary rehabilitation Covered according to the type of benefit and the place where the service is received. Short-Term Rehabilitation Therapy Services Outpatient Cognitive Therapy, Physical Therapy Occupational Therapy and Speech Therapy Rehabilitation Benefits Outpatient physical therapy Physical therapy 30% (of the Negotiated Charge) per visit Visit limit* per Calendar Year 60 *A visit is equal to no more than 1 hour of therapy. Visit limits are combined for outpatient physical therapy, outpatient occupational therapy and outpatient speech therapy. Outpatient occupational therapy Occupational therapy 30% (of the Negotiated Charge) per visit Visit limit* per Calendar Year 60 *A visit is equal to no more than 1 hour of therapy. Visit limits are combined for outpatient physical therapy, outpatient occupational therapy and outpatient speech therapy. Outpatient speech therapy Speech therapy 30% (of the Negotiated Charge) per visit Visit limit* per Calendar Year 60 *A visit is equal to no more than 1 hour of therapy. Visit limits are combined for outpatient physical therapy, outpatient occupational therapy and outpatient speech therapy. Spinal manipulation Spinal manipulation Visit limit per Calendar Year 20 Habilitation therapy services Therapies other than physical, occupational, and speech Visit limit* per Calendar Year 60 *A visit is equal to no more than 1 hour of therapy. $60 per visit No Deductible applies 30% (of the Negotiated Charge) per visit *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [16] AZ SG-off HNO AZ Silver HNOption R
128 Eligible health services 7. Other Covered Benefits Acupuncture Covered as a form of anesthesia in connection with a covered surgical procedure Ambulance service Ground Ambulance Air or water Ambulance Non-emergency Ambulance Disposable Outpatient Supplies Disposable Outpatient Supplies Durable Medical Equipment (DME) DME In-network coverage* $60 per visit No Deductible applies 30% (of the Negotiated Charge) per trip 30% (of the Negotiated Charge) per trip 30% (of the Negotiated Charge) per trip 30% (of the Negotiated Charge) per visit 30% (of the Negotiated Charge) per visit Family planning services - other Voluntary sterilization for males Covered according to the type of benefit and the place where the service is received. Voluntary termination of pregnancy Covered according to the type of benefit and the place where the service is received. Outpatient services Voluntary sterilization for males Covered according to the type of benefit and the place where the service is received. Voluntary termination of pregnancy Covered according to the type of benefit and the place where the service is received. Hearing aids and exams Hearing aid exams $60 per visit No Deductible applies Hearing aids Jaw Joint Disorder Jaw Joint Disorder treatment 30% (of the Negotiated Charge) per visit Covered according to the type of benefit and the place where the service is received. Bariatric Surgery Bariatric Surgery Includes Surgical Procedure and Acute Hospital Services -Facility Services 30% (of the Negotiated Charge) per admission *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [17] AZ SG-off HNO AZ Silver HNOption R
129 Nutritional supplements Medical foods to treat Inherited Metabolic Disorders Nutritional supplements 25% (of the Negotiated Charge) per item/prescription No Deductible applies Formulas to treat Eosinophilic Gastrointestinal Disorders 25% (of the Negotiated Charge) per item/prescription No Deductible applies Prosthetic devices Prosthetic devices 30% (of the Negotiated Charge) per item Vision care Pediatric vision care Coverage is limited to covered persons through the end of the month in which the person turns 19 Routine vision exams (including refraction) Performed by an ophthalmologist or optometrist $0 per visit No Deductible applies Visit limit per Calendar Year Vision care services and supplies Preferred eyeglass frames, Prescription lenses or Prescription contact lenses. Non-preferred eyeglass frames, Prescription lenses or Prescription contact lenses. Number of eyeglass frames per Calendar Year Number of Prescription lenses per Calendar Year Number of Prescription contact lenses per Calendar Year (includes non-conventional Prescription contact lenses and aphakic lenses prescribed after cataract surgery) 1 visit $0 per visit No Deductible applies 50% (of the Negotiated Charge) per item One set of eyeglass frames One pair of Prescription lenses Daily disposables: up to 3 month supply Extended wear disposable: up to 6 month supply Non-disposable Lenses: one set *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [18] AZ SG-off HNO AZ Silver HNOption R
130 Adult vision care Coverage is limited to covered persons through the end of the month in which the person turns 19 Routine vision exams (including refraction) Performed by an ophthalmologist or optometrist 0% per visit No Deductible applies Visit limit per Calendar Year 1 visit *Important note: Refer to the Vision care section in the Certificate for the explanation of these vision care supplies. As to coverage for Prescription lenses in a Contract Year, this benefit will cover either Prescription lenses for eyeglass frames or Prescription contact lenses, but not both. Coverage does not include the office visit for the fitting of Prescription contact lenses. Pediatric dental Coverage is limited to covered persons through the end of the month in which the person turns 19 Type A services 0% No Deductible applies Type B services 30% Type C services 50% Orthodontic services 50% Dental emergency limit: $75 The dental emergency limit is the most the plan will pay for health care services incurred by a Member for any one dental emergency. Dental benefits are subject to the medical plan s Deductibles and Maximum Out-of-Pocket Limits as explained on the Schedule of Benefits. Type A Services: Diagnostic and Preventive Care Visits and images (D0120) Office visit during regular office hours, for oral examination (limited to: 2 visits every 12 months) (D0160) Routine comprehensive or recall examination (limited to: 2 visits every 12 months) (D0150, D0180) Comprehensive periodontal evaluation (limited to: 2 visits every 12 months) (D0140) Problem-focused examination (limited to: 2 visits every 12 months) (D1110, D1120) Prophylaxis (cleaning) (limited to: 2 treatments per year) (D1208) Topical application of fluoride (limited to: 2 courses every 12 months) (D1206) Topical fluoride varnish (limited to: 2 courses every 12 months) (D1351) Sealants, per tooth (limited to: one application every 3 years for permanent molars) (D1352) Preventive resin restoration in a moderate to high caries risk patient-permanent tooth (limited to: one application every 3 years for permanent molars) (D0270-D0274) Bitewing images (limited to: 2 sets per 12 months) (D0210) Complete image series, including bitewings (limited to: 1 set every 3 years) *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [19] AZ SG-off HNO AZ Silver HNOption R
131 (D0330) Panoramic images (limited to: 1 set every 3 years) (D0340) Cephalometric image (D0350) Oral facial photographic images (D0470) Diagnostic models (D0277) Vertical bitewing images (limited to: 2 sets per year) (D0220, D0230) Periapical images (D0240) Intra-oral, occlusal view, maxillary or mandibular (D9110) Emergency palliative treatment per visit Note: Diagnostic procedures of: D0330, D0340, D0350 and D0470 are covered as Type A benefit for a nonvested orthodontia patient. Space maintainers (Includes all adjustments within 6 months after installation) (D1510, D1515) Fixed (unilateral or bilateral) (D1520, D1525) Removable (unilateral or bilateral) (D1550) Re-cementation of space maintainer (D1555) Removal of space maintainer Type B Services: Basic Restorative Care Visits and images (D9440) Professional visit after hours (payment will be made on the basis of services rendered the charge for the after-hours visit, whichever is greater) (D9310) Consultation (by other than the treating provider) (D9930) Treatment of complications (post-surgical) unusual circumstances, by report Images and pathology (D0250-D0260) Upper or lower jaw, extra-oral (D9610) Therapeutic drug injection, by report Oral surgery (D7111) Extraction, coronal remnants-deciduous tooth (D7140) Extraction, erupted tooth or exposed root (elevation and/or forceps removal) (D7210) Surgical removal of erupted tooth requiring removal of bone and/or resectioning of tooth (D7251) Coronal remnants (D7250) Surgical removal of erupted tooth/root tip Surgical removal of impacted teeth (D7220) Removal of impacted tooth (soft tissue) (D7230) Removal of impacted tooth (partially bony) (D7240) Removal of impacted tooth (completely bony) (D7241) Removal of impacted tooth (completely bony with unusual surgical complications) (D7510) Incision and drainage of abscess (D7450, D7451) Removal of odontogenic cyst or tumor (D7280) Other surgical procedures (D7310) Alveoplasty, in conjunction with extractions - per quadrant (D7311) Alveoplasty, in conjunction with extractions, 1 to 3 teeth or tooth spaces - per quadrant (D7320) Alveoplasty, not in conjunction with extraction - per quadrant *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [20] AZ SG-off HNO AZ Silver HNOption R
132 (D7321) Alveoplasty, not in conjunction with extractions, 1 to 3 teeth or tooth spaces - per quadrant (D7980) Sialolithotomy: removal of salivary calculus (D7983) Closure of salivary fistula (D7970) Excision of hyperplastic tissue (D7471) Removal of exostosis (D7270) Tooth re-implantation (D7272) Transplantation of tooth or tooth bud (D7260) Closure of oral fistula of maxillary sinus (D7550) Sequestrectomy (D7283) Crown exposure to aid eruption (D7530) Removal of foreign body from soft tissue (D7960) Frenectomy (D7910) Suture of soft tissue injury (D7971) Excision of pericornal gingiva Periodontics (D9951, D9952) Occlusal adjustment (other than with an appliance or by restoration) (D4341) Periodontal scaling and root planing, per quadrant (limited to 4 separate quadrants every 2 years) (D4342) Root planing and scaling 1 to 3 teeth per quadrant (limited to once per site every 2 years) (D4910) Periodontal maintenance procedures following active therapy (limited to: 4 in 12 months) (combined with prophylaxis after completion of active periodontal therapy) (D4381) Localized delivery of antimicrobial agents Endodontics (D3110-D3120) Pulp capping (D3220-D3222) Pulpotomy (D3230-D3240) Pulpal therapy (D3355-D3357) Pulpal regeneration Restorative dentistry Excludes inlays, crowns (other than prefabricated stainless steel or resin) and bridges. Multiple restorations in 1 surface will be considered as a single restoration. (D2140, D2150, D2160, D2161) Amalgam restorations - one, two three, four or more surfaces, primary or permanent teeth (D2330, D2331, D2332, D2335) Resin-based composite one, two three, four or more surfaces, anterior (D2390) Resin-based composite crown, anterior (D2391, D2392, D2393, D2394) Resin-based composite - one, two, three, four or more surfaces, posterior Pins (D2951) Pin retention per tooth, in addition to amalgam or resin restoration Crowns (when tooth cannot be restored with a filling material) (D2930-D2931) Prefabricated stainless steel (D2932) Prefabricated resin crown (excluding temporary crowns) (D2940) Protective resin *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [21] AZ SG-off HNO AZ Silver HNOption R
133 Re-cementation (D2910) Inlay (D2920) Crown (D6930) Bridge Prosthodontics Dentures and partials (D5730, D5731) Office reline, complete denture - maxillary or mandibular (D5740, D5741) Office reline, partial denture - maxillary or mandibular (D5750, D5751) Reline, complete denture - maxillary or mandibular - laboratory (D5760, D5761) Reline, partial denture - maxillary or mandibular - laboratory (D5850, D5851) Special tissue conditioning, per denture - maxillary or mandibular (D5710, D5711) Rebase complete denture - maxillary or mandibular (D5720, D5721) Rebase partial denture - maxillary or mandibular (D5410, D5411) Adjustment to complete denture (more than 6 months after installation) - maxillary or mandibular (D5421, D5422) Adjustment to partial denture (more than 6 months after installation) - maxillary or mandibular Repairs: Dentures and partial dentures D6980) Fixed partial denture repair, by report (D5510) Repair broken complete denture base (D5520) Replace missing or broken teeth complete denture (each tooth) (D5610) Repair resin denture base (D5620) Repair cast framework (D5630) Broken denture clasp, no teeth involved (D5640) Replacing missing or broken teeth, each tooth Adding teeth to existing partial denture (D5650) Each tooth (D5660) Each clasp General anesthesia and intravenous sedation Only when medically necessary and only when provided in conjunction with a covered dental surgical procedure (D9220) Deep sedation/general anesthesia first 30 minutes (D9221) Deep sedation/general anesthesia each additional 15 minutes (D9241) Intravenous conscious sedation first 301 minutes (D9242) Intravenous conscious sedation each additional 15 minutes Type C Services: Major Restorative Care Periodontics (D4261) Osseous surgery, including flap and closure, 1 to 3 teeth per quadrant (limited to 1 per site every 3 years) (D4260) Osseous surgery, including flap and closure, (limited to 1 per quadrant every 3 years) (D4270) Pedicle soft tissue graft procedure (D4277, D4278) Free soft tissue graft procedures (D4273) Subepithelial connective tissue graft procedure (including donor site surgery) *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [22] AZ SG-off HNO AZ Silver HNOption R
134 (D4210) Gingivectomy, per quadrant (limited to 1 per quadrant every 3 years) (D4211) Gingivectomy, 1 to 3 teeth per quadrant (D4240) Gingival flap procedure - per quadrant (limited to 1 per quadrant every 3 years) (D4241) Gingival flap procedure 1 to 3 teeth per quadrant (limited to 1 per site every 3 years) (D4249) Clinical crown lengthening (D4355) Full mouth debridement (limited to 1 treatment per lifetime) Endodontics (D3351, D3352, D3353) Apexification/recalcification (D3410, D3421, D3425, D3426) Apicoectomy/periradicular surgery anterior/bicuspid/molar/each additional root (D3354) Pulpal regeneration Root canal therapy including medically necessary images: (D3310) Anterior (D3320) Bicuspid (D3330) Molar Retreatment of previous root canal therapy including medically necessary images: (D3346) Anterior (D3347) Bicuspid (D3348) Molar (D3450) Root amputation (D3920) Hemisection (including any root removal) Restorative Inlays, onlays, labial veneers and crowns when provided as treatment for decay or acute traumatic injury and only when teeth cannot be restored with a filling material or when the tooth is an abutment to a fixed bridge (limited to: 1 per tooth every 5 years) Inlays/Onlays (limited to: 1 tooth every 5 years) (D2510, D2520, D2530) Inlay metallic, one, two, three surfaces (D2542, D2543, D2544) Onlay metallic, one, two, three and four or more surfaces (D2610, D2620, D2630) Inlay porcelain/ceramic, one, two, three or more surfaces (D2642, D2643, D2644) Onlay porcelain/ceramic, two, three and four or more surfaces (D2650, D2651, D2652) Inlay resin based composite, one, two, three or more surfaces (D2662, D2663, D2664) Onlay resin based composite, two, three and four or more surfaces Crowns (limited to: 1 tooth every 5 years) (D2710) Resin-based composite (D2712) 3/4 resin based composite (D2720) Resin with high noble metal (D2721) Resin with base metal (D2722) Resin with noble metal (D2740) Porcelain/ceramic substrate (D2750) Porcelain fused to noble metal (D2751) Porcelain fused to predominately base metal (limited to: 1 tooth every 5 years) (D2752) Porcelain fused to noble metal (D2790) Full cast high noble metal *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [23] AZ SG-off HNO AZ Silver HNOption R
135 (D2791) Base metal (full cast) (D2792) Noble metal (full cast) (D2780) 3/4 cast high noble metal (D2781) 3/4 cast base metal (D2782) 3/4 cast noble metal (D2783) 3/4 porcelain/ceramic (D2794) Titanium (D2950) Core build-up, including any pins (D2952,D2953) Post and core in addition to crown, indirectly fabricated (D2954) Prefabricated post and core, in addition to crown (D2980) Crown repair Prosthodontics Installation of dentures and bridges is covered only if needed to replace teeth which were not abutments to a denture or bridge/partial denture less than 5 years old. Replacement of existing bridges/partial denture or dentures (limited to: 1 every 5 years) Bridge/partial denture abutments (See Inlays/Onlays and Crowns) (limited to: 1 tooth every 5 years) Pontics (limited to: 1 tooth every 5 years) (D6210) Cast high noble metal (D6211) Cast base metal (D6212) Cast noble metal (D6214) Titanium (D6240) Porcelain fused to high noble metal (D6241) Porcelain fused to base metal (D6242) Porcelain fused to noble metal (D6245) Porcelain/ceramic (D6250) Resin with high noble (D6251) Resin with base metal (D6252) Resin with noble metal (D6545) Retainer cast metal for resin bonded fixed prosthesis (limited to: 1 tooth every 5 years) (D6548) Retainer porcelain/ceramic for resin bonded fixed prosthesis (limited to: 1 tooth every 5 years) Fixed partial denture retainers-crowns (limited to: 1 tooth every 5 years) (D6740) Porcelain/ceramic (D6750) Porcelain fused to high noble metal (D6751) Porcelain fused to base metal (D6752) Porcelain fused to noble metal (D6780) 3/4 cast high noble metal (D6781) 3/4 cast base metal (D6782) 3/4 cast noble metal (D6783) 3/4 porcelain/ceramic (D6790) Full cast high noble metal (D6791) Full cast base metal (D6792) Full cast noble metal (D6794 Titanium *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [24] AZ SG-off HNO AZ Silver HNOption R
136 (D5281) Removable partial denture (unilateral) (limited to: 1 every 5 years) One piece casting, chrome cobalt alloy clasp attachment (all types) per unit, including pontics (limited to: 1 every 5 years) Dentures and Partials (limited to: 1 every 5 years) Fees for dentures and partial dentures include relines, rebases and adjustments within 6 months after installation. Fees for relines and rebases include adjustments within 6 months after installation. Specialized techniques and characterizations are not eligible) (D5110) Complete upper denture (D5120) Complete lower denture (D5130) Immediate upper denture (D5140) Immediate lower denture (D5211, D5212) Partial upper or lower, resin base (including any conventional clasps, rests and teeth) (D5213, D5214) Partial upper or lower, cast metal base with resin saddles (including any conventional clasps, rests and teeth) Implants and implant services (Only if determined as a dental necessity and limited to 1 every 5 years) (D6010) Endosteal Implant (D6012) Surgical placement of interim implant body (D6040) Eposteal implant (D6050) Transosteal implant, including hardware (D6053) Implant supported complete denture (D6054) Implant supported partial denture (D6055) Connecting bar implant or abutment supported (D6056) Prefabricated abutment (D6058) Abutment supported porcelain ceramic crown (D6059) Abutment supported porcelain fused to high noble metal (D6060) Abutment supported porcelain fused to predominately base metal crown (D6061) Abutment supported porcelain fused to noble metal crown (D6062) Abutment supported cast high noble metal crown (D6063) Abutment supported cast predominately base metal crown (D6064) Abutment supported cast noble metal crown (D6065) Implant supported porcelain/ceramic crown (D6066) Implant supported porcelain fused to high noble metal (D6067) Implant supported metal crown (D6068) Abutment supported retainer for porcelain/ceramic fixed partial denture (D6069) Abutment supported retainer for porcelain fused to high noble metal fixed partial denture (D6070) Abutment supported retainer for porcelain fused to predominately base metal fixed partial denture (D6071) Abutment supported retainer for porcelain fused to noble metal fixed partial denture (D6072) Abutment supported retainer for cast high noble metal fixed partial denture (D6073) Abutment supported retainer for predominately base metal fixed partial denture (D6074) Abutment supported retainer for cast noble metal fixed partial denture (D6075) Implant supported retainer for ceramic fixed partial denture (D6076) Implant supported retainer for porcelain fused to high noble metal fixed partial denture *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [25] AZ SG-off HNO AZ Silver HNOption R
137 (D6077) Implant supported retainer for cast metal fixed partial denture (D6078, D6079) Implant supported complete denture, partial denture (limited to 1 every 5 years) (D6080) Implant maintenance procedures (limited to 1 every 5 years) (D6090) Repair implant prosthesis (D6091) Replacement of semi-precious or precision attachment (D6094) Abutment supported crown titanium (D6095) Repair implant abutment (D6100) Implant removal, by report (D6110, D6111) Implant/abutment supported removable denture, maxillary or mandibular (D6112, D6113) Implant/abutment supported removable denture for partially edentulous arch, maxillary or mandibular (D6114, D6115) Implant/abutment supported fixed denture for completely edentulous arch maxillary or mandibular (D6116, D6117) Implant/abutment supported fixed denture for partially edentulous arch maxillary or mandibular (D6100) Implant removal, by report (D6190) Implant index (D6194) Abutment supported retainer crown for fixed partial denture titanium Other services (D6940) Stress breakers (D6985) Interim partial denture (stayplate), anterior only (D9940) Occlusal guard, by report (limited to 1 in 12 months) (D8210) Removable appliance therapy (D8220) Fixed appliance therapy Orthodontic services Medically necessary comprehensive treatment (D8010) Limited orthodontic treatment of the primary dentition (D8020) Limited orthodontic treatment of the transitional dentition (D8030) Limited orthodontic treatment of the adolescent dentition (D8040) Limited orthodontic treatment of the adult dentition (D8050) Interceptive orthodontic treatment of the primary dentition (D8060) Interceptive orthodontic treatment of the transitional dentition (D8070) Comprehensive orthodontic treatment of the transitional dentition (D8080) Comprehensive orthodontic treatment of the adolescent dentition (D8090) Comprehensive treatment of adult dentition (D8660) Pre-orthodontic treatment examination to monitor growth and development (D8670) Periodic orthodontic treatment visit (as part of contract) (D8680) Orthodontic retention (removal of appliances, construction and placement of retainer(s) (D8691) Repair of orthodontic appliance (D8693) Rebonding or recementing; and/or repair, as required of fixed retainers (D8694) Repair of fixed retainers Orthodontic treatment (includes removal of appliance, construction and placement of retainer) Replacement of retainer (limited to: 1 per lifetime) *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [26] AZ SG-off HNO AZ Silver HNOption R
138 Note: Benefits for codes D0330, D0340, D0350, and D0470 will be considered orthodontia when performed as part of orthodontic treatment. All other services for which cost sharing is not shown above All other services Covered according to the type of benefit and the place where service is received. Eligible Health Services 8. Outpatient Prescription Drugs Deductible/Copayment/Coinsurance/ Maximums Deductible and Copayment or Coinsurance waiver for risk reducing breast cancer drugs The Calendar Year Deductible and the per prescription Copayment or Coinsurance will not apply to risk reducing breast cancer Prescription Drugs when obtained at a network pharmacy. This means that such risk reducing breast cancer Prescription Drugs will be paid at 100%. Deductible and Copayment or Coinsurance waiver for contraceptives The Calendar Year Deductible and the per prescription Copayment or Coinsurance will not apply to female contraceptive methods when obtained at a network pharmacy. This means that such contraceptive methods will be paid at 100% for: The following female oral and injectable contraceptives that are Generic Prescription Drugs: - Oral drugs - Injectable drugs - Vaginal rings - Transdermal contraceptive patches Female contraceptive devices that are generic devices and brand-name devices FDA approved female: - Generic emergency contraceptives - Generic over-the-counter (OTC) emergency contraceptives The Calendar Year Deductible and the per prescription Copayment or Coinsurance continue to apply to Prescription Drugs that have a generic equivalent, biosimilar or generic alternative available within the same therapeutic drug class obtained at a network pharmacy unless you are granted a medical exception. Deductible and Copayment or Coinsurance waiver for tobacco cessation Prescription and over-the-counter drugs The Calendar Year Deductible and the per prescription Copayment or Coinsurance will not apply to the first two 90-day treatment regimens for tobacco cessation Prescription Drugs and OTC drugs when obtained at a retail network pharmacy.this means that such Prescription Drugs and OTC drugs will be paid at 100%. Your Calendar Year Deductible and any prescription Copayment or Coinsurance will apply after those two regimens have been exhausted. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [27] AZ SG-off HNO AZ Silver HNOption R
139 Eligible Health Services In-network coverage Per prescription Copayment or Coinsurance Tier 1 -- Preferred Generic Prescription Drugs For each 30 day supply filled at a retail pharmacy $15 per supply no Deductible applies For all fills greater than a 30 day supply but no more than a 90 day supply filled at a mail order pharmacy $30 per supply no Deductible applies Tier 2 -- Preferred Brand-Name Prescription Drugs For each fill up to a 30 day supply filled at a retail pharmacy $50 per supply no Deductible applies For all fills greater than a 30 day supply but no more than a 90 day supply filled at a mail order pharmacy $100 per supply no Deductible applies Tier 3 -- Non-Preferred Generic and Brand-Name Prescription Drugs For each 30 day supply filled at a retail pharmacy $80 per supply no Deductible applies For all fills greater than a 30 day supply but no more than a 90 day supply filled at a mail order pharmacy $160 per supply no Deductible applies Tier 4 -- Preferred Specialty Care Prescription Drugs(Including Biosimilar Prescription Drugs) For each 30 day supply filled at a retail pharmacy or specialty network pharmacy 30% (of the Contracted Rate) up to $300 per supply no Deductible applies Tier 5 Non-Preferred Specialty Care Prescription Drugs(Including Biosimilar Prescription Drugs) For each 30 day supply filled at a retail pharmacy or specialty network pharmacy Diabetic Prescription Drugs, Supplies and Insulin For each 30 day supply filled at a retail pharmacy For all fills greater than a 30 day supply but no more than a 90 day supply filled at a mail order pharmacy Orally Administered Anti-Cancer Medications For each 30 day supply filled at a retail pharmacy or specialty network pharmacy 50% (of the Contracted Rate) up to $500 per supply no Deductible applies Paid according to the tier of drug per the Schedule of Benefits, above Paid according to the tier of drug per the Schedule of Benefits, above Paid according to the tier of drug per the Schedule of Benefits, above however the cost-share will not exceed the cost-share provided under the medical plan for injectable and intravenous medication. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [28] AZ SG-off HNO AZ Silver HNOption R
140 Outpatient Prescription Contraceptive Drugs and Devices Female contraceptives that are Generic Prescription Drugs. For each 30 day supply: Oral drugs 0% per prescription or refill Injectable drugs Vaginal rings Transdermal contraceptive patches Female contraceptives that are brand-name Prescription Drugs. For each 30 day supply: Oral drugs Paid according to the tier of drug per the Schedule of Benefits, above Injectable drugs Vaginal rings* *Brand-name vaginal rings covered at 100% to the extent that a generic is not available Transdermal contraceptive patches Female contraceptive generic devices and brand name devices. For each 30 day supply FDA-approved female generic and brand-name emergency contraceptives. For each 30 day supply FDA-approved female generic and brand-name over-the-counter emergency contraceptives. For each 30 day supply Preventive Care Drugs and Supplements For each 30 day supply filled at a retail pharmacy 0% per prescription or refill 0% per prescription or refill 0% per prescription or refill 0% per prescription or refill Maximums: Coverage will be subject to any sex, age, medical condition, family history, and frequency guidelines in the recommendations of the United States Preventive Services Task Force. For details on the guidelines and the current list of covered preventive care drugs and supplements, contact Member Services by logging onto the Aetna Navigator secure member website at or calling the number on the back of the Member ID card. Risk Reducing Breast Cancer Prescription Drugs For each 30 day supply filled at a retail pharmacy 0% per prescription or refill Maximums: Coverage will be subject to any sex, age, medical condition, family history, and frequency guidelines in the recommendations of the United States Preventive Services Task Force. For details on the guidelines and the current list of covered risk reducing breast cancer prescription drugs, contact Member Services by logging onto the Aetna Navigator secure member website at or calling the number on the back of the Member ID card. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [29] AZ SG-off HNO AZ Silver HNOption R
141 Important note: See the Outpatient prescription contraceptive drugs and devices, Preventive care drugs and supplements and Risk reducing breast cancer prescription drugs section for more information on other Prescription Drug coverage under this plan. If the Member or the Member s prescriber requests a covered Brand-Name Prescription Drug when a covered Generic Prescription Drug equivalent is available, the Member will be responsible for the cost difference between the Generic Prescription Drug and the Brand-Name Prescription Drug, plus the cost sharing that applies to Brand-Name Prescription Drugs. The cost difference between the Generic Prescription Drug and the Brand-Name Prescription Drug charge is not applied toward the Calendar Year Deductible or Maximum Out-of-Pocket Limit. *See How to read the Schedule of Benefits at the beginning of this Schedule of Benefits HI SG-OFF2016-HNO-SB [30] AZ SG-off HNO AZ Silver HNOption R
142 IMPORTANT HEALTH CARE REFORM NOTICES CHOICE OF PROVIDER If your Aetna plan generally requires or allows the designation of a primary care provider, you have the right to designate any primary care provider who participates in our network and who is available to accept you or your family members. If the plan or health insurance coverage designates a primary care provider automatically, then until you make this designation, Aetna designates one for you. For information on how to select a primary care provider, and for a list of the participating primary care providers, contact your Employer or, if you are a current member, your Aetna contact number on the back of your ID card. If your Aetna plan allows for the designation of a primary care provider for a child, you may designate a pediatrician as the primary care provider. If your Aetna plan provides coverage for obstetric or gynecological care and requires the designation of a primary care provider then you do not need prior authorization from Aetna or from any other person (including a primary care provider) in order to obtain access to obstetrical or gynecological care from a health care professional in our network who specializes in obstetrics or gynecology. The health care professional, however, may be required to comply with certain procedures, including obtaining prior authorization for certain services, following a preapproved treatment plan, or procedures for making referrals. For a list of participating health care professionals who specialize in obstetrics or gynecology, contact your Employer or, if you are a current member, your Aetna contact number on the back of your ID card. PPACA-1 (10/10)
143 AETNA HEALTH INSURANCE COMPANY (Arizona) GROUP INSURANCE CERTIFICATE NON-REFERRED BENEFITS UNDER THE Health Network Option Open Access PROGRAM This Group Insurance Certificate ("Certificate") is part of the Group Policy ("Group Policy") between Aetna Health Insurance Company, hereinafter referred to as Aetna, and the Contract Holder. The Group Policy determines the terms and conditions of coverage. The Certificate describes covered health care benefits. Provisions of this Certificate include the Schedule of Benefits, and any amendments, endorsements, inserts, or attachments. Amendments, endorsements, inserts, or attachments may be delivered with the Certificate or added thereafter. The Certificate is part of a dual contract, to be used in conjunction with the Aetna Certificate of Coverage, which is made up of the Aetna Certificate of Coverage, Schedule of Benefits, any riders, and any amendments, endorsements, inserts, or attachments. Together, the Group Policy and the Aetna Group Agreement is referred to as the Health Network Option Open Access Program. This program provides coverage for Covered Benefits received from Participating Providers and Non- Participating Providers. This Certificate details Covered Benefits accessed through Non- Participating Providers, and the Aetna Certificate of Coverage details Referred Benefits accessed through Participating Providers. Members must be covered by the Aetna Certificate of Coverage to be eligible for benefits under this Certificate. Coverage is not provided for any services received before coverage starts or after coverage ends, except as shown in the Continuation section of this Certificate. Certain words have specific meanings when used in this Certificate. The defined terms appear in bold type with initial capital letters. The definitions of those terms are found in the Definitions section of this Certificate. This Certificate is not in lieu of insurance for Workers Compensation. This Certificate is governed by applicable federal law and the laws of Arizona. Coverage under this plan is non-occupational. Only non-occupational injuries and non-occupational illnesses are covered under this plan. If you are an owner of the company that applied for coverage under this plan and no other sources of coverage or reimbursement are available to you for the services or supplies, then you will also be covered for occupational injuries and occupational illnesses. Other sources of coverage or reimbursement may include workers compensation, or an occupational illness or similar program under local, state or federal law. A source of coverage or reimbursement will be considered available to you even if you waived your right to payment from that source. If you are also covered under a workers compensation law or similar law, and submit proof that you are not covered for a particular illness or injury under such law, that illness or injury will be considered non-occupational regardless of cause. HO SG2016COC 03 1 SG Off Exchange
144 READ THIS ENTIRE CERTIFICATE CAREFULLY. IT DESCRIBES THE RIGHTS AND OBLIGATIONS OF MEMBERS AND AETNA. IT IS THE CONTRACT HOLDER S AND THE MEMBER'S RESPONSIBILITY TO UNDERSTAND THE TERMS AND CONDITIONS IN THIS CERTIFICATE. IN SOME CIRCUMSTANCES, CERTAIN MEDICAL SERVICES ARE NOT COVERED OR MAY REQUIRE PRECERTIFICATION BY AETNA. NO SERVICES ARE COVERED UNDER THIS CERTIFICATE IN THE ABSENCE OF PAYMENT OF CURRENT PREMIUMS SUBJECT TO THE GRACE PERIOD AND THE PREMIUMS SECTION OF THE GROUP POLICY. THIS CERTIFICATE APPLIES TO COVERAGE ONLY AND DOES NOT RESTRICT A MEMBER S ABILITY TO RECEIVE HEALTH CARE SERVICES THAT ARE NOT, OR MIGHT NOT BE, COVERED BENEFITS UNDER THIS CERTIFICATE. PROVIDERS, INSTITUTIONS, FACILITIES OR AGENCIES ARE NEITHER AGENTS NOR EMPLOYEES OF AETNA. Important Unless otherwise specifically provided, no Member has the right to receive the benefits of this plan for health care services or supplies furnished following termination of coverage. Benefits of this plan are available only for services or supplies furnished during the term the coverage is in effect and while the individual claiming the benefits is actually covered by the Group Policy. Benefits may be modified during the term of this plan as specifically provided under the terms of the Group Policy or upon renewal. If benefits are modified, the revised benefits (including any reduction in benefits or elimination of benefits) apply for services or supplies furnished on or after the effective date of the modification. Aetna will provide 60 day advance notice to the Member before the effective date of any material modification including changes in preventative benefits. There is no vested right to receive the benefits of the Group Policy. HO SG2016COC 03 2 SG Off Exchange
145 TABLE OF CONTENTS Section Page Aetna Procedure 4 Eligibility 7 Covered Benefits 7 Exclusions and Limitations 45 Termination of Coverage 54 Continuation 54 Claim Procedures/Complaints and Appeals 54 /Dispute Resolution Coordination of Benefits 54 Responsibility of Members 54 General Provisions 55 Definitions 59 HO SG2016COC 03 3 SG Off Exchange
146 AETNA PROCEDURE You Must Have Coverage with Aetna A Member must be covered by Aetna for the health benefits listed in the Aetna Certificate of Coverage in order to be eligible to be covered by this Certificate. If a Member is not covered under the Aetna Certificate of Coverage or fails to remain covered under the Aetna Certificate of Coverage, the Member cannot remain covered under this Certificate. Legal Relationship This Certificate establishes a legal relationship between the Member and Aetna. The Member is entitled to receive from Aetna only the benefits specified in this Certificate. Benefits Available Through the Health Network Option Open Access Program This Certificate provides coverage in the event the Member seeks benefits from Non-Participating Providers. Aetna must be contacted for Precertification prior to receiving certain services or supplies that are identified in this Certificate as requiring Precertification in order to avoid a reduction in benefits. The Aetna Certificate of Coverage The Member s eligibility to receive Aetna Benefits under the Aetna Certificate of Coverage makes the Member eligible to receive coverage under this Certificate for Covered Benefits. A copy of the Aetna Certificate of Coverage, to which this Certificate is attached, is made part of this Certificate. In case of any discrepancy in meaning, this Certificate shall control Covered Benefits under the Health Network Option Open Access Program. Aetna and Health Network Option Open Access Benefits received under the Aetna Certificate of Coverage, and benefits that a Member receives under this Certificate, do not duplicate each other. A service or supply, which is a covered benefit under the Aetna Certificate of Coverage, is not a Covered Benefit under this Certificate. Any Aetna Benefits that a Member receives under the Aetna Certificate of Coverage, and any benefits that a Member receives under this Certificate, will be combined when calculating the maximum benefits which a Member is entitled to receive under either Certificate. Benefit limits offset and do not duplicate each other. The benefits provided under this Certificate are offered only in conjunction with and as a supplement to Aetna Benefits. Any Aetna Benefits covered by rider(s), amendment(s) and/or endorsement(s) to the Aetna Certificate of Coverage are not part of this Certificate and are excluded from coverage hereunder, unless such services are specifically included in the Covered Benefits section of this Certificate. Copayments paid by Members for Aetna Benefits received under the Aetna Certificate of Coverage, including any rider(s), amendment(s) and/or endorsement(s), shall not apply in satisfying the Deductibles under this Certificate. HO SG2016COC 03 4 SG Off Exchange
147 Ongoing Reviews Aetna conducts ongoing reviews of those services and supplies which are recommended or provided by Health Professionals to determine whether such services and supplies are Covered Benefits under this Certificate. If Aetna determines that the recommended services and supplies are not Covered Benefits, the Member will be notified. If a Member wishes to appeal such determination, the Member may then contact Aetna to seek a review of the determination. Please refer to the Claim Procedures/Complaints and Appeals/Dispute Resolution section of the Aetna Certificate. Precertification Certain services, such as inpatient stays, require Precertification by Aetna. Precertification is a process that helps you and your Physician determine whether the services being recommended are Covered Benefits under the plan. It also allows Aetna to help your Provider coordinate your transition from an inpatient setting to an outpatient setting (called discharge planning), and to register you for specialized programs or case management when appropriate. When you go to a Non-Participating Provider, it is your responsibility to obtain Precertification from Aetna for any services or supplies on the Precertification list below. If you do not Precertify, your benefits the plan may not pay any benefits. The list of services requiring Precertification appears below. Precertification for Emergency services is not required, however, we do suggest that you, or your Physician or facility call as soon as reasonable possible. If your outpatient Hospice Care has been Precertified, and you subsequently require a Hospital stay for pain control or acute symptom management, that Hospital stay does not have to be Precertified. Important Note Please read the following sections in their entirety for important information on the precertification process, and any impact it may have on your coverage. Services and Supplies Which Require Precertification Precertification is required for the following types of medical expenses: Inpatient and Outpatient Care Stays in a hospital; Stays in a skilled nursing facility; Stays in a rehabilitation facility; Stays in a hospice facility; Stays in a residential treatment facility for treatment of mental disorders and substance abuse; Complex imaging; Cosmetic and reconstructive surgery; Injectables, (immunoglobulins, growth hormones, Multiple Sclerosis medications, Osteoporosis medications, Botox, Hepatitis C medications); Kidney dialysis; Bariatric surgery (obesity); Outpatient back surgery not performed in a physician s office; Sleep studies; Knee surgery; and Wrist surgery. HO SG2016COC 03 5 SG Off Exchange
148 The Out-of Network Precertification Process Precertification should be secured within the timeframes specified below. To obtain precertification, call Aetna at the telephone number listed on the back of your ID card. This call must be made: For non-emergency admissions: For an emergency admission: For an urgent admission: For outpatient non-emergency medical services requiring Precertification: You or a member of your family, your Physician or the facility will need to call and request Precertification at least 14 days before the date you are scheduled to be admitted. You or a member of your family, your Physician or the facility should call within 48 hours or as soon as reasonably possible after you have been admitted. You or a member of your family, your Physician or the facility will need to call before you are scheduled to be admitted. You or a member of your family, your Physician or the facility must call at least 14 days before the outpatient care is provided, or the treatment or procedure is scheduled. Aetna will provide a written notification to you and your Physician of the Precertification decision where required under applicable State law. If your Precertified expenses are approved the approval is good for 180 days as long as you remain enrolled in the plan. Precertification, Precertify, Precertified A process where Aetna is contacted before certain services are provided, such as hospitalization or outpatient services, are prescribed to determine whether the services being recommended or the drugs prescribed are considered covered expenses under the plan. It is not a guarantee that benefits will be payable if, for example, it is determined at the time the claim is submitted that you were not eligible for benefits at that time. Precertification Penalty Aetna will reduce the benefits payable under this Certificate by the percentage or dollar amount set forth on the Schedule of Benefits if the procedures for Precertification set forth in this Certificate are not followed. The Member will be responsible to pay the unpaid balance of the benefits. FAILURE TO PRECERTIFY WILL RESULT IN A REDUCTION OF BENEFITS UNDER THIS CERTIFICATE. PLEASE REFER TO THE SCHEDULE OF BENEFITS FOR THE PRECERTIFICATION PENALTY. The additional percentage or dollar amount of the Recognized Charge which a Member may pay as a penalty for failure to obtain Precertification under this section is not a Covered Expense, and will not be applied to the Deductible amount or the Maximum Out-of-Pocket Limit, if any. HO SG2016COC 03 6 SG Off Exchange
149 ELIGIBILITY In order to be eligible to receive benefits and to be covered under this Certificate, a Member first must be eligible to receive benefits as a Subscriber or as a dependent of a Subscriber under the Aetna Certificate of Coverage, and be covered under it. The Effective Date of Coverage under this Certificate shall be the same date as the Effective Date of Coverage under the Aetna Certificate. COVERED BENEFITS A Member shall be entitled to the Covered Benefits as specified below, in accordance with the terms and conditions of this Certificate. Unless specifically stated otherwise, in order for benefits to be covered, they must be Medically Necessary. For the purpose of coverage, Aetna may determine whether any benefit provided under the Certificate is Medically Necessary. Preventive Care and Wellness Benefits, as described below, will be considered Medically Necessary. Important Note: You should review your Schedule of Benefits for the cost sharing that applies to the Covered Benefits in this section. This will help you become familiar with your payment responsibilities. Some Covered Benefits may have visit limits and maximums that apply to the service or supply. You should always review your Certificate and Schedule of Benefits together. ALL SERVICES ARE SUBJECT TO THE EXCLUSIONS AND LIMITATIONS DESCRIBED IN THIS CERTIFICATE. To be Medically Necessary, the service or supply must: Be care or treatment as likely to produce a significant positive outcome as, and no more likely to produce a negative outcome than, any alternative service or supply, both as to the disease or injury involved and the Member's overall health condition; Be care or services related to diagnosis or treatment of an existing illness or injury, except for Preventive Care Benefits, as determined by Aetna; Be a diagnostic procedure, indicated by the health status of the Member and be as likely to result in information that could affect the course of treatment as, and no more likely to produce a negative outcome than, any alternative service or supply, both as to the disease or injury involved and the Member's overall health condition; Include only those services and supplies that cannot be safely and satisfactorily provided at home, in a Physician s or Dental Provider s office, on an outpatient basis, or in any facility other than a Hospital, when used in relation to inpatient Hospital services; and As to diagnosis, care and treatment be no more costly (taking into account all health expenses incurred in connection with the service or supply) than any equally effective service or supply in meeting the above tests. HO SG2016COC 03 7 SG Off Exchange
150 In determining if a service or supply is Medically Necessary, Aetna s Patient Management Medical Director or its Physician or Dentist designee will consider: Information provided on the Member's health status; Reports in peer reviewed medical literature; Reports and guidelines published by nationally recognized health care organizations that include supporting scientific data; Professional standards of safety and effectiveness which are generally recognized in the United States for diagnosis, care or treatment; The opinion of Health Professionals in the generally recognized health specialty involved; The opinion of the attending Physicians or Dental Providers, which have credence but do not overrule contrary opinions; and Any other relevant information brought to Aetna's attention. All Covered Benefits will be covered in accordance with the guidelines determined by Aetna. If a Member has questions regarding coverage under this Certificate, the Member may call the Member Services toll-free telephone number listed on the Member s identification card. THE MEMBER IS RESPONSIBLE FOR PAYMENT OF THE APPLICABLE COPAYMENTS AND DEDUCTIBLES LISTED ON THE SCHEDULE OF BENEFITS. IMPORTANT: REFER TO THE AETNA PROCEDURE SECTION OF THIS CERTIFICATE FOR THE LIST OF SERVICES AND SUPPLIES WHICH REQUIRE PRECERTIFICATION. 1. Preventive Care and Wellness Benefits Preventive Care 1. The recommendations and guidelines of the: Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention; United States Preventive Services Task Force; and Health Resources and Services Administration; as referenced throughout this Preventive Care Benefit may be updated periodically. This Plan is subject to updated recommendations or guidelines that are issued by these organizations beginning on the first day of the plan year, one year after the recommendation or guideline is issued. 2. If any diagnostic x-rays, lab, or other tests or procedures are ordered, or given, in connection with any of the Preventive Care Benefits described below, those diagnostic x-rays, lab or other tests or procedures will not be covered as Preventive Care Benefits. Those that are Covered Benefits will be subject to the cost-sharing that applies to those specific services under this Plan. 3. Refer to the Schedule of Benefits for information about cost-sharing and maximums that apply to Preventive Care benefits. HO SG2016COC 03 8 SG Off Exchange
151 4. Gender-Specific Preventive Care Benefits -- covered expenses include any recommended Preventive Care benefits described below that are determined by your provider to be medically necessary, regardless of the sex you were assigned at birth, your gender identity, or your recorded gender. 5. To learn what frequency and age limits apply to routine physical exams and routine cancer screenings, contact your physician or contact Member Services by logging on to your Aetna Navigator secure member website at www. aetna.com or at the toll-free number on your ID card. This information can also be found at the website. Routine Physical Exam Benefit Covered Benefits include office visits to a Member's Primary Care Physician for routine physical exams, including routine vision and hearing screenings given as part of the routine physical exam. A routine exam is a medical exam given by a Physician for a reason other than to diagnose or treat a suspected or identified illness or injury, and also includes: Evidence-based items that have in effect a rating of A or B in the current recommendations of the United States Preventive Services Task Force; Services as recommended in the American Academy of Pediatrics/Bright Futures/Health Resources and Services Administration guidelines for children and adolescents. For females, screenings and counseling services as provided for in the comprehensive guidelines recommended by the Health Resources and Services Administration. These services may include but are not limited to: - Screening and counseling services, such as those on: - Interpersonal and domestic violence; - Sexually transmitted diseases; and - Human Immune Deficiency Virus (HIV) infections. - Screening for gestational diabetes. - High risk Human Papillomavirus (HPV) DNA testing for women age 30 and older. X-rays, lab and other tests given in connection with the exam. For covered newborns, an initial Hospital check-up. Benefits for the routine physical exam services above may be subject to visit maximums as shown in the Schedule of Benefits. For details on the frequency and age limits that apply to Routine Physical Exam Benefit, Members may contact their Physician or Member Services by logging onto the Aetna Navigator website or calling the toll-free number on the back of the ID card. For a detailed listing of preventive care services described in this section refer to Benefit Limitations: Unless specified above, not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; Services which are for diagnosis or treatment of a suspected or identified illness or injury; Exams given while the Member is confined in a Hospital or other facility for medical care; Services not given by a Physician or under his or her direction; and HO SG2016COC 03 9 SG Off Exchange
152 Psychiatric, psychological, personality or emotional testing or exams. Preventive Care Immunizations Benefit Covered Benefits include: Immunizations for infectious diseases; and The materials for administration of immunizations; provided by a Member's Physician or a facility. The immunizations must be recommended by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention. Specifically, the following immunizations are covered for adults at the recommended ages and populations: Hepatitis A, Hepatitis B, Herpes Zoster, Human Papillomavirus, Influenza (flu shot), Measles, Mumps, Rubella, Meningococcal, Pneumococcal, Tetanus, Diphtheria, Pertussis, and Varicella. Specifically, the following immunizations are covered for children, from birth to age 18, at the recommended ages and populations: Diphtheria, Tetanus, Pertussis, Haemophilus Influenza type b, Hepatitis A, Hepatitis B, Human Papillomavirus, Inactivated Poliovirus, Influenza (flu shot), Measles, Mumps, Rubella, Meningococcal, Pneumococcal, Rotavirus, and Varicella. Benefit Limitations: Not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; and Immunizations that are not considered preventive care such as those required due to a Member's employment or travel. Well Woman Preventive Visits Benefit Covered Benefits include a routine well woman preventive exam office visit, including Pap smears, provided by a Member's PCP, Physician, obstetrician, or gynecologist in accordance with the recommendations by the Health Resources and Services Administration. A routine well woman preventive exam is a medical exam given by a Physician for a reason other than to diagnose or treat a suspected or identified illness or injury; and Routine preventive care breast cancer genetic counseling and breast cancer (BRCA) gene blood testing. Covered Benefits include charges made by a Physician and lab for the BRCA gene blood test and charges made by a genetic counselor to interpret the test results and evaluate treatment. These benefits will be subject to any age; family history; and frequency guidelines that are: Evidence-based items or services that have in effect a rating of A or B in the recommendations of the United States Preventive Services Task Force; and Evidence-informed items or services provided in the comprehensive guidelines supported by the Health Resources and Services Administration. Benefits for the well woman preventive visit services above are subject to visit maximums as shown in the Schedule of Benefits. HO SG2016COC SG Off Exchange
153 Benefit Limitations: Unless specified above, not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; Services which are for diagnosis or treatment of a suspected or identified illness or injury; Exams given while the Member is confined in a Hospital or other facility for medical care; Services not given by a Physician or under his or her direction; and Psychiatric, psychological, personality or emotional testing or exams; and Services and supplies furnished by a Non-Participating Provider. Screening and Counseling Services Benefit Covered Benefits include the following services provided by a Member's Physician, as applicable, in an individual or group setting: Obesity and/or Healthy Diet Counseling Benefit Covered Benefits include screening and counseling services to aid in weight reduction due to obesity. Coverage includes: Preventive counseling visits and/or risk factor reduction intervention; Nutritional counseling; and Healthy diet counseling visits provided in connection with Hyperlipidemia (high cholesterol) and other known risk factors for cardiovascular and diet-related chronic disease. Benefits for the screening and counseling services above are subject to the visit maximums as shown in the Schedule of Benefits. Sexually Transmitted Infection Counseling Covered Benefits include the counseling services to help you prevent or reduce sexually transmitted infections. Genetic Risk Counseling for Breast and Ovarian Cancer Covered Benefits include the counseling and evaluation services to help you assess whether or not you are at risk of breast and ovarian cancer. Misuse of Alcohol and/or Drugs Benefit Covered Benefits include screening and counseling services to aid in the prevention or reduction of the use of an alcohol agent or controlled substance. Coverage includes preventive counseling visits, risk factor reduction intervention and a structured assessment. Benefits for the screening and counseling services above are subject to visit maximums as shown later in this amendment. Use of Tobacco Products Benefit Covered Benefits include screening and counseling services to aid in the cessation of the use of tobacco products. HO SG2016COC SG Off Exchange
154 Coverage includes: Preventive counseling visits; Treatment visits; and Class visits; to aid in the cessation of the use of tobacco products. Coverage also includes the use of over-the-counter (OTC) smoking cessation medications and prescription U.S. Food and Drug Administration (FDA) approved smoking cessation medications when used in accordance with FDA approval including nicotine replacement therapy. Tobacco product means a substance containing tobacco or nicotine including: Cigarettes; Cigars; Smoking tobacco; Snuff; Smokeless tobacco; Candy-like products that contain tobacco; and Nicotine replacement therapy includes but is not limited to nicotine gum, patches, lozenges, nasal spray, and inhalers. Benefits for the screening and counseling services above are subject to visit maximums as shown in the Schedule of Benefits. Benefit Limitations: Unless specified above, not covered under this benefit are services which are covered to any extent under any other part of this Certificate. Tobacco Cessation Prescription and Over-the-Counter Drugs Covered Benefits include FDA-approved Prescription Drugs and over-the-counter (OTC) drugs to help stop the use of tobacco products, when prescribed by a Prescriber and the Prescription is submitted to the pharmacist for processing. Routine Cancer Screenings Benefit Covered Benefits include, but are not limited to, the following routine cancer screenings: One baseline mammogram for a woman age 35 to 39; One annual mammogram for a woman age 40 and over; Fecal occult blood tests; Digital rectal exams; Prostate specific antigen (PSA) tests; Sigmoidoscopies; Double contrast barium enema (DCBE); and Colonoscopies; (removal of polyps performed during a screening procedure is a Covered Benefit); and Lung cancer screenings. HO SG2016COC SG Off Exchange
155 These benefits will be subject to any age, family history and frequency guidelines that are: Evidence-based items or services that have in effect a rating of A or B in the recommendations of the United States Preventive Services Task Force; and Evidence-informed items or services provided in the comprehensive guidelines supported by the Health Resources and Services Administration. For details on the frequency and age limits that apply to Routine Cancer Screenings Benefit, Members may contact their Physician or Member Services by logging onto the Aetna Navigator website or calling the toll-free number on the back of the ID card. Benefit Limitations: Unless specified above, not covered under this benefit are services which are covered to any extent under any other part of this Plan. Prenatal Care Benefit Prenatal care will be covered as Preventive Care for services received by a pregnant female in a Physician's, OB/GYN, obstetrician's, or gynecologist's office but only to the extent described below. Coverage for prenatal care under this benefit is limited to pregnancy-related Physician office visits including the initial and subsequent history and physical exams of the pregnant woman (maternal weight, blood pressure; fetal heart rate check and fundal height). Benefit Limitations: Unless specified above, not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; and Services for maternity care (other than prenatal care as described above). Important Note: Refer to the: Maternity Care and Related Newborn Care Benefits section of the Certificate; and Prenatal Care Services, Delivery Services and Postpartum Care Services cost-sharing in the Schedule of Benefits; for more information on coverage for services related to maternity care under this Plan. Comprehensive Lactation Support and Counseling Services Benefit Covered Benefits include comprehensive lactation support (assistance and training in breast feeding) and counseling services provided to females during pregnancy or at any time following delivery, for breastfeeding by a certified lactation support provider. Covered Benefits also include the rental or purchase of breast feeding equipment as described below. Lactation support and lactation counseling services are Covered Benefits when provided in either a group or individual setting. Benefits for lactation counseling services are subject to the visit maximum shown later in this amendment. HO SG2016COC SG Off Exchange
156 Breast Feeding Durable Medical Equipment Covered Benefits includes the rental or purchase of breast feeding Durable Medical Equipment for the purpose of lactation support (pumping and storage of breast milk) as follows. Breast Pumps Covered Benefits include the following: The rental of a hospital-grade electric pump for a newborn child when the newborn child is confined in a Hospital. The purchase of: - An electric breast pump (non-hospital grade),. A purchase will be covered once every three years; or - A manual breast pump. A purchase will be covered once per pregnancy. If a breast pump was purchased within the previous three year period, the purchase of another breast pump will not be covered until a three year period has elapsed from the last purchase. Breast Pump Supplies Coverage is limited to only one purchase per pregnancy in any year where a covered female would not qualify for the purchase of a new pump. Coverage for the purchase of breast pump equipment is limited to one item of equipment, for the same or similar purpose, and the accessories and supplies needed to operate the item. A Member is responsible for the entire cost of any additional pieces of the same or similar equipment purchased or rented for personal convenience or mobility. Aetna reserves the right to limit Covered Benefits to the most cost efficient and least restrictive level of service or item which can be safely and effectively provided. The decision to rent or purchase is at the discretion of Aetna. Benefit Limitations: Unless specified above, not covered under this benefit are services which are covered to any extent under any other part of this Plan. Family Planning Services - Female Contraceptives Benefit Important Note: For a list of the types of female contraceptives covered under this plan, refer to the section What the Pharmacy Benefit Covers and the Contraceptives benefit later in this Booklet-Certificate. For females with reproductive capacity, Covered Benefits include those services and supplies that are provided to a Member to prevent pregnancy. All contraceptive methods, services and supplies covered under this benefit must be approved by the U.S. Food and Drug Administration (FDA). HO SG2016COC SG Off Exchange
157 Voluntary Sterilization Covered Benefits include charges billed separately by the provider for female voluntary sterilization procedures and related services and supplies including, but not limited to, tubal ligation and sterilization implants. Covered Benefits under this benefit would not include a voluntary sterilization procedure to the extent that the procedure was not billed separately by the provider or because it was not the primary purpose of the confinement. Benefit Limitations: Unless specified above, not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; Services and supplies incurred for an abortion; Services which are for the treatment of an identified illness or injury; Services that are not given by a Physician or under his or her direction; Psychiatric, psychological, personality or emotional testing or exams; Any contraceptive methods that are only "reviewed" by the FDA and not "approved" by the FDA; The reversal of voluntary sterilization procedures, including any related follow-up care. 2. Physician and Other Health Professional Care Physician Benefit Office visits during office hours. Home visits. Hospital visits. If the Member's injury or illness is a Medical Emergency, the Member should follow the procedures outlined under the Emergency Care/Urgent Care Benefits section of this Certificate Immunizations for infectious disease, but not if solely for your employment or travel. Allergy testing and allergy injections. Charges made by the Physician for supplies, radiological services, x-rays, and tests provided by the Physician. Alternatives to Physicians Office Visits Walk-in Clinic Benefits Covered Benefits include charges made by walk-in clinics for: Unscheduled, non-emergency illnesses and injuries; The administration of certain immunizations administered within the scope of the clinic s license; and Individual screening and counseling services to aid you: - In weight reduction due to obesity; - In developing and maintaining a healthy diet; - To stop the use of tobacco products. HO SG2016COC SG Off Exchange
158 Benefit Limitations: Unless specified above, not covered under this benefit are charges incurred for services and supplies furnished in a group setting for screening and counseling services Important Note: Not all services are available at all Walk-In Clinics. The types of services offered will vary by the provider and location of the clinic. For a complete description of the screening and counseling services provided on the use of tobacco products, healthy diet and to aid in weight reduction due to obesity, refer to the Preventive Care Benefits section in this Certificate and the Screening and Counseling Services benefit for a description of these services. These services may also be obtained from your Physician. Specialist Physician Benefits Covered Benefits include outpatient and inpatient services. Coverage is also provided for second medical opinions regarding a proposed surgery or course of treatment recommended by a Physician. Important: Refer to the Aetna Procedure section of this Certificate for the list of services and supplies which require Precertification. Covered Benefits also include Telemedicine consultations An online, internet, consultation between a Member and a Physician about a health care matter that is not a Medical Emergency or Urgent Care. A Telemedicine consultation shall not substitute a Member s initial in-person consultation with a Physician, and it must be conducted through an Aetna authorized internet Telemedicine service vendor. Important Reminder: For a description of the preventive care benefits covered under this Certificate, refer to the Preventive Care and Wellness Benefits section in this Certificate. 3. Hospital and Other Facility Care Hospital Benefit A Member is covered for inpatient Hospital services and supplies. Private accommodations will be provided when Medically Necessary as determined by Aetna, upon certification by the Physician or Aetna. Without such certification, only semi-private room and board accommodations will be considered a Covered Benefit. Skilled Nursing Facility Benefit A Member is covered for Skilled Care in a Skilled Nursing Facilities. Coverage for Skilled Nursing Facility benefits is subject to the limits, if any, shown on the Schedule of Benefits. Outpatient Surgery Benefit Coverage is provided for outpatient surgical services and supplies in connection with a covered surgical procedure when furnished by an outpatient surgery center. HO SG2016COC SG Off Exchange
159 Home Health Care Benefit The following services are covered for a Homebound Member when provided by a home health care agency. Precertification must be obtained from the Aetna by the Member s attending Physician. Aetna shall not be required to provide home health benefits when Aetna determines the treatment setting is not appropriate, or when there is a more cost effective setting in which to provide covered health care services. Coverage for Home Health Services is not determined by the availability of caregivers to perform the services; the absence of a person to perform a non-skilled or Custodial Care service does not cause the service to become covered. If the Member is a minor or an adult who is dependent upon others for non-skilled care (e.g. bathing, eating, toileting), coverage for Home Health Services will only be provided during times when there is a family member or caregiver present in the home to meet the Member s non-skilled needs. Skilled Nursing services that require the medical training of and are provided by a licensed nursing professional are a covered benefit. Services must be provided during intermittent visits of 4 hours or less with a daily maximum of 3 visits. Up to 12 hours (3 visits) of continuous Skilled Nursing services per day within 30 days of an inpatient Hospital or Skilled Nursing Facility discharge may be covered, when all home health care criteria are met, for transition from the Hospital or Skilled Nursing Facility to home care. Services of a home health aide are covered only when they are provided in conjunction with Skilled Nursing services and directly support the Skilled Nursing. Services must be provided during intermittent visits of 4 hours or less with a daily maximum of 3 visits. Medical social services are covered only when they are provided in conjunction with Skilled Nursing services and must be provided by a qualified social worker. Skilled behavioral health care services provided in the home by a behavioral health provider when ordered by a physician and directly related to an active treatment plan of care established by the physician. All of the following must be met: - The skilled behavioral health care is appropriate for the active treatment of a condition, illness or disease to avoid placing you at risk for serious complications. - The services are in lieu of a continued confinement in a hospital or residential treatment facility, or receiving outpatient services outside of the home. - You are homebound because of illness or injury. - The services provided are not primarily for comfort, convenience or custodial in nature. - The services are intermittent or hourly in nature. Outpatient home health short-term physical, speech, or occupational therapy is covered when the above home health care criteria are met. Coverage is subject to the conditions and limits listed in the Short- Term Rehabilitation Therapy Services Benefit section of the Certificate and the Short-Term Rehabilitation and Habilitation Therapy Services Benefit section of the Schedule of Benefits. Covered Home Health Care benefits do not include charges for infusion therapy or applied behavior analysis. HO SG2016COC SG Off Exchange
160 Hospice Benefit Hospice Care services for a terminally ill Member are covered. Services may include home and Hospital visits by nurses and social workers; pain management and symptom control; instruction and supervision of a family Member; inpatient care; counseling and emotional support; and other home health benefits listed in the Home Health Benefits section of this Certificate. Benefit Limitations: Coverage is not provided for funeral arrangements, pastoral counseling, and financial or legal counseling. Homemaker or caretaker services, and any service not solely related to the care of the Member, including but not limited to, sitter or companion services for the Member or other Members of the family, transportation, house cleaning, and maintenance of the house are not covered. 4. Emergency Care and Urgent Care Emergency Care/Urgent Care Benefit 1. A Member is covered for Emergency Services and Urgent Care benefits without Precertification, provided the services are Covered Benefits, and Aetna's review determines that a Medical Emergency or Urgent Care situation existed at the time medical attention was sought by the Member. Medical transportation is covered during a Medical Emergency. 2. A Member is covered for any follow-up care. Follow-up care is any care directly related to the need for Emergency Services or Urgent Care which is provided to a Member after the Medical Emergency care or Urgent Care situation has terminated. 5. Specific Conditions Maternity Care and Related Newborn Care Benefit Outpatient and inpatient pre-natal and postpartum care and obstetrical services are a Covered Benefit. Coverage for maternity care and related newborn care benefits is provided to the extent covered by this Certificate for Specialist Physician benefits and inpatient Hospital benefits, and is subject to the limits, if any, shown on the Schedule of Benefits. As an exception to the Medically Necessary requirements of this Certificate, the following coverage is provided for a mother and newly born child: A minimum of 48 hours of inpatient care in a Hospital following a vaginal delivery; A minimum of 96 hours of inpatient care in a Hospital following a cesarean section; or A shorter Hospital stay, if requested by a mother, and if determined to be medically appropriate by the Providers in consultation with the mother. If a Member requests a shorter Hospital stay, the Member will be covered for one home health care visit scheduled to occur within 24 hours of discharge. An additional visit will be covered when prescribed by HO SG2016COC SG Off Exchange
161 the Provider. This benefit is in addition to the home health maximum number of visits, if any, shown on the Schedule of Benefits. A Copayment or Coinsurance will not apply for home health care visits. Coverage for a legally adopted child or for a child who has been placed for adoption with the Subscriber will include expenses incurred for services and supplies related to the cost of such child's birth, if: 1. the child is adopted within one year of birth; and 2. the Subscriber is legally obligated to pay the costs of the child's birth; and 3. the Subscriber has notified Aetna of his or her acceptability to adopt children pursuant to Arizona law regarding adoption, within 60 days after such acceptance or within 60 days after enrolling; whichever occurs last. Aetna coverage shall be secondary to and in excess of any other maternity benefits coverage of the natural mother. The Subscriber must notify Aetna regarding the existence and extent of any other such coverage of the natural mother. Within 31 days of Aetna's request, the Subscriber shall provide evidence satisfactory to Aetna that the child meets any of the above requirements. Precertification is required soon after pregnancy is confirmed and within 24 hours after birth or as soon thereafter as possible. Reconstructive Breast Surgery Benefit Covered Benefits include reconstruction of the breast on which a mastectomy was performed, including an implant and areolar reconstruction. Also included is surgery on a healthy breast to make it symmetrical with the reconstructed breast and Medically Necessary physical therapy to treat complications of mastectomy, including lymphedema. Reconstructive or Cosmetic Surgery and Supplies Covered Benefits include charges made by a Physician, Hospital, or surgery center for reconstructive services and supplies, including: Surgery needed to improve a significant functional impairment of a body part. Surgery to correct the result of an accidental injury, including subsequent related or staged surgery, provided that the surgery occurs no more than 24 months after the original injury. For a covered child, the time period for coverage may be extended through age 18. Surgery to correct the result of an injury that occurred during a covered surgical procedure provided that the reconstructive surgery occurs no more than 24 months after the original injury. Important Note: Injuries that occur as a result of a medical (i.e., non-surgical) treatment are not considered accidental injuries, even if unplanned or unexpected. Surgery to correct a gross anatomical defect present at birth or appearing after birth (but not the result of an illness or injury) when - The defect results in severe facial disfigurement, or - The defect results in significant functional impairment and the surgery is needed to improve function. HO SG2016COC SG Off Exchange
162 Mental Disorders Benefit Covered Benefits include charges made by a Hospital, Psychiatric Hospital, Residential Treatment Facility or Behavioral Health Provider for the treatment of Mental Disorders as follows: Inpatient room and board at the semi-private room rate, and other services and supplies related to your condition that are provided during your stay in a Hospital, Psychiatric Hospital, or Residential Treatment Facility. Outpatient treatment received while not confined as an inpatient in a Hospital or Psychiatric Hospital or Residential Treatment Facility, including: as described below. Partial Hospitalization Treatment (at least 4 hours, but less than 24 hours per day of clinical treatment) provided in a facility or program under the direction of a Physician. The facility or program does not make a room and board charge for the treatment. - Intensive Outpatient Program (at least 2 hours per day and at least 6 hours per week of clinical treatment) provided in a facility or program under the direction of a Physician. Office visits to a Physician (such as a Psychiatrist), psychologist, social worker, or licensed professional counselor, as well as other health professionals. Benefits are payable in the same way as those for any other disease. Important Note: Not all types of services are covered. For example, educational services and certain types of therapies are not covered. See Exclusions section for more information. Important Reminder Inpatient and certain outpatient treatments must be precertified by Aetna. Substance Abuse Benefit Covered Benefits include charges made by a Hospital, Psychiatric Hospital, Residential Treatment Facility or Behavioral Health Provider for the treatment of Substance Abuse as follows: Inpatient room and board at the semi-private room rate and other services and supplies that are provided during your stay in a Hospital, Psychiatric Hospital or Residential Treatment Facility. Treatment of Substance Abuse in a general medical Hospital is only covered when you are admitted to the Hospital s separate Substance Abuse section (or unit), for treatment of medical complications of Substance Abuse. As used here, medical complications include, but are not limited to, Detoxification, electrolyte imbalances, malnutrition, cirrhosis of the liver, delirium tremens and hepatitis. Outpatient treatment received while not confined as an inpatient in a Hospital or Psychiatric Hospital or as part of Partial Hospitalization Treatment including: Partial Hospitalization Treatment (at least 4 hours, but less than 24 hours per day of clinical treatment) provided in a facility or program under the direction of a Physician. The facility or program does not make a room and board charge for the treatment. Partial Hospitalization Treatment will only be covered if: - Intensive Outpatient Program (at least 2 hours per day and at least six hours per week of clinical treatment) provided in a facility or program under the direction of a physician. HO SG2016COC SG Off Exchange
163 - Ambulatory detoxification Outpatient services that monitor withdrawal from alcohol or other substance abuse, including administration of medications. - Office visits to a physician (such as a psychiatrist), psychologist, social worker, or licensed professional counselor, as well as other health care professionals. Benefits are payable in the same way as those for any other disease. Important Note: Not all types of services are covered. For example, educational services and certain types of therapies are not covered. See Exclusions section for more information. Important Reminder Inpatient and certain outpatient treatments must be precertification by Aetna. Autism Spectrum Disorders Benefit Autism Spectrum Disorder is defined in the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association. Covered Benefits include the services and supplies for the screening, diagnosis and treatment, (including behavioral therapy and Applied Behavioral Analysis), of Autism Spectrum Disorder. The services and supplies must be ordered by a Physician or Behavioral Health Provider. Coverage also includes early intensive behavioral interventions such as Applied Behavioral Analysis (ABA). Applied Behavioral Analysis is an educational service that is the process of applying interventions that: Systematically change behavior; and Are responsible for the observable improvement in behavior. Coverage for Applied Behavioral Analysis is subject to the maximums shown in the Schedule of Benefits, if any. Important: Applied Behavior Analysis requires precertification by Aetna. Please refer to the Aetna Precertification section of the Certificate for information regarding precertification procedures that must be followed. Diabetes Benefit Covered Benefits include charges for the following services, supplies, equipment, and training for the treatment of insulin- and non-insulin-dependent diabetes as well as gestational diabetes: Services and Supplies: - Foot care to minimize the risk of infection; - Insulin preparations; - Diabetic needles and syringes; - Diabetic test agents; - Lancets/lancing devices; - Prescribed oral medications whose primary purpose is to influence blood sugar; - Alcohol swabs; HO SG2016COC SG Off Exchange
164 - Injectable glucagons; and - Glucagon emergency kits. Equipment: - External insulin pumps; and - Blood glucose monitors without special features unless required due to blindness. Training: - Self-management training provided by a licensed health care provider certified in diabetes self-management training. Basic Infertility Services Benefit Infertility services and supplies to diagnose the underlying medical cause of Infertility are covered. All other Infertility services and supplies are not covered. Transplant Benefit Transplant Benefit Non-experimental or non-investigational Transplants are Covered Benefits. Covered Benefits include the following:. Inpatient and outpatient expenses directly related to a Transplant Occurrence. Charges made by a Physician or Transplant team. Compatibility testing of prospective organ donors who are immediate family members. For the purpose of this coverage, an immediate family member is defined as a first-degree biological relative. These are your: biological parent, sibling or child. Charges for activating the donor search process with national registries. Charges made by a Hospital or outpatient facility and/or Physician for the medical and surgical expenses of a live donor, but only to the extent not covered by another plan or program. Related supplies and services provided by the facility during the Transplant Occurrence process. These services and supplies may include: physical, speech and occupational therapy; biomedicals and immunosuppressants; Home Health Services and home infusion services. Any Copayments or Coinsurance associated with Transplants are set forth in the Schedule of Benefits. Copayments or Coinsurance apply per Transplant Occurrence. One Transplant Occurrence includes the following four phases of Transplant care: Pre-Transplant Evaluation/Screening: Includes all Transplant-related professional and technical components required for assessment, evaluation and acceptance into a Transplant facility s Transplant program. Pre-Transplant/Candidacy Screening: Includes HLA typing of immediate family members. Transplant Event: Includes inpatient and outpatient services for all Transplant-related health services and supplies provided to a Member and donor during the one or more surgical procedures or medical therapies for a Transplant; prescription drugs provided during the Member s inpatient stay or outpatient visit(s), including bio-medical and immunosuppressant HO SG2016COC SG Off Exchange
165 drugs; physical, speech or occupational therapy provided during the Member s inpatient stay or outpatient visit(s); cadaveric and live donor organ procurement. Follow-up Care: Includes Home Health Services; home infusion services; and Transplantrelated outpatient services rendered within 180 days from the date of the Transplant. For the purposes of this section, the following will be considered to be one Transplant Occurrence: Heart Lung Heart/ Lung Simultaneous Pancreas Kidney (SPK) Pancreas Kidney Liver Intestine Bone Marrow/Stem Cell Transplant Multiple organs replaced during one Transplant surgery Tandem Transplants (Stem Cell) Sequential Transplants Re-Transplant of same organ type within 180 days of the first Transplant Any other single organ Transplant, unless otherwise excluded under the coverage The following will be considered to be more than one Transplant Occurrence: Autologous Blood/Bone Marrow Transplant followed by Allogenic Blood/Bone Marrow Transplant (when not part of a tandem Transplant) Allogenic Blood/Bone Marrow Transplant followed by an Autologous Blood/Bone Marrow Transplant (when not part of a tandem Transplant) Re-Transplant after 180 days of the first Transplant Pancreas Transplant following a kidney Transplant A Transplant necessitated by an additional organ failure during the original Transplant surgery/process. More than one Transplant when not performed as part of a planned tandem or sequential Transplant, (e.g. a liver Transplant with subsequent heart Transplant). Benefit Limitations Unless specified above, not covered under this benefit are charges incurred for: Outpatient drugs including bio-medicals and immunosuppressants not expressly related to an outpatient transplant occurrence; Services that are covered under any other part of this plan; Services and supplies furnished to a donor when the recipient is not covered under this plan; Home infusion therapy after the transplant occurrence; Harvesting or storage of organs, without the expectation of immediate transplantation for an existing illness; Harvesting and/or storage of bone marrow, tissue or stem cells, without the expectation of transplantation within 12 months for an existing illness; Cornea (Corneal Graft with Amniotic Membrane) or Cartilage (autologous chondrocyte or autologous osteochondral mosaicplasty) transplants, unless otherwise authorized by Aetna. HO SG2016COC SG Off Exchange
166 6. Specific Therapies and Tests Diagnostic and Preoperative Testing Diagnostic Complex Imaging Benefit Covered Benefits include charges made on an outpatient basis by a Physician, Hospital or a licensed imaging or radiological facility for complex imaging services to diagnose an illness or injury, including: C.A.T. scans; Magnetic Resonance Imaging (MRI); Nuclear medicine imaging, including Positron Emission Tomography (PET) Scans; and Any other outpatient diagnostic imaging service costing over $500. Complex Imaging Expenses for preoperative testing will be payable under this benefit. Benefit Limitations: The plan does not cover diagnostic complex imaging expenses under this part of the plan if such imaging expenses are covered under any other part of the plan. Outpatient Diagnostic Lab Work Covered Benefits include charges for lab services, and pathology and other tests provided to diagnose an illness or injury. The charges must be made by a Physician, Hospital or licensed radiological facility or lab. Important Reminder: Refer to the Schedule of Benefits for details about any cost-sharing or benefit maximums that may apply to outpatient diagnostic testing, lab services and radiological services. Outpatient Diagnostic Radiological Services Covered Benefits include charges for radiological services (other than complex imaging services), provided to diagnose an illness or injury. The services must be provided by a Physician, Hospital or licensed radiological facility. Benefit Limitations: The plan does not cover diagnostic complex imaging expenses under this part of the plan if such imaging expenses are covered under any other part of the plan. Outpatient Preoperative Testing Prior to a scheduled covered surgery, Covered Benefits include charges made for tests performed by a Hospital, Physician or licensed diagnostic laboratory provided the charges for the surgery are Covered Benefits and the tests are: Related to your surgery, and the surgery takes place in a Hospital; Completed within 14 days before your surgery; Performed on an outpatient basis; HO SG2016COC SG Off Exchange
167 Covered if you were an inpatient in a Hospital; Not repeated in or by the Hospital where the surgery will be performed. Test results should appear in your medical record kept by the Hospital where the surgery is performed. Benefit Limitations: The plan does not cover diagnostic complex imaging expenses under this part of the plan if such imaging expenses are covered under any other part of the plan. If your tests indicate that surgery should not be performed because of your physical condition, the plan will pay for the tests, however surgery will not be covered. Important: Complex Imaging testing for preoperative testing is covered under the Diagnostic Complex Imaging Expense section. Separate cost sharing may apply. Refer to your Schedule of Benefits for information on cost sharing amounts for complex imaging. Clinical Trial Therapies (Experimental or Investigational Treatment) Covered Benefits include charges made by a provider for Experimental or Investigational drugs, devices, treatments or procedures under an approved clinical trial only when you have cancer or a terminal illness and all of the following conditions are met: You have been diagnosed with cancer, chronic fatigue syndrome, or a condition likely to cause death within one year or less; Standard therapies have not been effective or are inappropriate; Aetna determines, based on published, peer-reviewed scientific evidence that you may benefit from the treatment; and You are enrolled in an approved clinical trial that meets these criteria. An approved clinical trial is a clinical trial that meets these criteria: The FDA has approved the drug, device, treatment or procedure to be investigated or granted it investigational new drug (IND) or Group c/treatment IND status. This requirement does not apply to procedures and treatments that do not require FDA approval; The clinical trial has been approved by an Institutional Review Board that will oversee the investigation; The clinical trial is sponsored by the National Cancer Institute (NCI) or similar federal organization; The trial conforms to standards of the NCI or other applicable federal organization. The clinical trial takes place at an NCI-designated cancer center or takes place at more than one institution; and You are treated in accordance with the protocols of that study. Clinical Trials (Routine Patient Costs) Covered Benefits include "routine patient costs" furnished to you in connection with participation in an "approved clinical trial as a qualified individual" for cancer or other life-threatening disease or condition, as those terms are defined in the federal Public Health Service Act, Section HO SG2016COC SG Off Exchange
168 Not covered under this Plan are: Services and supplies related to data collection and record-keeping that is solely needed due to the clinical trial (i.e. protocol-induced costs); Services and supplies provided by the trial sponsor without charge to the Member; and The experimental intervention itself (except medically necessary Category B investigational devices and promising experimental or investigational interventions for terminal illnesses in certain clinical trials in accordance with Aetna s claim policies). Important Notes: 3. Refer to the Schedule of Benefits for details about cost sharing and any benefit maximums that apply to the Clinical Trial benefit. 4. These Clinical Trial benefits are subject to all of the terms; conditions; provisions; limitations; and exclusions of this Plan including, but not limited to, any precertification and referral requirements. Outpatient Therapies Outpatient Infusion Therapy Benefit Covered Benefits include infusion therapy you receive in an outpatient setting. An outpatient setting includes but is not limited to: A free-standing outpatient facility The outpatient department of a Hospital A Physician in his/her office or in your home The list of preferred infusion locations can be found by contacting Member Services by logging onto your Aetna Navigator secure member website at or calling the number on the back of your ID card. Certain infused medications may be covered under the prescription drug plan. You can access the list of Specialty Care Prescription Drugs by contacting Member Services or by logging onto your Aetna Navigator secure member website at or calling the number on the back of your ID card to determine if coverage is under the prescription drug plan or this certificate. Infusion therapy is the intravenous or continuous administration of medications or solutions that are medically necessary for your course of treatment. Charges for the following outpatient infusion therapy services and supplies are covered expenses: Pharmaceutical when administered in connection with infusion therapy and any medical supplies, equipment and nursing services required to support the infusion therapy; Professional services; Total parenteral nutrition (TPN); Chemotherapy; Drug therapy (includes antibiotic and antivirals); Pain management (narcotics); and Hydration therapy (includes fluids, electrolytes, and other additives). Infusion therapy is the intravenous administration of prescribed medications or solutions. HO SG2016COC SG Off Exchange
169 Benefit Limitations: Not included under this infusion therapy benefit are charges incurred for: Enteral nutrition; Blood transfusions and blood products; and Insulin. Chemotherapy Covered Benefits include charges for chemotherapy treatment. Coverage levels depend on where treatment is received. In most cases, chemotherapy is covered as outpatient care. Inpatient Hospitalization for chemotherapy is limited to the initial dose while Hospitalized for the diagnosis of cancer and when a Hospital stay is otherwise Medically Necessary based on your health status. Radiation Therapy Benefit Covered Benefits include charges for the treatment of illness by x-ray, gamma ray, accelerated particles, mesons, neutrons, radium or radioactive isotopes. Short-Term Cardiac and Pulmonary Rehabilitation Therapy Services Benefit Covered Benefits include short-term rehabilitation therapy services, as described below provided in a hospital, when prescribed by a Physician. All services are subject to precertification by Aetna. The services have to be performed by: A licensed or certified physical or occupational therapist; or A physician. The following are Covered Benefits for short term rehabilitation therapy services: Cardiac Rehabilitation Benefits Cardiac rehabilitation benefits are available as part of a Member s inpatient Hospital stay. A course of outpatient cardiac rehabilitation appropriate for your condition is covered when Medically Necessary for a cardiac condition that can be changed. The plan will cover charges in accordance with a treatment plan as determined by your risk level when recommended by a Physician. Pulmonary Rehabilitation Benefits Pulmonary rehabilitation benefits are available as part of a Member s inpatient Hospital stay. A course of outpatient pulmonary rehabilitation appropriate for your condition is covered when Medically Necessary for the treatment of reversible pulmonary disease states. HO SG2016COC SG Off Exchange
170 Benefit Limitations Unless specifically covered above, not covered under this benefit are charges for: Any services which are covered expenses in whole or in part under any other group plan sponsored by an employer; Any services unless provided in accordance with a specific treatment plan; Services not performed by a physician or under the direct supervision of a physician; Services provided by a physician or physical or occupational therapist who resides in your home; or who is a member of your family, or a member of your spouse s family; or your domestic partner. Special education to instruct a person whose speech has been lost or impaired, to function without that ability. This includes lessons in sign language. Short-Term Rehabilitation and Habilitation Therapy Services Benefit Covered Benefits include charges for short-term rehabilitation therapy services, as described below, when prescribed by a Physician up to the benefit maximums listed on your Schedule of Benefits. The services have to be performed by: A licensed or certified physical, occupational or speech therapist; A Hospital, Skilled Nursing Facility, or Hospice Facility; A Home Health Care Agency; or A Physician. Cognitive Therapy, Physical Therapy, Occupational Therapy, Speech Therapy Rehabilitation Benefits Coverage is subject to the limits, if any, shown on the Schedule of Benefits. For inpatient rehabilitation benefits for the services listed below, refer to the Inpatient Hospital and Skilled Nursing Facility benefits provision under the Covered Benefits section of this Certificate. Physical therapy is covered for non-chronic conditions and acute illnesses and injuries provided the therapy is expected to: - Significantly improve, develop or restore physical functions lost; or - Improves any impaired function as a result of an acute illness, injury or surgical procedure. Physical therapy does not include educational training except for treatment of Autism Spectrum Disorders. Occupational therapy, (except for vocational rehabilitation or employment counseling), is covered for non-chronic conditions and acute illnesses and injuries provided the therapy is expected to: - Significantly improve, develop or restore physical functions lost as a result of an acute illness, injury or surgical procedure; or - Improve an impaired function as a result of an acute illness, injury or surgical procedure; or - To relearn skills to significantly improve independence in the activities of daily living. Occupational therapy does not include educational training except for treatment of Autism Spectrum Disorders. HO SG2016COC SG Off Exchange
171 Speech therapy is covered for non-chronic conditions and acute illnesses and injuries provided the therapy is expected to: - Significantly improve or restore the speech function or correct a speech impairment resulting from illness, injury or surgical procedure; or; - Improve delays in speech function development as a result of a gross anatomical defect present at birth. Speech function is the ability to express thoughts, speak words and form sentences. Speech impairment is difficulty with expressing one s thoughts with spoken words. Cognitive rehabilitation is covered when the cognitive deficits have been acquired as a result of neurologic impairment due to trauma, stroke, or encephalopathy, and when the therapy is coordinated with Aetna as part of a treatment plan intended to restore previous cognitive function. Benefit Limitations Unless specifically covered above, not covered under this benefit are charges for: Educational services for Down's Syndrome and Cerebral Palsy, for example, as they are considered both developmental and/or chronic in nature; Any services unless provided in accordance with a specific treatment plan; Services provided during a stay in a hospital, skilled nursing facility, or hospice facility except as stated above; Services not performed by a physician or under the direct supervision of a physician; Treatment covered as part of the Spinal Manipulation Care. This applies whether or not benefits have been paid under that section; Special education to instruct a person whose speech has been lost or impaired, to function without that ability. This includes lessons in sign language. Spinal Manipulation Care Benefit Covered benefits include Chiropractic care services including diagnostic and treatment services utilized in an office setting by Participating Chiropractic Physicians and Osteopaths. Chiropractic treatment includes the conservative management of neuromusculoskeletal conditions through manipulation and ancillary physiological treatment rendered to specific joints to restore motion, reduce pain and improve function. Habilitation Therapy Treatment Covered Benefits include habilitation therapy services your physician prescribes. The services have to be performed by: A licensed or certified physical, occupational or speech therapist A Hospital, Skilled Nursing Facility, or Hospice Facility A Home Health Care Agency A Physician Habilitation therapy services have to follow a specific treatment plan, ordered by your Physician, that: Details the treatment, and specifies frequency and duration, and Provides for ongoing reviews and is renewed only if continued therapy is appropriate. Allows therapy services, provided in your home, if you are homebound HO SG2016COC SG Off Exchange
172 Outpatient Physical, Occupational, and Speech Therapy Covered Benefits under Habilitation Therapy Treatment include: Physical therapy, if it is expected to: - Develop any impaired function Occupational therapy (except for vocational rehabilitation or employment counseling), if it is expected to: - Develop any impaired function, or - Relearn skills to significantly develop your independence in the activities of daily living Speech therapy is covered provided the therapy is expected to: - Develop speech function as a result of delayed development (Speech function is the ability to express thoughts, speak words and form sentences). Short-Term Rehabilitation and Habilitation Therapy Services benefit limitations Unless specifically covered above, not covered under this benefit are charges for: Educational services for Down's Syndrome and Cerebral Palsy, for example, as they are considered both developmental and/or chronic in nature; Any services unless provided in accordance with a specific treatment plan; Services provided during a stay in a hospital, skilled nursing facility, or hospice facility except as stated above; Services not performed by a physician or under the direct supervision of a physician; Treatment covered as part of the Chiropractic Treatment. This applies whether or not benefits have been paid under that section; Special education to instruct a person whose speech has been lost or impaired, to function without that ability. This includes lessons in sign language. 7. Other Covered Benefits Acupuncture Benefit The plan covers charges made for acupuncture services provided by a physician, if the service is performed as a form of anesthesia in connection with a covered surgical procedure. Administration of Blood and Blood Products Covered Benefits include the administration, cost, and processing of blood and blood products. Coverage also includes fees related to autologous blood donations. Ambulance Service Covered Benefits include charges made by a professional Ambulance, as follows: Ground Ambulance Covered Benefits include charges for transportation: To the first Hospital where treatment is given in a medical emergency. From one Hospital to another Hospital in a medical emergency when the first Hospital does not have the required services or facilities to treat your condition. From Hospital to home or to another facility when other means of transportation would be considered unsafe due to your medical condition. HO SG2016COC SG Off Exchange
173 From home to Hospital for covered inpatient or outpatient treatment when other means of transportation would be considered unsafe due to your medical condition. When during a covered inpatient stay at a Hospital, Skilled Nursing Facility or acute rehabilitation Hospital, an Ambulance is required to safely and adequately transport you to or from inpatient or outpatient Medically Necessary treatment. Air or Water Ambulance Covered Benefits include charges for transportation to a Hospital by air or water Ambulance when: Ground Ambulance transportation is not available; and Your condition is unstable, and requires medical supervision and rapid transport; and In a medical emergency, transportation from one Hospital to another Hospital; when the first Hospital does not have the required services or facilities to treat your condition and you need to be transported to another Hospital; and the two conditions above are met. Benefit Limitations: Not covered under this benefit are charges incurred to transport you: If an Ambulance service is not required by your physical condition; or If the type of Ambulance service provided is not required for your physical condition; or By any form of transportation other than a professional Ambulance service. Non-emergency transport by fixed wing aircraft. Bariatric Surgery Covered Benefits for the treatment of morbid obesity include one bariatric surgical procedure including related outpatient services, within a two-year period beginning with the date of the first bariatric surgical procedure, unless a multi-stage procedure is planned. Benefit Limitations: Unless specified above, not covered under this benefit are charges incurred for: Weight control services including open vertical banded gastroplasty, laparoscopic vertical banded gastroplasty, open sleeve gastrectomy, laparoscopic sleeve gastrectomy, open adjustable gastric banding, medical treatments, weight control/loss programs, dietary regimens and supplements, food or food supplements, appetite suppressants and other medications; exercise programs, exercise or other equipment; and other services and supplies that are primarily intended to control weight or treat obesity, including morbid obesity, or for the purpose of weight reduction, regardless of the existence of comorbid conditions; except as provided in the Certificate. Disposable Outpatient Supplies Covered benefits for medically necessary supplies, including ostomy supplies, which may be considered disposable are required for a Member in a course of treatment for a specific medical condition. Supplies must be obtained from a provider. Limitations Unless specified above, not covered under this benefit are charges incurred for: Over the counter supplies, such as band-aids and gauze. HO SG2016COC SG Off Exchange
174 Durable Medical Equipment (DME) Benefit Coverage is provided for Durable Medical Equipment. The wide variety of Durable Medical Equipment and continuing development of patient care equipment makes it impractical to provide a complete listing, therefore, the Aetna Medical Director has the authority to approve requests on a caseby-case basis. Covered Durable Medical Equipment includes those items covered by Medicare unless excluded in the Exclusions and Limitations section of this Certificate. Aetna reserves the right to provide the most cost efficient and least restrictive level of service or item which can be safely and effectively provided. The decision to rent or purchase is at the discretion of Aetna. Instruction and appropriate services required for the Member to properly use the item, such as attachment or insertion, is also covered upon precertification by Aetna. Replacement, repairs and maintenance are covered only if it is demonstrated to the Aetna that: It is needed due to a change in the Member s physical condition; or It is likely to cost less to buy a replacement than to repair the existing equipment or to rent like equipment. All maintenance and repairs that result from a misuse or abuse are a Member s responsibility. Family Planning Services - Other Covered Benefits include charges for the following family planning services, even though not provided to treat an illness or injury: Voluntary termination of pregnancy; and Voluntary sterilization for males. Benefit Limitations: Not covered under this benefit are charges incurred for: Reversal of voluntary sterilization procedures, for males and females including related follow-up care; Charges for services which are covered to any extent under any other part of this plan; and Charges incurred for family planning services while confined as an inpatient in a Hospital or other facility. Important Notes: Refer to the Schedule of Benefits for details about cost sharing and benefit maximums that apply to Family Planning Services - Other. For more information, see the sections on Family Planning Services - Female Contraceptives, Pregnancy Expenses and Treatment of Infertility in this Certificate. Hearing Aid Benefit Covered Benefits for hearing care includes charges for hearing exams, prescribed hearing aids and hearing aid expenses as described below. HO SG2016COC SG Off Exchange
175 Hearing aid means: Any wearable, non-disposable instrument or device designed to aid or compensate for impaired human hearing; and Parts, attachments or accessories. Covered Benefits include the following: Charges for an audiometric hearing exam and evaluation for a hearing aid prescription performed by: - A Physician certified as an otolaryngologist or otologist; or - An audiologist who (1) is legally qualified in audiology; or (2) holds a certificate of Clinical Competence in Audiology from the American Speech and Hearing Association in the absence of any licensing requirements; and who performs the exam at the written direction of a legally qualified otolaryngologist or otologist. Charges for electronic hearing aids, installed in accordance with a Prescription written during a covered hearing exam; Any other related services necessary to access, select and adjust or fit a hearing aid. Covered Benefits for hearing aids will not include per 12 consecutive month period: Charges for more than one hearing aid per ear; and Charges in excess of any maximum amount shown on the Schedule of Benefits. Hearing Aids Alternate Treatment Rule Sometimes there are several types of hearing aids that can be used to treat a medical condition, all of which provide acceptable results. When alternate hearing aids can be used, the plan s coverage may be limited to the cost of the least expensive device that is: Customarily used nationwide for treatment, and Deemed by the medical profession to be appropriate for treatment of the condition in question. The device must meet broadly accepted standards of medical practice, taking into account your physical condition. You should review the differences in the cost of alternate treatment with your Physician. Of course, you and your Physician can still choose the more costly treatment method. You are responsible for any charges in excess of what the plan will cover. This Alternate Treatment Rule provision will not operate to deny benefits as mandated by any applicable state statute or regulation. Benefit Limitations: No benefits are payable under this benefit for charges incurred for: A service or supply which is received while the person is not a covered person under this Certificate; A replacement of: - A hearing aid installed within the prior 12 month period. Replacement parts or repairs for a hearing aid; Batteries or cords; A hearing aid that does not meet the specifications prescribed for correction of hearing loss: Any ear or hearing exam performed by a Physician who is not certified as an otolaryngologist or otologist; Any hearing aid furnished or ordered because of a hearing exam that was done before the date the person became covered under this Plan; HO SG2016COC SG Off Exchange
176 Any hearing care service or supply which is a Covered Benefits in whole or in part under any other part of this Plan; Any hearing care service or supply which does not meet professionally accepted standards; Any hearing exam: - Required by an employer as a condition of employment; or - Which an employer is required to provide under a labor agreement; or - Which is required by any law of government. Hearing exams given during a stay in a Hospital or other facility, except those provided to newborns as part of the overall Hospital stay; and Any tests, appliances and devices for the improvement of hearing including hearing aid batteries and auxiliary equipment or to enhance other forms of communication to compensate for hearing loss or devices that simulate speech. Oral and Maxillofacial Treatment (Mouth, Jaws and Teeth) Benefit Covered Benefits include charges made by a Physician, a Dentist and Hospital for: Non-surgical treatment of infections or diseases of the mouth, jaw joints or supporting tissues. Services and supplies for treatment of, or related conditions of, the teeth, mouth, jaws, jaw joints or supporting tissues, (this includes bones, muscles, and nerves), for surgery needed to: Treat a fracture, dislocation, or wound. Cut out cysts, tumors, or other diseased tissues. Cut into gums and tissues of the mouth. This is only covered when not done in connection with the removal, replacement or repair of teeth. Alter the jaw, jaw joints, or bite relationships by a cutting procedure when appliance therapy alone cannot result in functional improvement. Hospital services and supplies received for a stay required because of your condition. Dental work, surgery and orthodontic treatment needed to remove, repair, restore or reposition: Natural teeth damaged, lost, or removed; or Other body tissues of the mouth fractured or cut due to injury. Any such teeth must have been free from decay or in good repair, and are firmly attached to the jaw bone at the time of the injury. The treatment must begin within six months from the date of the injury. The treatment must be completed in the Calendar Year of the accident or in the next Calendar Year. If crowns, dentures, bridges, or in-mouth appliances are installed due to injury, covered benefits only include charges for: The first denture or fixed bridgework to replace lost teeth; The first crown needed to repair each damaged tooth; and An in-mouth appliance used in the first course of orthodontic treatment after the injury. HO SG2016COC SG Off Exchange
177 Jaw Joint Disorder Treatment Covered Benefits include charges made by a Physician, Hospital or surgery center for the diagnosis and treatment of jaw joint disorder. A jaw joint disorder is defined as a painful condition: Temporomandibular joint dysfunction (TMJ) syndrome; or Involving the relationship between the jaw joint and related muscles and nerves such as myofacial pain dysfunction (MPD). resulting from accident, trauma, a congenital defect, a developmental defect, or a pathology. Covered benefits include: Surgical treatment of the jaw joint itself Treatment that is recognized by the medical or dental profession as effective and appropriate treatment for TMJ, including intra-oral splints that stabilize the jaw joint. Medical Foods to Treat Inherited Metabolic Disorders and Formulas to Treat Eosinophilic Gastrointestinal Disorders Covered Benefits include the expenses incurred for the purchase of: Medically Necessary Medical Foods used in the therapeutic treatment of Inherited Metabolic Disorders, including Modified Low Protein Foods and Metabolic Formula; and Medically Necessary amino acid-based formulas necessary for the treatment of Eosinophilic Gastrointestinal Disorders, when prescribed or ordered by the Member s Participating Physician. Any applicable Copayments are set forth in the Schedule of Benefits. Prosthetic Device Benefit The Member s initial provision and replacement of a prosthetic device that temporarily or permanently replaces all or part of an external body part lost or impaired as a result of disease or injury or congenital defects is covered, when such device is prescribed by a Provider. Coverage includes repair and replacement when due to growth and development or a significant change in a Member s physical condition. Instruction and appropriate services required for the Member to properly use the item (such as attachment or insertion) are covered. Covered Benefits that are prosthetic devices include those items covered by Medicare unless excluded in the Exclusions and Limitations section of this Certificate. Aetna reserves the right to provide the most cost efficient and least restrictive level of service or item which can be safely and effectively provided. HO SG2016COC SG Off Exchange
178 Benefit Limitations The plan will not cover expenses and charges for, or expenses related to: Orthopedic shoes, therapeutic shoes, foot orthotics, or other devices to support the feet, unless required for the treatment of or to prevent complications of diabetes; or if the orthopedic shoe is an integral part of a covered leg brace; or Trusses, corsets, and other support items; or Repair and replacement due to loss, misuse, abuse or theft. Any item listed in the Exclusions and Limitations section of this Certificate. Vision Care Benefits Pediatric Routine Vision Exams Covered Benefits include charges made by a legally qualified ophthalmologist or optometrist for a routine vision exam. The exam will include refraction and glaucoma testing. Pediatric Vision Care Services and Supplies Covered Benefits include charges for the following vision care services and supplies: Preferred eyeglass frames, Prescription lenses or Prescription contact lenses identified by a vision Provider. These are eyeglass frames, Prescription lenses, or Prescription contact lenses that are covered at 100% by a vision Provider. Non-Preferred eyeglass frames, Prescription lenses or Prescription contact lenses that are not identified as Preferred by a vision Provider. Coverage includes charges incurred for: Non-conventional Prescription contact lenses that are required to correct visual acuity to 20/40 or better in the better eye and that correction cannot be obtained with conventional lenses.aphakic Prescription lenses prescribed after cataract surgery has been performed. Low vision services. A listing of the locations of the vision Providers under this Plan can be accessed at the website. Be sure to look at the appropriate vision Provider listing that applies to your plan, since different Aetna plans use different networks of providers. You must present your ID card to the vision Provider at the time of service. This benefit is subject to the maximums shown on the Schedule of Benefits. As to coverage for Prescription lenses in a calendar year, this benefit will cover either Prescription lenses for eyeglass frames or Prescription contact lenses, but not both. Benefit Limitations: Unless specified above, not covered under this benefit are charges incurred for services and supplies: Office visits to an ophthalmologist, optometrist or optician related to the fitting of Prescription contact lenses. Eyeglass frames, Prescription lenses and Prescription contact lenses that are not identified as Preferred by a vision Provider. Eyeglass frames, non-prescription lenses and non-prescription contact lenses that are for cosmetic purposes. HO SG2016COC SG Off Exchange
179 Adult Routine Vision Exams Covered Benefits include charges made by a legally qualified ophthalmologist or optometrist for a routine vision exam. The exam will include refraction and glaucoma testing. Benefit Limitations: Unless specified above, not covered under this benefit are charges incurred for services and supplies: Office visits to an ophthalmologist, optometrist or optician related to the fitting of Prescription contact lenses. Eyeglass frames, Prescription lenses and Prescription contact lenses that are not identified as Preferred by a vision Provider. Eyeglass frames, non-prescription lenses and non-prescription contact lenses that are for cosmetic purposes. Important Notes: Refer to the Schedule of Benefits for any cost-sharing, age limits, exam frequency limits and maximums that apply to vision exams, services and supplies. Pediatric Dental Services Covered Benefits include charges made by a Dental Provider for the dental services listed in the Pediatric Dental Care Schedule below and provided to covered persons through the end of the month in which the person turns 19. The plan does not pay a benefit for all dental care expenses that you incur. Important Reminder: Your dental services and supplies must meet the following rules to be covered by the plan: The services and supplies must be Medically Necessary. The services and supplies must be covered by the plan. You must be covered by the plan when you incur the expense. About the Dental Plan The plan is a Dental Plan that covers a limited range of dental services and supplies. You can visit the Dental Provider of your choice when you need dental care. You can choose a Dental Provider who is in the dental network. You have the freedom to choose a Dental Provider who is not in the dental network. You may pay more out of your own pocket when you choose a Non-Participating Dental Provider. HO SG2016COC SG Off Exchange
180 The Choice Is Yours You have a choice each time you need dental care: Using Non-Participating Dental Providers You can obtain dental care from Dental Providers who are not in the network. The plan covers out-of-network services and supplies but your expenses will generally be higher. The plan begins to pay benefits after you satisfy a Deductible. Non-Participating Dental Providers have not agreed to accept the Negotiated Charge. You will be reimbursed for a covered benefit received from a Non-Participating Dental Provider, up to the Recognized Charge and the maximum benefits under this plan, less any cost sharing required by you such as Deductibles and Copayments. Your Copayment is based on the Recognized Charge. You will have to pay any balance bills above the Recognized Charge for that covered service or supply. You will have to submit dental claims for treatment received from Non-Participating Dental Providers unless your Dental Provider takes care of claim submissions for you. When a Dental Provider submits a claim submission, Aetna will directly pay the Non-Participating Dental Provider less any cost sharing required by you. You will be responsible for Deductibles and Copayments, if any. You will receive notification of what the plan has paid toward your Covered Benefits. It will indicate any amounts you owe towards any Deductible, Copayment or other non-covered Benefits you have incurred. You may elect to receive this notification by , or through the mail. Contact Member Services by logging onto the Aetna website or calling the toll-free number on the back of your ID card if you have questions regarding your statement. Pediatric Dental Care Schedule If: A charge is made for an unlisted service given for the dental care of a specific condition; and The list includes one or more services that, under standard practices, are separately suitable for the dental care of that condition; then the charge will be considered to have been made for a service in the list that Aetna determines would have produced a professionally acceptable result. The Pediatric Dental Care Schedule is a list of dental benefits that are covered by the plan. There are several categories of Covered Benefits: Diagnostic and Preventive Care Basic Restorative Care Major Restorative Care Orthodontic Care These covered services and supplies are grouped as Type A, Type B, Type C and Orthodontic Expenses. Coverage is also provided for a Dental Emergency. For additional information, please refer later in this amendment to the In Case of a Dental Emergency section. HO SG2016COC SG Off Exchange
181 Getting an Advance Claim Review The purpose of the advance claim review is to determine, in advance, the benefits the plan will pay for proposed services. Knowing ahead of time which services are covered by the plan, and the benefit amount payable, helps you and your Dentist make informed decisions about the care you are considering. Important Note: The pre-treatment review process is not a guarantee of benefit payment, but rather an estimate of the amount or scope of benefits to be paid. When to Get an Advance Claim Review An advance claim review is recommended whenever a course of dental treatment is likely to cost more than $300. Ask your Dentist to write down a full description of the treatment you need, using either an Aetna claim form or an ADA approved claim form. Then, before actually treating you, your Dentist should send the form to Aetna. Aetna may request supporting images and other diagnostic records. Once all of the information has been gathered, Aetna will review the proposed treatment plan and provide you and your Dentist with a statement outlining the benefits payable by the plan. You and your Dentist can then decide how to proceed. The advance claim review is voluntary. It is a service that provides you with information that you and your Dentist can consider when deciding on a course of treatment. It is not necessary for emergency treatment or routine care such as cleaning teeth or check-ups. In determining the amount of benefits payable, Aetna will take into account alternate procedures, services, or courses of treatment for the dental condition in question in order to accomplish the anticipated result. (See the Alternate Treatment Rule later in this amendment for more information on alternate dental procedures.) What Is a Course of Dental Treatment? A course of dental treatment is a planned program of one or more services or supplies. The services or supplies are provided by one or more Dentists to treat a dental condition that was diagnosed by the attending Dentist as a result of an oral examination. A course of treatment starts on the date your Dentist first renders a service to correct or treat the diagnosed dental condition. In Case of a Dental Emergency If you need dental care for the palliative treatment (e.g., pain relieving, stabilizing) of a Dental Emergency, you are covered 24 hours a day, 7 days a week. A Dental Emergency is any dental condition which: Occurs unexpectedly; Requires immediate diagnosis and treatment in order to stabilize the condition; and Is characterized by symptoms such as severe pain and bleeding. Services provided for a Dental Emergency will be covered at the network level of benefits even if services and supplies are not provided by a Dental Provider. Rules and Limits That Apply to the Dental Benefits Several rules apply to the dental benefits. Following these rules will help you use the plan to your advantage by avoiding expenses that are not covered by the plan. HO SG2016COC SG Off Exchange
182 Waiting Period The plan has a waiting period for Orthodontic Treatment as follows: Orthodontic treatment: Your coverage will take effect after 24 months of continuous coverage under the Plan. Orthodontic Treatment Rule Orthodontic treatment is covered when it is medically necessary for a covered person under the age of 19 with a severe, dysfunctional, handicapping condition such as: Cleft lip and palate, cleft palate, or cleft lip with alveolar process involvement The following craniofacial anomalies: - Hemifacial microsomia; - Craniosynostosis syndromes; - Cleidocranial dental dysplasia; - Arthrogryposis; or - Marfan syndrome Anomalies of facial bones and/or oral structures Facial trauma resulting in functional difficulties Reimbursable orthodontic services include: Pre-orthodontic treatment visit Comprehensive orthodontic treatment Orthodontic retention (removal of appliances, construction and placement of retainers(s) This benefit does not cover charges for the following: Replacement of broken appliances; Re-treatment of orthodontic cases; Changes in treatment necessitated by an accident; Maxillofacial surgery; Myofunctional therapy; Lingually placed direct bonded appliances and arch wires (i.e. invisible braces ); or Removable acrylic aligners (i.e. invisible aligners ). Replacement Rule Crowns, inlays, onlays and veneers, complete dentures, removable partial dentures, fixed partial dentures (bridges) and other prosthetic services are subject to the plan's replacement rule. That means certain replacements of, or additions to, existing crowns, inlays, onlays, veneers, dentures or bridges are covered only when you give proof to Aetna that: You had a tooth (or teeth) extracted after the existing denture or bridge was installed. As a result, you need to replace or add teeth to your denture or bridge. The present crown, inlay and onlay, veneer, complete denture, removable partial denture, fixed partial denture (bridge), or other prosthetic service was installed at least 5 years before its replacement and cannot be made serviceable. Your present denture is an immediate temporary one that replaces that tooth (or teeth). A permanent denture is needed, and the temporary denture cannot be used as a permanent denture. Replacement must occur within 12 months from the date that the temporary denture was installed. HO SG2016COC SG Off Exchange
183 Tooth Missing but Not Replaced Rule The first installation of complete dentures, removable partial dentures, fixed partial dentures (bridges), and other prosthetic services will be covered if: The dentures, bridges or other prosthetic items are needed to replace one or more natural teeth; and The tooth that was removed was not an abutment to a removable or fixed partial denture installed during the prior 5 years. The extraction of a third molar does not qualify. Any such appliance or fixed bridge must include the replacement of an extracted tooth or teeth. Alternate Treatment Rule Sometimes there are several ways to treat a dental problem, all of which provide acceptable results. When alternate services or supplies can be used, the plan's coverage will be limited to the cost of the least expensive service or supply that is: Customarily used nationwide for treatment; and Deemed by the dental profession to be appropriate for treatment of the condition in question. The service or supply must meet broadly accepted standards of dental practice, taking into account your current oral condition. You should review the differences in the cost of alternate treatment with your Dental Provider. Of course, you and your Dental Provider can still choose the more costly treatment method. You are responsible for any charges in excess of what the plan will cover. Coverage for Dental Work Completed After Termination of Coverage Your dental coverage may end while you or your covered dependent is in the middle of treatment. The plan does not cover dental services that are given after your coverage terminates. There is an exception. The plan will cover the following services if they are ordered while you were covered by the plan, and installed within 30 days after your coverage ends. Inlays; Onlays; Crowns; Removable bridges; Cast or processed restorations; Dentures; Fixed partial dentures (bridges); and Root canals. "Ordered" means: For a denture: the impressions from which the denture will be made were taken. For a root canal: the pulp chamber was opened. For any other item: the teeth which will serve as retainers or supports, or the teeth which are being restored: - Must have been fully prepared to receive the item; and HO SG2016COC SG Off Exchange
184 Pediatric Dental Plan Exclusions Not every dental care service or supply is covered by the plan, even if prescribed, recommended, or approved by your Physician or Dental Provider. The plan covers only those services and supplies that are Medically Necessary. Charges made for the following are not covered except to the extent listed under the Covered Benefits section of the Certificate or by amendment attached to the Certificate. In addition, some services are specifically limited or excluded. This section describes services and supplies that are not covered or subject to special limitations. These dental exclusions are in addition to the exclusions that apply to health coverage. Acupuncture, acupressure and acupuncture therapy, except as provided in the Covered Benefits section of the Certificate. Any charges in excess of the benefit, dollar, day, visit, or supply limits stated in the Certificate. Any instruction for diet, plaque control and oral hygiene. Charges for a service or supply furnished by a Provider in excess of the Negotiated Charge. Charges submitted for services: - By an unlicensed Hospital, Physician or other provider; or - By a licensed Hospital, Physician or other provider that are not within the scope of the provider s license. Charges submitted for services that are not rendered, or not rendered to a person not eligible for coverage under the plan. Cosmetic services and supplies including plastic surgery, reconstructive surgery, Cosmetic surgery, personalization or characterization of dentures or other services and supplies which improve alter or enhance appearance, augmentation and vestibuloplasty, and other substances to protect, clean, whiten bleach or alter the appearance of teeth; whether or not for psychological or emotional reasons; except to the extent coverage is specifically provided in the Covered Benefits section of the Certificate. Facings on molar crowns and pontics will always be considered Cosmetic. Court ordered services, including those required as a condition of parole or release. Crown, inlays and onlays, and veneers unless: - It is treatment for decay or traumatic injury and teeth cannot be restored with a filling material; or - The tooth is an abutment to a covered partial denture or fixed bridge. Dental Examinations that are: - Required by a third party, including examinations and treatments required to obtain or maintain employment, or which an employer is required to provide under a labor agreement; - Required by any law of a government, securing insurance or school admissions, or professional or other licenses; - Required to travel, attend a school, camp, or sporting event or participate in a sport or other recreational activity; and - Any special medical reports not directly related to treatment except when provided as part of a covered service. Dental implants, braces, (that are determined not to be Medically Necessary), mouth guards, and other devices to protect, replace or reposition teeth and removal of implants. Dental services and supplies that are covered in whole or in part under any other part of this plan. Dentures, crowns, inlays, onlays, bridges, or other appliances or services used for the purpose of splinting, to alter vertical dimension, to restore occlusion, or correcting attrition, abrasion, abfraction or erosion. HO SG2016COC SG Off Exchange
185 Except as covered in the Covered Benefits section of the Certificate, treatment of any Jaw Joint Disorder and treatments to alter bite or the alignment or operation of the jaw, including temporomandibular joint disorder (TMJ) treatment, orthognathic surgery, and treatment of malocclusion or devices to alter bite or alignment. Experimental or Investigational drugs, devices, treatments or procedures, except as described in the What the Medical Benefit Covers section of the Certificate. General anesthesia and intravenous sedation, unless specifically covered and only when done in connection with another Medically Necessary covered service or supply. Medicare: Payment for that portion of the charge for which Medicare is the primary payer. Miscellaneous charges for services or supplies including: - Annual or other charges to be in a Physician s practice; - Charges to have preferred access to a Physician s services such as boutique or concierge Physician practices; - Cancelled or missed appointment charges or charges to complete claim forms; - Charges the recipient has no legal obligation to pay; or the charges would not be made if the recipient did not have coverage (to the extent exclusion is permitted by law) including: Care in charitable institutions; Care for conditions related to current or previous military service; Care while in the custody of a governmental authority; Any care a public Hospital or other facility is required to provide; or Any care in a Hospital or other facility owned or operated by any federal, state or other governmental entity, except to the extent coverage is required by applicable laws. Non-Medically Necessary services, including but not limited to, those treatments, services, Prescription Drugs and supplies which are not Medically Necessary, as determined by Aetna, for the diagnosis and treatment of illness, injury, restoration of physiological functions, or covered preventive services. This applies even if they are prescribed, recommended or approved by your Physician or Dentist. Orthodontic treatment except as covered in this amendment and in the Covered Benefits section of the Certificate. Pontics, crowns, cast or processed restorations made with high noble metals (gold). Prescribed drugs; pre-medication; or analgesia. Replacement of a device or appliance that is lost, missing or stolen, and for the replacement of appliances that have been damaged due to abuse, misuse or neglect and for an extra set of dentures. Replacement of teeth beyond the normal complement of 32. Routine dental exams and other preventive services and supplies, except as specifically provided in this amendment and in the Covered Benefits section of the Certificate. Services and supplies done where there is no evidence of pathology, dysfunction, or disease other than covered preventive services. Services and supplies provided for your personal comfort or convenience, or the convenience of any other person, including a provider. Services and supplies provided in connection with treatment or care that is not covered under the plan. Services rendered before the effective date or after the termination of coverage. Space maintainers except when needed to preserve space resulting from the premature loss of deciduous teeth. Surgical removal of impacted wisdom teeth only for orthodontic reasons. HO SG2016COC SG Off Exchange
186 Treatment by other than a Dentist or dental provider that is legally qualified to furnish dental services or supplies. Work related: Any illness or injury related to employment or self-employment including any injuries that arise out of (or in the course of) any work for pay or profit, unless no other source of coverage or reimbursement is available to you for the services or supplies. Sources of coverage or reimbursement may include your employer, workers compensation, or an occupational illness or similar program under local, state or federal law. A source of coverage or reimbursement will be considered available to you even if you waived your right to payment from that source. If you are also covered under a workers compensation law or similar law, and submit proof that you are not covered for a particular illness or injury under such law, that illness or injury will be considered non-occupational regardless of cause. HO SG2016COC SG Off Exchange
187 EXCLUSIONS AND LIMITATIONS Medical Exclusions The following are not Covered Benefits except as described in the Covered Benefits section of this Certificate or by amendment(s) attached to this Certificate: Acupuncture, acupressure and acupuncture therapy, except as provided in the Covered Benefits section of the Certificate. Ambulance services, for routine transportation to receive outpatient or inpatient services. Any non-emergency charges for Covered Benefits incurred outside of the United States. Behavioral health services that are not primarily aimed at treatment of illness, injury, restoration of physiological functions or that do not have a physiological or organic basis. Biofeedback, except as precertified by Aetna. Any related services including processing, storage or replacement costs, and the services of blood donors, apheresis or plasmapheresis are not covered. For autologous blood donations, only administration and processing costs are covered. Care for conditions that state or local laws require to be treated in a public facility, including but not limited to, mental illness commitments. Care furnished to provide a safe surrounding, including the charges for providing a surrounding free from exposure that can worsen the disease or injury. Charges, expenses, or costs in excess of Recognized Charge. Charges, expenses, or costs applied toward satisfaction of any applicable Deductible, Coinsurance, or Copayment amounts. Clinical trial therapies - Services and supplies related to data collection and record-keeping that is solely needed due to the clinical trial (i.e. protocol-induced costs) - Services and supplies provided by the trial sponsor without charge to you - The experimental intervention itself (except Medically Necessary Category B investigational devices and promising experimental and investigational interventions for terminal Illnesses in certain clinical trials in accordance with Aetna s claim policies). Contraception, except as specifically described in the Covered Benefit section including, but not limited to, over the counter contraceptive supplies such as condoms, contraceptive foams, jellies and ointments. HO SG2016COC SG Off Exchange
188 Cosmetic Surgery, or treatment relating to the consequences of, or as a result of, Cosmetic Surgery, other than Medically Necessary Services. This exclusion includes, but is not limited to, surgery to correct gynecomastia and breast augmentation procedures, and otoplasties. Reduction mammoplasty, except when determined to be Medically Necessary by an Aetna Medical Director, is not covered. This exclusion does not apply to surgery to correct the results of injuries causing the impairment, or as a continuation of a staged reconstruction procedure, or congenital defects necessary to restore normal bodily functions, including but not limited to, cleft lip and cleft palate or surgery required for post-mastectomy reconstruction. Court ordered services, or those required by court order as a condition of parole or probation. Custodial Care. Dental services except as specifically covered in the Covered Benefits section including but not limited to, services related to the care, filling, removal or replacement of teeth and treatment of injuries to or diseases of the teeth, dental services related to the gums, apicoectomy (dental root resection), orthodontics, root canal treatment, soft tissue impactions, bony impacted teeth, alveolectomy, augmentation and vestibuloplasty treatment of periodontal disease, false teeth, prosthetic restoration of dental implants, and dental implants. This exclusion does not include bone fractures, removal of tumors, and odontogenic cysts. Educational services except as specifically covered in the Covered Benefits section and treatment of behavioral disorders, together with services for remedial education including evaluation or treatment of learning disabilities, minimal brain dysfunction, developmental and learning disorders, behavioral training, and cognitive rehabilitation. This includes services, treatment or educational testing and training related to behavioral (conduct) problems, learning disabilities, or developmental delays. Special education, including lessons in sign language to instruct a Member, whose ability to speak has been lost or impaired, to function without that ability, are not covered. Experimental or Investigational Procedures, or ineffective surgical, medical, psychiatric, or dental treatments or procedures, research studies, or other experimental or investigational health care procedures or pharmacological regimes as determined by Aetna, unless precertified by Aetna. This exclusion will not apply with respect to drugs: - That have been granted treatment investigational new drug (IND) or Group c/treatment IND status; - That are being studied at the Phase III level in a national clinical trial sponsored by the National Cancer Institute; or - Aetna has determined that available scientific evidence demonstrates that the drug is effective or the drug shows promise of being effective for the disease. E-Visits Non-Participating Providers. Any services that are given by Providers that are not contracted with Aetna as E-visit Providers. Any services that are not provided during an internet-based consult or via telephone. Foot orthotics unless required for the treatment of, or to prevent, complications of diabetes. HO SG2016COC SG Off Exchange
189 Habilitation Therapy Services -- Physical, Occupational and Speech Therapy Services for the treatment of delays in development, including speech development, unless as a result of a gross anatomical defect present at birth, including: Therapies to treat delays in development and/or chronic conditions. Examples of noncovered diagnoses that are considered both developmental and/or chronic in nature are: - Down syndrome Any service unless provided in accordance with a specific treatment plan Services you get from a Home Health Care Agency. Services not given by a Physician (or under the direct supervision of a Physician), physical, occupational or speech therapist. This exclusion does not apply to physical therapy, occupational therapy or speech therapy provided for the treatment of Autism Spectrum Disorder. Hair analysis. Hearing aids. Related services and supplies, except as specifically described in this Certificate. Home births. Home uterine activity monitoring. Household equipment, including but not limited to, the purchase or rental of exercise cycles, water purifiers, hypo-allergenic pillows, mattresses or waterbeds, whirlpool or swimming pools, exercise and massage equipment, central or unit air conditioners, air purifiers, humidifiers, dehumidifiers, escalators, elevators, ramps, stair glides, emergency alert equipment, handrails, heat appliances, improvements made to a Member s house or place of business, and adjustments made to vehicles. Hypnotherapy, except when precertified by Aetna. Implantable drugs. Infertility. Any services, treatments, procedures or supplies that are designed to enhance fertility or the likelihood of conception, such as: - Drugs, and drugs related to the treatment of non-covered benefits. - Injectable infertility medication, including but not limited to menotropins, hcg, and GnRH agonists. - Reversal of voluntary sterilization including related procedures, services and supplies. - The purchase of donor sperm and any charges for the storage of sperm. - All charges associated with surrogacy for you or the surrogate. A surrogate is a female carrying her own genetically related child where the child is conceived with the intention of turning the child over to be raised by others, including the biological father. - Home ovulation prediction kits or home pregnancy tests. - Medication that is experimental and investigational in relation to infertility. - The purchase of donor embryos, donor oocytes, or donor sperm. - Charges associated with cryopreservation or storage of cryopreserved eggs and embryos (e.g., office, hospital, ultrasounds, laboratory tests, etc.), including thawing charges. HO SG2016COC SG Off Exchange
190 - All charges associated with the care of the donor in a donor egg cycle. This includes, but is not limited to, any payments to the donor, donor screening fees, fees for lab tests, and any charges associated with care of the donor required for donor egg retrievals or transfers. - All charges associated with the use of a gestational carrier for the female acting as the gestational carrier. A gestational carrier is a female carrying an embryo to which she is not genetically related. - Comprehensive infertility services and ART services that are not medically necessary. - Any charges associated with obtaining sperm for ART services. - Ovulation induction with menotropins, Intrauterine insemination and any related services, products or procedures. - In vitro fertilization (IVF), Zygote intrafallopian transfer (ZIFT), Gamete intra-fallopian transfer (GIFT), Cryopreserved embryo transfers and any related services, products or procedures (such as Intracytoplasmic sperm injection (ICSI) or ovum microsurgery). Mental health treatment Mental health services for the following categories (or equivalent terms as listed in the most recent version of the International Classification of Diseases (ICD)): - Dementias and amnesias without behavioral disturbances - Sexual deviations and disorders except for gender identity disorders - Tobacco use disorders - Specific disorders of sleep - Antisocial or dissocial personality disorder - Pathological gambling, kleptomania, pyromania - Specific delays in development (learning disorders, academic underachievement) - Intellectual disability - Wilderness Treatment Programs or any such related or similar programs, school and/or education services. Military service related diseases, disabilities or injuries for which the Member is legally entitled to receive treatment at government facilities and which facilities are reasonably available to the Member. Missed appointment charges. Non-medically necessary services, including but not limited to, those services and supplies: - Which are not Medically Necessary, as determined by Aetna, for the diagnosis and treatment of illness, injury, restoration of physiological functions, or covered preventive services; - That do not require the technical skills of a medical, mental health or a dental professional; - Furnished mainly for the personal comfort or convenience of the Member, or any person who cares for the Member, or any person who is part of the Member s family, or any Provider; - Furnished solely because the Member is an inpatient on any day in which the Member s disease or injury could safely and adequately be diagnosed or treated while not confined; - Furnished solely because of the setting if the service or supply could safely and adequately be furnished in a Physician s or a dentist s office or other less costly setting. Non-prescription drugs and medicines, except as provided on an inpatient basis or as specifically covered in the Covered Benefits section. HO SG2016COC SG Off Exchange
191 Non-surgical treatment of temporomandibular joint disorder (TMJ), including but not limited to, treatment performed by prosthesis placed directly on the teeth, surgical and non-surgical medical and dental services, and diagnostic or therapeutics services related to TMJ. Nursing and aide services provided outside of the home (such as in conjunction with school, vacation, work or recreational activities). Outpatient supplies, including but not limited to, medical consumable or disposable supplies such as syringes, incontinence pads, elastic stockings, and reagent strips, except as described in the Covered Benefits section. Outpatient prescription contraceptive drugs and devices - Oral drugs that are Brand-Name Prescription Drugs and Biosimilar Prescription Drugs. - Injectable drugs that are Brand-Name Prescription Drugs and Biosimilar Prescription Drugs. - Vaginal rings that are Generic Prescription Drugs, Brand-Name Prescription Drugs and Biosimilar Prescription Drugs. - Transdermal contraceptive patches that are Generic Prescription Drugs, Brand-Name Prescription Drugs and Biosimilar Prescription Drugs. - Female contraceptive devices that are brand-name devices. - FDA-approved female brand-name and biosimilar emergency contraceptives and brandname over-the-counter (OTC) emergency contraceptives. - Other FDA-approved female and male brand-name over-the-counter (OTC) contraceptives. Payment for that portion of the benefit for which Medicare or another party is the primary payer. Personal comfort or convenience items, including those services and supplies not directly related to medical care, such as guest meals and accommodations, barber services, telephone charges, radio and television rentals, homemaker services, travel expenses, take-home supplies, and other like items and services. Private Duty Nursing (See the Home Health Benefits section regarding coverage of nursing services). Recreational, educational, and sleep therapy, including any related diagnostic testing. Religious, marital and sex counseling, including services and treatment related to religious counseling, marital/relationship counseling, and sex therapy. Reversal of voluntary sterilizations, including related follow-up care and treatment of complications of such procedures. Routine foot/hand care, including routine reduction of nails, calluses and corns. Services for which a Member is not legally obligated to pay in the absence of this coverage. HO SG2016COC SG Off Exchange
192 Services for the treatment of sexual dysfunctions or inadequacies, including therapy, supplies, or counseling for sexual dysfunctions or inadequacies that do not have a physiological or organic basis. Services, including those related to pregnancy, rendered before the effective date or after the termination of the Member s coverage, unless coverage is continued under the Continuation section of this Certificate. Services performed by a relative of a Member for which, in the absence of any health benefits coverage, no charge would be made. Services required by third parties, including but not limited to, physical examinations, diagnostic services and immunizations in connection with obtaining or continuing employment, obtaining or maintaining any license issued by a municipality, state, or federal government, securing insurance coverage, travel, school admissions or attendance, including examinations required to participate in athletics, except when such examinations are considered to be part of an appropriate schedule of wellness services. Services which are not a Covered Benefit under this Certificate. Short-Term Rehabilitation Services -- Outpatient Cognitive Rehabilitation, Physical, Occupational and Speech Therapy Services for the treatment of delays in development, including speech development, unless as a result of a gross anatomical defect present at birth, including: Therapies to treat delays in development and/or chronic conditions. Examples of non-covered diagnoses that are considered both developmental and/or chronic in nature are: - Down syndrome - Cerebral palsy Any service unless provided in accordance with a specific treatment plan Services you get from a Home Health Care Agency. Services provided by a Physician, or treatment covered as part of the spinal manipulation benefit. This applies whether or not benefits have been paid under the spinal manipulation section. - Services not given by a Physician (or under the direct supervision of a Physician), physical, occupational or speech therapist. This exclusion does not apply to physical therapy, occupational therapy or speech therapy provided for the treatment of Autism Spectrum Disorder. Specific non-standard allergy services and supplies, including but not limited to, skin titration (wrinkle method), cytotoxicity testing (Bryan's Test), treatment of non-specific candida sensitivity, and urine autoinjections. Specific injectable drugs, except as provided in the Covered Benefits section of the Certificate, including: - Experimental drugs or medications, or drugs or medications that have not been proven safe and effective for a specific disease or approved for a mode of treatment by the Food and Drug Administration (FDA) and the National Institutes of Health (NIH); - Needles, syringes and other injectable aids; - Drugs related to the treatment of non-covered services; and HO SG2016COC SG Off Exchange
193 - Drugs related to the treatment of Infertility, contraception, and performance enhancing steroids. Special medical reports, including those not directly related to treatment of the Member, e.g., employment or insurance physicals, and reports prepared in connection with litigation. Telemedicine: Any services that are given by providers that are not contracted with Aetna as telemedicine providers. Any services that are provided other than during an internet-based consult or via telephone. Therapy or rehabilitation, including but not limited to, primal therapy, chelation therapy, rolfing, psychodrama, megavitamin therapy, purging, bioenergetic therapy, vision perception training, and carbon dioxide. Thermograms and thermography. Treatment in a federal, state, or governmental entity, including care and treatment provided in a non-participating Hospital owned or operated by any federal, state or other governmental entity, except to the extent required by applicable laws. Treatment of mental retardation, defects, and deficiencies. This exclusion does not apply to mental health services or to medical treatment of mentally retarded Members in accordance with the benefits provided in the Covered Benefits section of this Certificate. Treatment of occupational injuries and occupational diseases, including those injuries that arise out of (or in the course of) any work for pay or profit, or in any way results from a disease or injury which does. If a Member is covered under a Workers' Compensation law or similar law, and submits proof that the Member is not covered for a particular disease or injury under such law, that disease or injury will be considered "non-occupational" regardless of cause. Vision: Vision-related services and supplies, except as described in the Covered Benefits section. In addition, the plan does not cover: - Special supplies such as non-prescription sunglasses; - Vision service or supply which does not meet professionally accepted standards; - Special vision procedures, such as orthoptics or vision training; - Eye exams during your stay in a Hospital or other facility for health care; - Eyeglasses or duplicate or spare eyeglasses or lenses or frames; - Replacement of lenses or frames that are lost or stolen or broken; - Acuity tests; - Eye Surgery for the correction of vision, including radial keratotomy, LASIK and similar procedures; - Services to treat errors of refraction. HO SG2016COC SG Off Exchange
194 Weight control services including surgical procedures, medical treatments, weight control/loss programs, dietary regimens and supplements, food or food supplements, appetite suppressants and other medications; exercise programs, exercise or other equipment; and other services and supplies that are primarily intended to control weight or treat obesity, including Morbid Obesity, or for the purpose of weight reduction, regardless of the existence of comorbid conditions except as provided by this Certificate. Wilderness treatment programs (whether or not the program is part of a licensed residential treatment facility, or otherwise licensed institution), educational services, schooling or any such related or similar program, including therapeutic programs within a school setting. Limitations In the event there are 2 or more alternative Medical Services which in the sole judgment of Aetna are equivalent in quality of care, Aetna reserves the right to provide coverage only for the least costly Medical Service, as determined by Aetna, provided that Aetna pre-authorizes the Medical Service or treatment. Determinations regarding eligibility for benefits, coverage for services, benefit denials and all other terms of this Certificate are at the sole discretion of Aetna, subject to the terms of this Certificate. HO SG2016COC SG Off Exchange
195 TERMINATION OF COVERAGE A Member s coverage under this Certificate will terminate upon the earliest of any of the conditions listed below and termination will be effective on the date indicated on the Aetna Certificate.. Termination of Subscriber Coverage A Subscriber s coverage will terminate for any of the following reasons: Employment terminates; The Group Policy or Aetna Group Agreement terminates; The Subscriber is no longer eligible as outlined in this Certificate; The Subscriber becomes covered under an alternative health benefit plan or under any other plan which is offered by, through, or in connection with, the Contract Holder in lieu of coverage under this Certificate. Termination of Dependent Coverage A Covered Dependent s coverage will terminate for any of the following reasons: A Covered Dependent is no longer eligible, as outlined in this Certificate; The Group Policy or Aetna Group Agreement terminates; or The Subscriber s coverage terminates; Coverage of a dependent will not terminate if the Subscriber becomes enrolled under a group Medicare + Choice plan offered by Aetna or one of its affiliates. However, the dependent s coverage will terminate if the Subscriber s coverage terminates under the Medicare + Choice plan. Termination For Cause Aetna may terminate coverage for cause: Upon 60 days advance written notice, if the Contract Holder or Member has failed to make any required premium payment which the Contract Holder or Member is obligated to pay. Upon the effective date of such termination, prepayments received by Aetna on account of such terminated Member or Members for periods after the effective date of termination shall be refunded to Contract Holder. Upon 60 days advance written notice, upon discovering a material misrepresentation by the Contract Holder in applying for or obtaining coverage or benefits under this Certificate or discovering that the Contract Holder has committed fraud against Aetna. A Member may register a Complaint with Aetna, as described in the Complaints and Appeals, External Review and Dispute Resolution sections of the Aetna Certificate, after receiving notice that Aetna has or will terminate the Member s coverage as described in the Termination For Cause subsection of the Certificate. Aetna will continue the Member s coverage in force until a final decision on the Complaint is rendered, provided the Premium is paid throughout the period prior to the issuance of that final decision. Aetna may rescind coverage, to the date coverage would have terminated had the Member not registered a Complaint with Aetna, if the final decision is in favor of Aetna. If coverage is rescinded, Aetna will provide the Member with a 60 day advance written notice prior to the date of the rescission, and refund any Premiums paid for any period after the termination date, minus the cost of Covered Benefits provided to a Member during this period. HO SG2016COC SG Off Exchange
196 Coverage will not be terminated on the basis of a Member s health status or health care needs, nor if a Member has exercised the Member s rights under the Certificate s Complaints and Appeals, External Review, and Dispute Resolution sections to register a Complaint with Aetna. The Complaint process described in the preceding paragraph applies only to those terminations affected pursuant to the Termination for Cause subsection of the Certificate. Aetna shall have no liability or responsibility under this Certificate for services provided on or after the date of termination of coverage. The fact that Members are not notified by the Contract Holder of the termination of their coverage due to the termination of the Group Policy shall not continue the Members' coverage beyond the date coverage terminates. CONTINUATION A Member is entitled to the Continuation provisions as described in the Aetna Certificate of Coverage. CLAIMS PROCEDURE, COMPLAINTS AND APPEALS AND EXTERNAL REVIEW/DISPUTE RESOLUTION The procedures described in the Aetna Certificate of Coverage govern Complaints and Appeals made or submitted by Members regarding coverage under this Certificate. COORDINATION OF BENEFITS The benefits provided under this Certificate will be subject to Coordination of Benefits as described in the Aetna Certificate of Coverage. RESPONSIBILITY OF MEMBERS Members or applicants shall complete and submit to Aetna such application or other forms or statements as Aetna may reasonably request. Members represent that all information contained in such applications, forms and statements submitted to Aetna incident to enrollment under this Certificate or the administration herein shall be true, correct, and complete to the best of the Member s knowledge and belief. The Member shall notify Aetna immediately of any change of address for the Member or any of the Subscriber s Covered Dependents, unless a different notification process is agreed to between Aetna and Contract Holder. The Member understands that Aetna is acting in reliance upon all information provided to it by the Member at time of enrollment and afterwards and represents that information so provided is true and accurate. HO SG2016COC SG Off Exchange
197 By electing coverage pursuant to this Certificate, or accepting benefits hereunder, all Members who are legally capable of contracting, and the legal representatives of all Members who are incapable of contracting, at time of enrollment and afterwards, represent that all information so provided is true and accurate and agree to all terms, conditions and provisions in this Certificate. GENERAL PROVISIONS Identification Card The identification card issued by Aetna to Members pursuant to this Certificate is for identification purposes only. Possession of an Aetna identification card confers no right to services or benefits under this Certificate, and misuse of such identification card may be grounds for termination of Member s coverage pursuant to the Termination of Coverage section of this Certificate. If the Member who misuses the card is the Subscriber, coverage may be terminated for the Subscriber as well as any of the Covered Dependents. To be eligible for services or benefits under this Certificate, the holder of the card must be a Member on whose behalf all applicable Premium charges under this Certificate have been paid. Any person receiving services or benefits which such person is not entitled to receive pursuant to the provisions of this Certificate shall be charged for such services or benefits at billed charges. If any Member permits the use of the Member s Aetna identification card by any other person, such card may be retained by Aetna, and all rights of such Member and their Covered Dependents, if any, pursuant to this Certificate shall be terminated immediately, subject to the Claim Procedures/Complaints and Appeals/Dispute Resolution in this Certificate. Reports and Records Aetna is entitled to receive from any Provider of services to Members, information reasonably necessary to administer this Certificate subject to all applicable confidentiality requirements as defined in the General Provisions section of this Certificate. By accepting coverage under this Certificate, the Subscriber, for himself or herself, and for all Covered Dependents covered hereunder, authorizes each and every Provider who renders services to a Member hereunder to: Disclose all facts pertaining to the care, treatment and physical condition of the Member to Aetna, or a medical, dental, or mental health professional that Aetna may engage to assist it in reviewing a treatment or claim; Render reports pertaining to the care, treatment and physical condition of the Member to Aetna, or a medical, dental, or mental health professional that Aetna may engage to assist it in reviewing a treatment or claim; and Permit copying of the Member s records by Aetna. Assignment of Benefits All rights of the Member to receive benefits hereunder are personal to the Member and may not be assigned, subject to the following sentence. A Member s right to receive payment for benefits will be assigned to a Provider, unless the Member provides evidence that the Member has already paid the Provider. HO SG2016COC SG Off Exchange
198 Legal Action No action at law or in equity may be maintained against Aetna for any expense or bill unless and until the appeal process has been exhausted, and in no event prior to the expiration of 60 days after written submission of claim has been furnished in accordance with requirements set forth in the Group Policy. No action shall be brought after the expiration of 3 years after the time written submission of claim is required to be furnished. Confidentiality Information contained in the medical records of Members and information received from any Provider incident to the provider-patient relationship shall be kept confidential in accordance with applicable law. Information may be used or disclosed by Aetna when necessary for a Member s care or treatment, the operation of Aetna and administration of this Certificate, or other activities, as permitted by applicable law. Members can obtain a copy of Aetna s Notice of Information Practices by calling the Member Services toll-free telephone number listed on the Member s identification card. Incontestability In the absence of fraud, all statements made by a Member shall be considered representations and not warranties, and no statement shall be the basis for voiding coverage or denying a claim after the Group Policy has been in force for 2 years from its effective date, unless the statement was material to the risk and was contained in a written application. Additional Provisions The following additional provisions apply to your coverage: This Certificate applies to coverage only, and does not restrict a Member s ability to receive health care benefits that are not, or might not be, Covered Benefits. Contract Holder hereby makes Aetna coverage available to persons who are eligible under the Eligibility section of this Certificate. However, this Certificate shall be subject to amendment, modification or termination in accordance with any provision hereof, by operation of law, by filing with and approval by the state Department of Insurance. This can also be done by mutual written agreement between Aetna and Contract Holder without the consent of Members. Aetna may adopt policies, procedures, rules and interpretations to promote orderly and efficient administration of this Certificate. No agent or other person, except an authorized representative of Aetna, has authority to waive any condition or restriction of this Certificate, to extend the time for making a payment, or to bind Aetna by making any promise or representation or by giving or receiving any information. No change in this Certificate shall be valid unless evidenced by an endorsement to it signed by an authorized representative of Aetna. The Health Network Option Open Access Program contract is a dual contract, consisting of the Aetna Group Agreement, and the Aetna Group Policy. The Aetna Group Agreement consists of the Group Agreement, Certificate of Coverage, Schedule of Benefits, any riders, and any amendments, endorsements, inserts, or attachments. The Aetna Group Policy consists of the HO SG2016COC SG Off Exchange
199 Group Insurance Policy, Group Insurance Certificate, Schedule of Benefits, any riders, and any amendments, endorsements, inserts, or attachments This Certificate, including the Schedule of Benefits and any amendments, endorsements, inserts, or attachments, is part of a dual certificate, to be used in conjunction with the Aetna Certificate of Coverage, which is made up of the Aetna Certificate of Coverage, Schedule of Benefits, any riders, and any amendments, endorsements, inserts, or attachments. These documents constitute the entire certificate between the parties hereto pertaining to the subject matter hereof and supersedes all prior and contemporaneous arrangements, understandings, negotiations and discussions of the parties with respect to the subject matter hereof, whether written or oral. There are no warranties, representations, or other agreements between the parties in connection with the subject matter hereof, except as specifically set forth in this Certificate. No supplement, modification or waiver of this Certificate shall be binding unless executed in writing by authorized representatives of the parties. This Certificate has been entered into and shall be construed according to applicable state and federal law. From time to time Aetna may offer or provide Members access to discounts on health care related goods or services. While Aetna has arranged for access to these goods, services and/or third party provider discounts, the third party service providers are liable to the Members for the provision of such goods and/or services. Aetna is not responsible for the provision of such goods and/or services nor is it liable for the failure of the provision of the same. Further, Aetna is not liable to the Members for the negligent provision of such goods and/or services by third party service providers. These discounts are subject to modification or discontinuance without notice. Discount and Wellness Programs Discount Arrangements: From time to time, Aetna may offer, provide, or arrange for discount arrangements or special rates from certain service Providers such as pharmacies, optometrists, dentist, alternative medicine, wellness and healthy living providers to Members or persons who become Members. Some of these arrangements may be available through third parties who may make payments to Aetna in exchange for making these services available. The third party service Providers are independent contractors and are solely responsible to Members for the provision of any such goods and/or services. Aetna reserves the right to modify or discontinue such arrangements at any time. These discount arrangements do not constitute benefits provided under the Group Policy. There are no benefits payable to Members nor does Aetna compensate Providers for services they may render. Wellness and Other Incentives We may encourage and incent you to access certain medical services, to use online tools that enhance your coverage and services, and to continue participation as an Aetna member. You and your doctor can talk about these medical services and decide if they are right for you. We may also encourage and incent you in connection with participation and outcome related thereto in a wellness or health improvement program. Incentives include but are not limited to: modifications to copayment, deductible, or coinsurance amounts; premium discounts or rebates; contributions to a health savings account; fitness center membership reimbursement; merchandise; coupons; gift cards; debit cards; or any combination of thereof. The award of any such incentive shall not depend upon the result of a wellness or health improvement activity or upon a member's health status. HO SG2016COC SG Off Exchange
200 Proof of Loss and Claims Payment The following provisions apply only as they relate to breast pump services and supplies obtained from a Non-Participating Provider under the Preventive Care Benefit. For more information refer to the Preventive Care Benefit earlier in this amendment. Proof of Loss: Written proof of loss must be furnished to Aetna within 90 days after a Member incurs expenses for Covered Benefits. Failure to furnish the proof of loss within the time required will not invalidate nor reduce any claim if it is not reasonably possible to give the proof of loss within 90 days, provided the proof of loss is furnished as soon as reasonably possible. However, except in the absence of legal capacity of the claimant, the proof of loss may not be furnished later than one year from the date when the proof of loss was originally required. A proof of loss form may be obtained from Aetna or the Contract Holder. If the Member does not receive such form before the expiration of 15 working days after Aetna receives the request, the Member shall be deemed to have complied with the requirements of this Certificate upon submitting within the time fixed in this Certificate written proof covering the occurrence, character and extent of the loss for which claim is made. Time for Payment of Claim: Benefits payable under this Certificate will be paid promptly after the receipt by Aetna of satisfactory proof of loss. If any portion of a claim is contested by Aetna, the uncontested portion of the claim will be paid promptly after the receipt of proof of loss by Aetna. Payment of Claims: All or any portion of any indemnities provided by the Certificate on account of Hospital, nursing, medical or surgical services shall be paid to the Subscriber. Any payment made by Aetna in good faith pursuant to this provision will fully discharge Aetna s obligation to the extent of the payment. The Member may request that payments not be made pursuant to this provision. The request must be made in writing and must be given to Aetna not later than the time of filing proof of loss. Payment made prior to receipt of the Member s written request at Aetna s principal executive office will be deemed to be payment made in good faith. Financial Sanctions Exclusions: If coverage provided under this policy violates or will violate any economic or trade sanctions, the coverage is immediately considered invalid. For example, Aetna companies cannot make payments for health care or other claims or services if it violates a financial sanction regulation. This includes sanctions related to a blocked person or a country under sanction by the United States, unless it is permitted under a written license from the Office of Foreign Asset Control (OFAC). For more information visit HO SG2016COC SG Off Exchange
201 DEFINITIONS The following words and phrases when used in this Certificate shall have, unless the context clearly indicates otherwise, the meaning given to them below: Aetna Health Insurance Company (AHIC), a Pennsylvania domiciled insurance company. Aetna Benefits The benefits covered under the Aetna Group Policy and Insurance Certificate. Ambulance A vehicle that is staffed with medical personnel and equipped to transport an ill or injured person. Autism Spectrum Disorder This means one of the following disorders as defined in the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association: Autistic Disorder; Rett s Disorder; Childhood Disintegrative Disorder; Asperger's Syndrome; and Pervasive Developmental Disorder--Not Otherwise Specified. Behavioral Health Provider A licensed organization or professional providing diagnostic, therapeutic or psychological services for behavioral health conditions. Behavioral Therapy Any interactive behavioral therapies derived from evidence-based research, including but not limited to: Applied Behavior Analysis; cognitive behavioral therapy; or other therapies supported by evidence of the effective treatment of individuals diagnosed with Autism Spectrum Disorder. Body Mass Index A practical marker that is used to assess the degree of obesity and is calculated by dividing the weight in kilograms by the height in meters squared. Calendar Year A period of 1 year commencing on January 1 st and ending at 12:00 midnight on December 31 st. Certificate This Certificate, including the Schedule of Benefits and any amendments, endorsements, inserts, or attachments, which outlines coverage for a Subscriber and Covered Dependents according to the Group Policy. HO SG2016COC SG Off Exchange
202 Coinsurance The portion of Covered Expenses which a Member must pay for care, after first meeting a Deductible amount. A Member does not have to pay Coinsurance after the Member reaches the individual and family Maximum Out-of-Pocket Limits, if any, as listed on the Schedule of Benefits. Continuous Period of Disability Any and all successive Hospital stays unless Aetna receives satisfactory evidence that a successive Hospital stay: Is due to causes not related to those of the earlier stay; Occurs after full recovery from the causes of the earlier Hospital stay; or The later Hospital stay occurs after the Member has completed a period of 90 days without a Hospital confinement. Contract Holder An employer or organization who agrees to remit the Premiums for coverage under the Group Policy payable to Aetna. The Contract Holder shall act only as an agent of Aetna Members in the Contract Holder's group, and shall not be the agent of Aetna for any purpose. Copayment The specified dollar amount or percentage required to be paid by or on behalf of a Member in connection with benefits, if any, as set forth in the Schedule of Benefits. Copayments may be changed by Aetna upon 30 days written notice to the Contract Holder. Cosmetic Services or supplies that alter, improve or enhance appearance. Cosmetic Surgery Any non-medically necessary surgery or procedure whose primary purpose is to improve or change the appearance of any portion of the body to improve self-esteem, but which does not restore bodily function, correct a diseased state, physical appearance, or disfigurement caused by an accident, birth defect, or correct or naturally improve a physiological function. Cosmetic Surgery includes, but is not limited to, ear piercing, rhinoplasty, lipectomy, surgery for sagging or extra skin, any augmentation or reduction procedures (e.g., mammoplasty, liposuction, keloids, rhinoplasty and associated surgery) or treatment relating to the consequences or as a result of Cosmetic Surgery. Covered Dependent Any person in a Subscriber s family who meets all the eligibility requirements of the Eligibility section of this Certificate has enrolled in Aetna, and is subject to Premium requirements set forth in the Premiums section of the Group Policy. Covered Benefits Those Medically Necessary Services and supplies set forth in this Certificate, which are covered subject to all of the terms and conditions of the Group Policy and this Certificate. Covered Expenses The Recognized Charge rate charged for Covered Benefits recognized under this Certificate as eligible for inclusion in calculating reimbursement. HO SG2016COC SG Off Exchange
203 Custodial Care Services and supplies that are primarily intended to help a Member meet their personal needs. Care can be Custodial Care even if it is prescribed by a Physician, delivered by trained medical personnel, or even if it involves artificial methods (or equipment) such as feeding tubes, monitors, or catheters. Examples of Custodial Care include, but are not limited to: Changing dressings and bandages, periodic turning and positioning in bed, administering oral medication, watching or protecting a Member. Care of a stable tracheostomy, including intermittent suctioning. Care of a stable colostomy/ileostomy. Care of stable gastrostomy/jejunostomy/nasogastric tube (intermittent or continuous) feedings. Care of a stable indwelling bladder catheter, including emptying/changing containers and clamping tubing. Respite care, adult (or child) day care, or convalescent care. Helping a Member perform an activity of daily living, such as: walking, grooming, bathing, dressing, getting in and out of bed, toileting, eating, or preparing food. Any services that an individual without medical or paramedical training can perform or be trained to perform. Deductible The first payments up to a specified dollar amount which a Member must make in the applicable calendar year for Covered Benefits. Dentist A legally qualified Dentist or a Physician licensed to do the dental work he or she performs. Dental Provider This is: Any dentist; Group; Organization; Dental facility; or Other institution or person; that is legally qualified to furnish dental services or supplies. Detoxification The process whereby an alcohol or drug intoxicated or alcohol or drug dependent person is assisted, in a facility licensed by the appropriate regulatory authority, through the period of time necessary to eliminate, by metabolic or other means, the intoxicating alcohol or drug, alcohol or drug dependent factors or alcohol in combination with drugs as determined by a licensed Physician, while keeping the physiological risk to the patient at a minimum. Durable Medical Equipment (DME) Equipment, as determined by Aetna, which is a) made for and mainly used in the treatment of a disease or injury; b) made to withstand prolonged use; c) suited for use while not confined as an inpatient in the Hospital; d) not normally of use to persons who do not have a disease or injury; e) not for use in altering air quality or temperature; and f) not for exercise or training. HO SG2016COC SG Off Exchange
204 Effective Date of Coverage The commencement date of coverage under this Certificate as shown on the records of Aetna. Emergency Service Professional health services that are provided to treat a Medical Emergency. Experimental or Investigational Procedures Services or supplies that are, as determined by Aetna, experimental. A drug, device, procedure or treatment will be determined to be experimental if: There are insufficient outcomes data available from controlled clinical trials published in the peerreviewed literature to substantiate its safety and effectiveness for the illness or injury involved; or Approval required by the U. S. Food and Drug Administration (FDA) has not been granted for marketing; or A recognized national medical or dental society or regulatory agency has determined, in writing, that it is experimental or investigational, or for research purposes; or It is a type of drug, device, procedure, or treatment that is the subject of a Phase I or Phase II clinical trial or the experimental or research arm of a Phase III clinical trial, using the definition of phases indicated in regulations and other official actions and publications of the FDA and Department of Health and Human Services; or The written protocol or protocols used by the treating facility, or the protocol or protocols of any other facility studying substantially the same drug, device, procedure, or treatment, or the written informed consent used by the treating facility or by another facility studying the same drug, device, procedure, or treatment states that it is experimental or investigational, or for research purposes. Group Policy The Group Policy between Aetna and the Contract Holder, including the Group Application, this Certificate, including the Schedule of Benefits and any amendments, endorsements, inserts, or attachments, as subsequently amended by operation of law and as filed with and approved by the applicable public authority. Habilitation Health care services that help a person keep, learn, or improve skills and functioning for daily living. Examples include therapy for a child who isn't walking or talking at the expected age. These services may include physical and occupational therapy, speech-language pathology and other services for people with disabilities in a variety of inpatient and/or outpatient settings. Health Professional(s) A Physician or other professional who is properly licensed or certified to provide medical care under the laws of the state where the individual practices, and who provides Medical Services which are within the scope of the individual s license or certificate. Homebound Member A Member who is confined to their place of residence due to an illness or injury which makes leaving the home medically contraindicated or if the act of transport would be a serious risk to their life or health. Examples where a Member would not be considered homebound are: A Member who does not often travel from home because of feebleness and/or insecurity brought on by advanced age (or otherwise). HO SG2016COC SG Off Exchange
205 A wheelchair bound Member who could safely be transported via wheelchair accessible transport. Home Health Services Those items and services provided by Providers as an alternative to hospitalization, and coordinated and precertified by Aetna. Hospice Care A program of care that is provided by a Hospital, Skilled Nursing Facility, hospice, or a duly licensed Hospice Care agency, and is approved by Aetna, and is focused on a palliative rather than curative treatment for Members who have a medical condition and a prognosis of less than 12 months to live. Hospital(s) An institution rendering inpatient and outpatient services, accredited as a Hospital by the Joint Commission on Accreditation of Health Care Organizations, the Bureau of Hospitals of the American Osteopathic Association, or as otherwise determined by Aetna as meeting reasonable standards. A Hospital may be a general, acute care, rehabilitation or specialty institution. Infertile or Infertility A disease defined by the failure to conceive a pregnancy after 12 months or more of timed intercourse or egg-sperm contact for women under age 35 (or 6 months for women age 35 or older). Jaw Joint Disorder This is: A Temporomandibular Joint (TMJ) dysfunction or any similar disorder of the jaw joint; or A Myofacial Pain Dysfunction (MPD); or Any similar disorder in the relationship between the jaw joint and the related muscles and nerves. L.P.N. A licensed practical or vocational nurse. Medical Community A majority of Physicians who are Board Certified in the appropriate specialty. Medical Emergency The existence of a medical condition manifesting itself by acute symptoms of sufficient severity (including severe pain) such that a prudent layperson, who possesses an average knowledge of health and medicine, could reasonably expect the absence of immediate medical attention to result in (i) placing the health of the individual (or, with respect to a pregnant woman, the health of the woman and her unborn child) in serious jeopardy; (ii) serious impairment to bodily functions; or (iii) serious dysfunction of any bodily organ or part. Medical Foods This means Modified Low Protein Foods and Metabolic Formula. HO SG2016COC SG Off Exchange
206 Medical Services The professional services of Health Professionals, including medical, surgical, diagnostic, therapeutic, preventive care and birthing facility services. Medically Necessary, Medically Necessary Services, or Medical Necessity These are health care or dental services that Aetna determines a Physician, other health care Provider or Dental Provider, exercising prudent clinical judgment, would give to a patient for the purpose of: preventing; evaluating; diagnosing; or treating: an Illness; an Injury; a disease; or its symptoms. The provision of the service, supply must, as Aetna determines, be: In accordance with generally accepted standards of medical or dental practice; Clinically appropriate, in terms of type, frequency, extent, site and duration, and considered effective for the patient's Illness, Injury or disease; and Not mostly for the convenience of the patient, Physician, other health care or Dental Provider; and And do not cost more than an alternative service or sequence of services at least as likely to produce the same therapeutic or diagnostic results as to the diagnosis or treatment of that patient's Illness, Injury, or disease. Generally accepted standards of medical or dental practice means: Standards that are based on credible scientific evidence published in peer-reviewed medical literature. They must be generally recognized by the relevant medical or dental community; Standards set forth in policy issues involving clinical judgment Member(s) A Subscriber or Covered Dependent as defined in this Certificate. Mental Disorders This is an illness commonly understood to be a Mental Disorder, whether or not it has a physiological basis, and for which treatment is generally provided by or under the direction of a Behavioral Health Provider such as a Psychiatrist, a psychologist or a psychiatric social worker. The following conditions are considered a Mental Disorder under this plan: Anorexia/Bulimia Nervosa. Bipolar disorder. Major depressive disorder. Obsessive compulsive disorder. Panic disorder. Pervasive Mental Developmental Disorder (including Autism). Psychotic Disorders/Delusional Disorder. Schizo-affective Disorder. Schizophrenia. HO SG2016COC SG Off Exchange
207 Also included is any other mental condition which requires Medically Necessary treatment. Metabolic Formula Foods that are all of the following: formulated to be consumed or administered internally under the supervision of the Member s Participating Physician. processed or formulated to be deficient in one or more of the nutrients present in typical foodstuffs. administered for the medical and nutritional management of a Member who has limited capacity to metabolize foodstuffs or certain nutrients contained in the foodstuffs or who has other specific nutrient requirements as established by medical evaluation. essential to a Member s optimal growth, health and metabolic homeostasis. Modified Low Protein Foods Foods that encompass those foods described in bullets 1, 3 and 4 under the definition of Metabolic Formula, and also the following: processed or formulated to contain less than one gram of protein per unit of serving, but does not include a natural food that is naturally low in protein. Morbid Obesity A Body Mass Index that is: greater than 40 kilograms per meter squared; or equal to or greater than 35 kilograms per meter squared with a high risk comorbid medical condition, including significant cardiovascular disease, sleep apnea, or uncontrolled type-2 diabetes. Negotiated Charge As to Health Coverage: The Negotiated Charge is the maximum charge a Non-Participating Provider has agreed to make as to any service or supply for the purpose of the benefits under this plan. Non-Hospital Facility A facility, licensed by the appropriate regulatory authority, for the care or treatment of alcohol or drug dependent persons, except for transitional living facilities. Non-Participating Dental Provider A Dental Provider not designated as an Aetna Participating Dental Provider. Non-Participating Infertility Specialist A Specialist who has entered into a contractual agreement with Aetna for the provision of Infertility services to Members. Non-Participating Providers A Provider not designated as an Aetna Participating Provider or such other Provider not part of the Aetna network. Non-Referred Benefits Covered Benefits under this Certificate received from Non-Participating Providers without a prior Referral issued by the Member s Aetna Primary Care Physician. HO SG2016COC SG Off Exchange
208 Open Enrollment Period A period each calendar year, when eligible enrollees of the Contract Holder may enroll in Aetna without a waiting period or exclusion or limitation based on health status or, if already enrolled in Aetna, may transfer to an alternative health plan offered by the Contract Holder. Orthodontic Treatment This is any: Medical service or supply; or Dental service or supply; furnished to prevent or to diagnose or to correct a misalignment: Of the teeth; or Of the bite; or Of the jaws or jaw joint relationship; whether or not for the purpose of relieving pain. The following are not considered orthodontic treatment: The installation of a space maintainer; or A surgical procedure to correct malocclusion. Partial Hospitalization The provision of medical, nursing, counseling or therapeutic services on a planned and regularly scheduled basis in a Hospital or Non-Hospital Facility which is licensed as an alcohol or drug abuse or mental illness treatment program by the appropriate regulatory authority, and which is designed for a patient or client who would benefit from more intensive services than are offered in outpatient treatment but who does not require inpatient care. Participating A description of a Provider that has entered into a contractual agreement with Aetna for the provision of services to Members. Physician(s) A duly licensed member of a medical profession, who has an M.D. or D.O. degree, who is properly licensed or certified to provide medical care under the laws of the state where the individual practices, and who provides Medical Services which are within the scope of the individual s license or certificate. Precertification, Precertify, Precertified A certification from Aetna that a Member must obtain prior to receiving any of the services that are identified by this Certificate as needing Precertification in order to receive unreduced benefits. Premium(s) The amount the Contract Holder or Member is required to pay to Aetna to continue coverage. HO SG2016COC SG Off Exchange
209 Primary Care Physician (PCP) A Participating Physician who supervises, coordinates and provides initial care and basic Medical Services as a general or family care practitioner, or in some cases, as an internist or a pediatrician to Members, initiates their Referral for Specialist care, and maintains continuity of patient care. Provider(s) A Physician, Health Professional, Hospital, Skilled Nursing Facility, Dental Provider, home health agency or other recognized entity or person licensed to provide Hospital Services, Medical Services, or dental services to Members. Psychiatric Hospital This is an institution that meets all of the following requirements: Mainly provides a program for the diagnosis, evaluation, and treatment of Substance Abuse or mental disorders. Is not mainly a school or a custodial, recreational or training institution. Provides infirmary-level medical services. Also, it provides, or arranges with a Hospital in the area for, any other medical service that may be required. Is supervised full-time by a Psychiatrist who is responsible for patient care and is there regularly. Is staffed by Psychiatrists involved in care and treatment. Has a Psychiatrist present during the whole treatment day. Provides, at all times, Psychiatric social work and nursing services. Provides, at all times, Skilled Nursing Services by licensed nurses who are supervised by a full-time R.N. Prepares and maintains a written plan of treatment for each patient based on medical, psychological and social needs. The plan must be supervised by a Psychiatrist. Makes charges. Meets licensing standards. Psychiatric Physician This is a physician who: Specializes in psychiatry; or Has the training or experience to do the required evaluation and treatment of Substance Abuse or Mental Disorders. Psychiatrist This is a Physician who: Specializes in psychiatry; or Has the training or experience to do the required evaluation and treatment of Substance Abuse or Mental Disorders. HO SG2016COC SG Off Exchange
210 Recognized Charge The amount of an out-of-network provider s charge that is eligible for coverage. You are responsible for all amounts above the recognized charge. The recognized charge may be less than the provider s full charge. Your plan s recognized charge applies to all out-of-network covered expenses except out-of-network emergency services. It applies even to charges from an out-of-network provider in a hospital that is a network provider. In all cases, the recognized charge is determined based on the Geographic Area where you receive the service or supply. Except as otherwise specified below, the recognized charge for each service or supply is the lesser of what the provider bills and: For professional services and for other services or supplies not mentioned below: - 90% of the Medicare allowable rate For services of hospitals and other facilities: - 90% of the Medicare allowable rate For prescription drugs: - 50% of the Average wholesale price (AWP) For dental expenses: - 80% of the prevailing charge rate We have the right to apply Aetna reimbursement policies. Those policies may further reduce the recognized charge. These policies take into account factors such as: The duration and complexity of a service When multiple procedures are billed at the same time, whether additional overhead is required Whether an assistant surgeon is necessary for the service If follow up care is included Whether other characteristics modify or make a particular service unique When a charge includes more than one claim line, whether any services described by a claim line are part of or incidental to the primary service provided and The educational level, licensure or length of training of the provider Aetna reimbursement policies are based on our review of: The Centers for Medicare and Medicaid Services (CMS) National Correct Coding Initiative (NCCI) and other external materials that say what billing and coding practices are and are not appropriate Generally accepted standards of medical and dental practice and The views of physicians and dentists practicing in the relevant clinical areas We use commercial software to administer some of these policies. Some policies are different for professional services than for facility services. HO SG2016COC SG Off Exchange
211 Special terms used Average Wholesale Price (AWP), Geographic Area, Prevailing Charge Rate, Medicare Allowable Rates, are defined as follows: Average Wholesale Price (AWP) Is the current average wholesale price of a prescription drug listed in the Facts and Comparisons Mediaspan weekly price updates (or any other similar publication chosen by Aetna). Geographic Area The Geographic area made up of the first three digits of the U.S. Postal Service zip codes. If we determine we need more data for a particular service or supply, we may base rates on a wider Geographic Area such as an entire state. Medicare Allowable Rates Except as specified below, these are the rates CMS establishes for services and supplies provided to Medicare enrollees. We update our systems with these revised rates within 180 days of receiving them from CMS. If Medicare does not have a rate, we will determine the rate as follows: Use the same method CMS uses to set Medicare rates. Look at what other providers charge. Look at how much work it takes to perform a service. Look at other things as needed to decide what rate is reasonable for a particular service or supply. Exceptions: For inpatient services, our Medicare Allowable Rate excludes amounts CMS allocates for Operating Indirect Medical Education (IME) and Direct Graduate Medical Education (DGME). Our rate also excludes other payments which CMS may make directly to hospitals, and for any retroactive adjustments made by CMS. Prevailing Charge Rates: The percentile value reported in a database prepared by FAIR Health, a nonprofit company. FAIR Health changes these rates periodically. Aetna updates its systems with these changes within 180 days after receiving them from FAIR Health. If the Fair Health database becomes unavailable, Aetna has the right to substitute an alternative database that Aetna believes is comparable. Additional information: Get the most value out of your benefits. Use the Estimate the Cost of Care tool on Aetna Navigator to help decide whether to get care in network or out-of-network. Aetna s secure member website at may contain additional information which may help you determine the cost of a service or supply. Log on to Aetna Navigator to access the Estimate the Cost of Care feature. Within this feature, view our Cost of Care and Member Payment Estimator tools. HO SG2016COC SG Off Exchange
212 Residential Treatment Facility (Mental Disorders) This is an institution that meets all of the following requirements: Is accredited by one of the following agencies, commissions or committees for the services being provided: The Joint Commission (TJC), Committee on Accreditation of Rehabilitation Facilities (CARF), American Osteopathic Association s Healthcare Facilities Accreditation Program (HFAP) or the Council on Accreditation (COA); or is credentialed by Aetna; Meets all applicable licensing standards established by the jurisdiction in which it is located; Performs a comprehensive patient assessment preferably before admission, but at least upon admission; Creates individualized active treatment plans directed toward the alleviation of the impairment that caused the admission; Has the ability to involve family/support systems in the therapeutic process; Has the level of skilled intervention and provision of care must be consistent with the patient s illness and risk; Provides access to psychiatric care by a psychiatrist as necessary for the provision of such care; Provides treatment services that are managed by a behavioral health provider who functions under the direction/supervision of a medical director; and Is not a wilderness treatment program (whether or not the program is part of a licensed residential treatment facility, or otherwise licensed institution), educational services, schooling or any such related or similar program, including therapeutic programs within a school setting. In addition to the above requirements, for Mental Health Residential Treatment Programs: A behavioral health provider must be actively on duty 24 hours per day for 7 days a week; The patient is treated by a psychiatrist at least once per week; and The medical director must be a psychiatrist. Residential Treatment Facility (Substance Abuse) This is an institution that meets all of the following requirements: Is accredited by one of the following agencies, commissions or committees for the services being provided: The Joint Commission (TJC), Committee on Accreditation of Rehabilitation Facilities (CARF), American Osteopathic Association s Healthcare Facilities Accreditation Program (HFAP), or the Council on Accreditation (COA); or is credentialed by Aetna; Meets all applicable licensing standards established by the jurisdiction in which it is located; Performs a comprehensive patient assessment preferably before admission, but at least upon admission; Creates individualized active treatment plans directed toward the alleviation of the impairment that caused the admission; Has the ability to involve family and/or support systems in the therapeutic process; Has the level of skilled intervention and provision of care that is consistent with the patient s illness and risk; Provides access to psychiatric care by a psychiatrist as necessary for the provision of such care; Provides treatment services that are managed by a behavioral health provider who functions under the direction/supervision of a medical director; and Is not a wilderness treatment program (whether or not the program is part of a licensed residential treatment facility, or otherwise licensed institution), educational services, schooling or any such related or similar program, including therapeutic programs within a school setting. HO SG2016COC SG Off Exchange
213 In addition to the above requirements, for Chemical Dependence Residential Treatment Programs: Is a behavioral health provider or an appropriately state certified professional (for example, CADC, CAC); Is actively on duty during the day and evening therapeutic programming; and The medical director must be a physician who is an addiction specialist. In addition to the above requirements, for Chemical Dependence Detoxification Programs within a residential setting: An R.N. is onsite 24 hours per day for 7 days a week; and The care must be provided under the direct supervision of a physician. Self-Referral, Self-Referred The process whereby a Member receives Covered Benefits under this Aetna Certificate from Providers without obtaining a prior Referral from the Aetna Primary Care Physician. Skilled Care Medical care that requires the skills of technical or professional personnel. Skilled Nursing Services that require the medical training of and are provided by a licensed nursing professional and are not Custodial Care. Skilled Nursing Facility An institution or a distinct part of an institution that is licensed or approved under state or local law, and which is primarily engaged in providing Skilled Nursing care and related services for residents who require medical or nursing care, or rehabilitation services for the rehabilitation of injured, disabled, or sick persons. Skilled Nursing Facility does not include institutions which provide only minimal care, Custodial Care services, ambulatory or part-time care services, or institutions which primarily provide for the care and treatment of Mental Disorder and Substance Abuse. The facility must qualify as a Skilled Nursing Facility under Medicare or as an institution accredited by the Joint Commission on Accreditation of Health Care Organizations, the Bureau of Hospitals of the American Osteopathic Association, the Commission on the Accreditation of Rehabilitative Facilities, or as otherwise determined by the health insurer to meet the reasonable standards applied by any of the aforesaid authorities. Examples of Skilled Nursing Facilities include Rehabilitation Hospitals (all levels of care, e.g. acute) and portions of a Hospital designated for Skilled or Rehabilitation services. Specialist(s) A Physician who provides medical care in any generally accepted medical or surgical specialty or subspecialty. Specialty Care Health care services or supplies that require the services of a specialist. Subscriber A person who meets all applicable eligibility requirements as described in this Certificate has enrolled in Aetna, and is subject to Premium requirements as set forth in the Premiums section of the Group Policy. HO SG2016COC SG Off Exchange
214 Substance Abuse Any use of alcohol and/or drugs which produces a pattern of pathological use causing impairment in social or occupational functioning or which produces physiological dependency evidenced by physical tolerance or withdrawal. Substance Abuse Rehabilitation Services, procedures and interventions to eliminate dependence on or abuse of legal and/or illegal chemical substances, according to individualized treatment plans. Surgery or Surgical Procedure The diagnosis and treatment of injury, deformity and disease by manual and instrumental means, such as cutting, abrading, suturing, destruction, ablation, removal, lasering, introduction of a catheter (e.g., heart or bladder catheterization) or scope (e.g., colonoscopy or other types of endoscopy), correction of fracture, reduction of dislocation, application of plaster casts, injection into a joint, injection of sclerosing solution, or otherwise physically changing body tissues and organs. Telemedicine A telephone or internet-based consult with a Provider that has contracted with Aetna to offer these services. Transplant Replacement of solid organs; stem cells; bone marrow or tissue. Transplant Occurrence Considered to begin at the point of authorization for evaluation for a Transplant, and end: (1) 180 days from the date of the Transplant; or (2) upon the date the Member is discharged from the Hospital or outpatient facility for the admission or visit(s) related to the Transplant, whichever is later. Urgent Care A facility licensed as a freestanding medical facility by applicable state and federal laws to treat an urgent condition. Walk-in Clinic A free-standing health care facility. Neither of the following should be considered a Walk-in Clinic: An emergency room; nor The outpatient department of a Hospital HO SG2016COC SG Off Exchange
215 All coverage other than PCP and PCP referred coverage (out-ofnetwork) coverage under the Health Network Option Open Access plan Schedule of benefits If this is an ERISA plan, Members have certain rights under this plan. If the Contract Holder is a church group or a government group this may not apply. Please contact the Contract Holder for additional information. HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
216 Schedule of Benefits This Schedule of Benefits lists the Deductibles and Copayments or Coinsurance, if any, that apply to the services Members receive under this plan. Members should review this schedule to become familiar with Deductibles and Copayments or Coinsurance and any limits that apply to the services. How to read the Schedule of Benefits Members are responsible to pay any Deductibles and Copayments or Coinsurance. Members are responsible for full payment of any health care services received that are not a Covered Benefit. This plan has limits for specific Covered Benefits. For example, these could be visit, day or dollar maximums. These may be combined maximums between or separate maximums for Participating Providers and Non-Participating Providers unless we state otherwise. Important note: All Covered Benefits are subject to the Deductible and Copayment or Coinsurance unless otherwise noted in the Schedule of Benefits below. For answers to any questions, contact Member Services by logging onto the Aetna Navigator secure member website at or at the toll-free number on the Member s ID card. The coverage described in this Schedule of Benefits will be provided under Aetna Health Insurance Company Coverage Agreement. This Schedule of Benefits replaces any Schedule of Benefits previously in effect under the Coverage Agreement. Keep this Schedule of Benefits with the Certificate. HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
217 Plan features Cost share/deductible/ Limits Out-of-network coverage Deductible Members have to meet their Deductible before this plan pays for benefits. Individual $3,000 per Calendar Year Family $6,000 per Calendar Year Deductible waiver The Deductible is waived for all of the following Eligible Health Services: Preventive care and wellness Family planning services - female contraceptives Nutritional supplements including Medical Foods to Treat Inherited Metabolic Disorders and Formulas to Treat Eosinophilic Gastrointestinal Disorders Maximum Out-of-Pocket Limit Maximum Out-of-Pocket Limit per Calendar Year Individual Family $13,700 per Calendar Year $27,400 per Calendar Year Precertification Covered Benefit reduction The Certificate contains a complete description of the Precertification program. You will find details on Precertification requirements in the Aetna Procedure section. Failure to Precertify your Eligible Health Services when required will result in the following benefits reduction: A $400 penalty will be applied separately to each type of expense. However, the penalty amount will not exceed 50% of the recognized charge for each type of expense. The additional percentage or dollar amount of the Recognized Charge which the Member may pay as a penalty for failure to obtain Precertification is not a Covered Benefit, and will not be applied to the Deductible amount or the Maximum Out-of-Pocket Limit, if any. General coverage provisions This section provides detailed explanations about the: Deductible Maximum Out-of-Pocket Limits Limits that are listed in this Schedule of Benefits. HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
218 Deductible Provisions Covered Benefits that are subject to the Deductible include Prescription Drug Covered Benefits provided under the medical plan and the Outpatient Prescription Drug plan. Covered Benefits applied to the out-of-network Deductibles will not be applied to satisfy the innetwork Deductibles. Covered Benefits applied to the in-network Deductibles will not be applied to satisfy the out-of-network Deductibles. The Deductible may not apply to certain Covered Benefits. You must pay any applicable Copayments or Coinsurance for Covered Benefits to which the Deductible does not apply. Individual This is the amount you owe for Covered Benefits each Calendar Year before the plan begins to pay for Covered Benefits. This Calendar Year Deductible applies separately to you and each Covered Dependent. After the amount you pay for Covered Benefits reaches the Calendar Year Deductible, this plan will begin to pay for Covered Benefits for the rest of the Calendar Year. Family This is the amount you owe for Covered Benefits each Calendar Year before the plan begins to pay the Covered Benefits. After the amount you pay for Covered Benefits reaches this family Calendar Year Deductible, this plan will begin to pay for Covered Benefits that the you and your Covered Dependents incur for the rest of the Calendar Year. To satisfy this family Deductible limit for the rest of the Calendar Year, the following must happen: The combined Covered Benefits that you and each Covered Dependent incur towards the individual Calendar Year Deductibles must reach this family Deductible limit in a Calendar Year. When this occurs in a Calendar Year, the individual Calendar Year Deductibles for you and your Covered Dependents will be considered to be met for the rest of the Calendar Year. Copayments Copayment As it applies to in-network coverage, this is a specified dollar amount or percentage that you must pay at the time Covered Benefits are received from a Participating Provider. As it applies to in-network coverage, if Aetna compensates Participating Providers on the basis of the reasonable amount, your cost share is based on this amount. Coinsurance The specific percentage you have to pay for a health care service listed in the Schedule of Benefits. Maximum Out-of-Pocket Limits Provisions Covered Benefits that are subject to the Maximum Out-of-Pocket Limit include Prescription Drug Covered Benefits provided under the medical plan and the Outpatient Prescription Drug plan. HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
219 Covered Benefits applied to the Out-of-Network Maximum Out-of-Pocket Limit will not be applied to satisfy the in-network Maximum Out-of-Pocket Limit and Covered Benefits applied to the in-network Maximum Out-of-Pocket Limit will not be applied to satisfy the Out-of-Network Maximum Out-of- Pocket Limit. The Maximum Out-of-Pocket Limit is the maximum amount you are responsible to pay for Copayments, Coinsurance and Deductibles for Covered Benefits during the Calendar Year. This plan has an individual and family Maximum Out-of-Pocket Limit. As to the individual Maximum Out-of- Pocket Limit, each covered person must meet their Maximum Out-of-Pocket Limit separately. Individual Once the amount of the Copayments, Coinsurance and Deductibles you or your Covered Dependents have paid for Covered Benefits during the Calendar Year meets the individual Maximum Out-of- Pocket Limit, this plan will pay 100% of the Covered Benefits that apply toward the limit for the rest of the Calendar Year for that person. Family Once the amount of the Copayments or Coinsurance and Deductibles you or your Covered Dependents have paid for Covered Benefits during the Calendar Year meets this family Maximum Out-of-Pocket Limit, this plan will pay 100% of the Covered Benefits that apply toward the limit for the remainder of the Calendar Year for all covered family members. The Maximum Out-of-Pocket Limit may not apply to certain Covered Benefits. If the Maximum Outof-Pocket Limit does not apply to a Covered Benefits, your Copayment or Coinsurance for that Covered Benefit will not count toward satisfying the Maximum Out-of-Pocket Limit amount. Certain costs that you incur do not apply toward the Maximum Out-of-Pocket Limit. These include: As it applies to Out-of-Network coverage: Charges, expenses or costs in excess of the Recognized Charge All costs for non-covered services Certain other Covered Benefits in the Schedule of Benefits Calculations; Determination of Recognized Charge; determination of Benefits Provisions Your responsibility for the costs of services will be calculated on the basis of when the service or supply is provided, not when payment is made. Benefits will be pro-rated to account for treatment or portions of stays that occur in more than one Calendar Year. Determinations regarding when benefits are covered are subject to the terms and conditions of the plan. HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
220 Eligible Health Services Out-of-network coverage* 1. Preventive care and wellness Routine physical exams- Performed at a Physician, PCP office Preventive care immunizations- Performed in a facility or at a Physician office Well woman preventive visits - routine gynecological exams (including pap smears)- Performed at a Physician, PCP, obstetrician (OB), gynecologist (GYN) or OB/GYN office Screening and counseling services - Includes obesity and/or healthy diet counseling, misuse of alcohol and/or drugs, use of tobacco products, sexually transmitted infection counseling, genetic risk counseling for breast and ovarian cancer - Office visits Tobacco Cessation Prescription and Over-the-Counter Drugs, for each thirty day supply filled at a retail pharmacy Routine cancer screenings - (applies whether performed at a Physician, PCP, specialist office or facility) Prenatal Care - (provided by an obstetrician (OB), gynecologist (GYN), and/or OB/GYN) Comprehensive lactation support and counseling services - Facility or office visits Breast feeding durable medical equipment - Breast pump supplies and accessories Family planning services Female Contraceptives Preventive care and wellness (as described above) 50% (of the Recognized Charge) per visit Preventive care and wellness benefit limitations Routine physical exams Limitations Child Subject to any age and visit limits provided for in the comprehensive guidelines supported by the American Academy of Pediatrics/Bright Futures/Health Resources and Services Administration guidelines for children and adolescents. For details, contact the Physician. Limitations Adult 1 visit HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
221 Preventive care immunizations Limitations Subject to any age limits provided for in the comprehensive guidelines supported by Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention Well woman preventive visits routine gynecological exams (including pap smears) Limitations For details, contact the Physician. Subject to any age limits provided for in the comprehensive guidelines supported by the Health Resources and Services Administration. Preventive screening and counseling services: limitations are per Calendar Year unless stated Obesity and/or healthy diet Coverage is limited to: age 0-22, unlimited visits; age 22+, 26 visits every 12 months, of which up to 10 visits may be used for healthy diet counseling. Misuse of alcohol and/or drugs Use of tobacco products Sexually transmitted infection Genetic risk counseling for breast and ovarian cancer Coverage is limited to 5 visits every 12 months Coverage is limited to 8 visits every 12 months. Coverage is limited to 2 visits every 12 months. Not subject to any age or frequency limitations Tobacco Cessation Prescription and Over-the-Counter Drugs For each 30 day supply filled at a retail pharmacy 0% per prescription or refill Maximums: Coverage is permitted for two, 90-day treatment regimens only. Any additional treatment regimens will be paid according to the tier of drug per the schedule of benefits, above. Coverage only includes generic drug when a brand-name drug is available. Coverage will be subject to any sex, age, medical condition, family history, and frequency guidelines in the recommendations of the United States Preventive Services Task Force. For details on the guidelines and the current list of covered tobacco cessation Prescription Drugs and OTC drugs, contact Member Services by logging onto the Aetna Navigator secure member website at or calling the number on the back of the Member ID card. HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
222 Routine cancer screenings Limitations: Subject to any age; family history; and frequency guidelines as set forth in the most current: Evidence-based items that have in effect a rating of A or B in the current recommendations of the United States Preventive Services Task Force; and The comprehensive guidelines supported by the Health Resources and Services Administration. Any lung cancer screenings that exceed the lung cancer screening maximum above are covered under the Outpatient diagnostic testing section. Comprehensive lactation support and counseling services Lactation counseling services visit limits per Calendar Year either in a group or individual setting Any visits that exceed the lactation counseling services limit are covered under Physician services office visits. Coverage is limited to 6 visits Breast feeding durable medical equipment Important note: Members should review the Maternity and related newborn care section. This will give more information on coverage levels for maternity care under this plan. See the Breast feeding durable medical equipment section of the Certificate for limitations on breast pump and supplies. Family planning services female contraceptives Contraceptive counseling services visit limits per Calendar Year either in a group or individual setting Coverage is limited to 2 visits Eligible Health Services Out-of-network coverage* 2. Physicians and other Health Professional care Physician services Office hours visits (non-surgical) non-preventive care 50% (of the Recognized Charge) per visit HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
223 Allergy injections Without a Physician, PCP or Specialist office visit Allergy testing and treatment Performed at a Physician, PCP or Specialist office 50% (of the Recognized Charge) per visit 50% (of the Recognized Charge) per visit Immunizations when not part of the physical exam Immunizations when not part of the physical exam Covered according to the type of benefit and the place where the service is received. Injectable medications Performed at a physician, PCP or specialist office Physician surgical services Performed at a Physician or Specialist office Alternatives to physician office visits Walk-in Clinic visits Walk-in Clinic non-emergency visit (includes coverage for immunizations.) Limitations 50% (of the Recognized Charge) per visit 50% (of the Recognized Charge) per visit 50% (of the Recognized Charge) per visit Subject to any age limits provided for in the comprehensive guidelines supported by Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention For details, contact the Physician. Individual screening and counseling services Includes obesity and/or healthy diet counseling, use of tobacco products and stress management services Individual screening and counseling services 50% (of the Recognized Charge) per visit Refer to the Preventive care and wellness section earlier in this Schedule of Benefits for maximums that may apply to these types of services. *Important note: Not all preventive care and stress management services are available at all Walk-in Clinics. The types of services offered will vary by the Provider and location of the clinic. These services may also be obtained from a Participating Physician. HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
224 E-Visits and Telemedicine consultations E-visit online consultation by a Physician, PCP Telemedicine consultation by a Physician, PCP E-visit online consultation by a Specialist Telemedicine consultation by a Specialist Specialist office visits Office hours visit (non-surgical) Not Covered Not Covered Not Covered Not Covered 50% (of the Recognized Charge) per visit Eligible Health Services 3. Hospital and other facility care Hospital care Inpatient Hospital Skilled nursing facility Inpatient facility Out-of-network coverage* 50% (of the Recognized Charge) per admission 50% (of the Recognized Charge) per admission Day limit per Calendar Year 90 Outpatient surgery Performed in Hospital outpatient department Performed in facility other than Hospital outpatient department Home health care Outpatient Hospice Inpatient facility and other Hospice benefits during a stay Hospice Outpatient 50% (of the Recognized Charge) per visit 50% (of the Recognized Charge) per visit 50% (of the Recognized Charge) per visit 50% (of the Recognized Charge) per admission 50% (of the Recognized Charge) per visit HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
225 Eligible Health Services Out-of-network coverage* 4. Emergency Care and Urgent Care A separate Hospital emergency room or Urgent Care Deductible or Copayment will apply for each visit to an emergency room or an Urgent Care Facility. Hospital emergency room $250 per visit, No deductible applies Non-emergency care in a Hospital emergency room Not Covered Important note: As Non-Participating Providers do not have a contract with Aetna the Provider may not accept payment of the Member s cost share, (Deductible, Copayment and Coinsurance), as payment in full. The Member may receive a bill for the difference between the amount billed by the Provider and the amount paid by this plan. If the Provider bills the Member for an amount above the Member s cost share, the Member is not responsible for paying that amount. The Member should send the bill to the address listed on the back of the Member ID card, and Aetna will resolve any payment dispute with the Provider over that amount. Make sure the Member's ID number is on the bill. If the Member is admitted to a Hospital as an inpatient right after a visit to an emergency room, the Member s emergency room Deductible or Copayment will be waived and the inpatient Deductible or Copayment will apply. Urgent medical care at a non-hospital free 50% (of the Recognized Charge) per visit standing facility Non-urgent use of Urgent Care Facility at a non- Hospital free standing facility Not Covered HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
226 Eligible Health Services Out-of-network coverage* 5. Specific conditions Maternity and related newborn care Inpatient and other maternity and related 50% (of the Recognized Charge) per admission newborn care services and supplies For in-network services, any Copayment that is collected applies to the delivery and postpartum care services provided by an OB's, GYN's, or OB/GYN s only. No Copayment that is collected applies to prenatal care services provided by an OB's, GYN's, or OB/GYN s. See the Prenatal care sections for cost-sharing and limits that apply to these services. Delivery services and postpartum care services Performed in a facility or at a Physician office Covered according to the type of benefit and the place where the service is received. Other prenatal care services Reconstructive breast surgery Reconstructive breast surgery Covered according to the type of benefit and the place where the service is received. Covered according to the type of benefit and the place where the service is received. Reconstructive or cosmetic services and supplies Reconstructive surgery and supplies Mental Disorders Covered according to the type of benefit and the place where the service is received. Coverage is provided under the same terms, conditions as any other illness. Inpatient facility and other inpatient services and 50% (of the Recognized Charge) per admission supplies Residential treatment Coverage is provided under the same terms, conditions as any other illness. Inpatient facility and other inpatient services and 50% (of the Recognized Charge) per visit supplies Mental Disorders Coverage is provided under the same terms, conditions as any other illness. Outpatient visits to a PCP - Physician Office visits 50% (of the Recognized Charge) per visit (non-surgical) Outpatient visits to a Specialist or Behavioral Health Provider Office visits (non-surgical) 50% (of the Recognized Charge) per visit HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
227 Partial Hospitalization Treatment (at least 4 hours, but less than 24 hours per day of clinical treatment) Intensive Outpatient Program (at least 2 hours per day and at least 6 hours per week of clinical treatment) Substance Abuse Detoxification Coverage is provided under the same terms, conditions as any other illness. Outpatient 50% (of the Recognized Charge) per visit Partial Hospitalization Treatment (at least 4 hours, but less than 24 hours per day of clinical treatment) Intensive Outpatient Program (at least 2 hours per day and at least 6 hours per week of clinical treatment) Rehabilitation Coverage is provided under the same terms, conditions as any other illness. Inpatient and other inpatient services and 50% (of the Recognized Charge) per admission supplies Residential treatment Coverage is provided under the same terms, conditions as any other illness. Inpatient facility and other inpatient services and 50% (of the Recognized Charge) per admission supplies Rehabilitation Coverage is provided under the same terms, conditions as any other illness. Outpatient visits to a PCP - Physician Office visits 50% (of the Recognized Charge) per visit (non-surgical) Outpatient visits to a Specialist or Behavioral Health Provider Office visits (non-surgical) 50% (of the Recognized Charge) per visit Partial Hospitalization Treatment (at least 4 hours, but less than 24 hours per day of clinical treatment) provided in a facility or program for treatment of Substance Abuse provided under the direction of a Physician. Intensive Outpatient Program (at least 2 hours per day and at least 6 hours per week of clinical treatment) provided in a facility or program for treatment of Substance Abuse provided under the direction of a Physician. Autism spectrum disorders, including Applied behavior analysis Outpatient visits to a PCP - Physician Office visits (non-surgical) 50% (of the Recognized Charge) per visit Outpatient visits to a Specialist or Behavioral Health Provider Office visits (non-surgical) 50% (of the Recognized Charge) per visit HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
228 Diabetes Diabetic equipment Diabetic supplies Diabetic education Treatment of basic infertility Basic infertility 50% (of the Recognized Charge) per item 50% (of the Recognized Charge) per item 50% (of the Recognized Charge) per visit Covered according to the type of benefit and the place where the service is received Eligible Health Services Transplant services facility and non-facility Inpatient and other inpatient services and supplies Network (Non-IOE facility) 50% (of the Recognized Charge) per admission Outpatient Covered according to the type of benefit and the place where the service is received. Physician services Covered according to the type of benefit and the place where the service is received. Transplant travel and lodging expenses (expenses are for transplant recipient and companion only) Maximum benefit for travel and lodging expenses for any one transplant, including tandem transplants $10,000 Eligible Health Services 6. Specific therapies and tests Diagnostic and preoperative testing Diagnostic complex imaging Complex imaging services Outpatient diagnostic lab work Lab work Out-of-network coverage* 50% (of the Recognized Charge) per visit 50% (of the Recognized Charge) per visit Outpatient diagnostic radiological services X-ray 50% (of the Recognized Charge) per visit HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
229 Outpatient preoperative testing Performed in the outpatient department of a Hospital Covered according to the type of benefit and the place where the service is received. Performed at an outpatient facility other than outpatient department of a Hospital Covered according to the type of benefit and the place where the service is received. Outpatient therapies Infusion therapy Performed in a Physician s office or in a 50% (of the Recognized Charge) per visit person s home Performed at outpatient facility 50% (of the Recognized Charge) per visit Chemotherapy Chemotherapy Radiation therapy Radiation therapy Specialty Care Prescription Drugs Performed in a Physician s office or in the home Covered according to the type of benefit and the place where the service is received. Covered according to the type of benefit and the place where the service is received. Covered according to the type of benefit and the place where the service is received. Performed at outpatient facility Short-term cardiac and pulmonary rehabilitation therapy services Cardiac and pulmonary rehabilitation Covered according to the type of benefit and the place where the service is received. Short-Term Rehabilitation Therapy Services Outpatient Cognitive Therapy, Physical Therapy Occupational Therapy and Speech Therapy Rehabilitation Benefits Outpatient physical therapy Physical therapy 50% (of the Recognized Charge) per visit Visit limit* per Calendar Year 60 *A visit is equal to no more than 1 hour of therapy. Visit limits are combined for outpatient physical therapy, outpatient occupational therapy and outpatient speech therapy. HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
230 Outpatient occupational therapy Occupational therapy 50% (of the Recognized Charge) per visit Visit limit* per Calendar Year 60 *A visit is equal to no more than 1 hour of therapy. Visit limits are combined for outpatient physical therapy, outpatient occupational therapy and outpatient speech therapy. Outpatient speech therapy Speech therapy 50% (of the Recognized Charge) per visit Visit limit* per Calendar Year 60 *A visit is equal to no more than 1 hour of therapy. Visit limits are combined for outpatient physical therapy, outpatient occupational therapy and outpatient speech therapy. Spinal manipulation Spinal manipulation 50% (of the Recognized Charge) per visit Habilitation therapy services Therapies other than physical, occupational, and speech Visit limit* per Calendar Year 60 *A visit is equal to no more than 1 hour of therapy. 50% (of the Recognized Charge) per visit Eligible Health Services 7. Other Covered Benefits Acupuncture Covered as a form of anesthesia in connection with a covered surgical procedure Ambulance service Ground Ambulance Air or water Ambulance Non-emergency Ambulance Disposable Outpatient Supplies Disposable Outpatient Supplies Out-of-network coverage* 50% (of the Recognized Charge) per visit 30% (of the Recognized Charge) per trip 30% (of the Recognized Charge) per trip 50% (of the Recognized Charge) per trip 50% (of the Recognized Charge) per item HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
231 Durable Medical Equipment (DME) DME 50% (of the Recognized Charge) per item Family planning services - other Inpatient services Voluntary sterilization for males 50% (of the Recognized Charge) per visit Voluntary termination of pregnancy 50% (of the Recognized Charge) per visit Outpatient services Voluntary sterilization for males 50% (of the Recognized Charge) per visit Voluntary termination of pregnancy 50% (of the Recognized Charge) per visit Hearing aids Hearing aid exams 50% (of the Recognized Charge) per visit Hearing aids Jaw Joint Disorder Jaw Joint Disorder treatment 50% (of the Recognized Charge) per visit 50% (of the Recognized Charge) per visit Bariatric Surgery Bariatric Surgery Includes Surgical Procedure and Acute Hospital Services -Facility Services 50% (of the Recognized Charge) per admission Nutritional supplements Medical foods to treat Inherited Metabolic Disorders Nutritional supplements 25% (of the Recognized Charge) per item/prescription No Deductible applies Formulas to treat Eosinophilic Gastrointestinal Disorders 25% (of the Recognized Charge) per item/prescription No Deductible applies Prosthetic devices Prosthetic devices 50% (of the Recognized Charge) per item HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
232 Eligible Health Services Out-of-network coverage* Vision care Pediatric vision care Coverage is limited to covered persons through the end of the month in which the person turns 19 Routine vision exams (including refraction) Performed by an ophthalmologist or optometrist 50% (of the Recognized Charge) per visit Visit limit per Calendar Year 1 visit Vision care services and supplies Preferred eyeglass frames, Prescription lenses or Prescription contact lenses. Non-preferred eyeglass frames, Prescription lenses or Prescription contact lenses. Number of eyeglass frames per Calendar Year 50% (of the Recognized Charge) per visit 50% (of the Recognized Charge) per visit One set of eyeglass frames Number of Prescription lenses per Calendar Year Number of Prescription contact lenses per Calendar Year (includes non-conventional Prescription contact lenses and aphakic lenses prescribed after cataract surgery) One pair of Prescription lenses Daily disposables: up to 3 month supply Extended wear disposable: up to 6 month supply Non-disposable lenses: one set Adult vision care Limited to covered person age 19 and over Routine vision exams (including refraction) Performed by an ophthalmologist or optometrist 50% (of the Recognized Charge) per visit Visit limit per Calendar Year 1 visit *Important note: Refer to the Vision care section in the Certificate for the explanation of these vision care supplies. As to coverage for Prescription lenses in a Contract Year, this benefit will cover either Prescription lenses for eyeglass frames or Prescription contact lenses, but not both. Coverage does not include the office visit for the fitting of Prescription contact lenses. HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
233 Pediatric dental Coverage is limited to covered persons through the end of the month in which the person turns 19 Type A services 30% after Deductible Type B services Type C services Orthodontic services 50% after Deductible 50% after Deductible 50% after Deductible Dental emergency limit: $75 The dental emergency limit is the most the plan will pay for health care services incurred by a Member for any one dental emergency. Dental benefits are subject to the medical plan s Deductibles and Maximum Out-of-Pocket Limits as explained on the Schedule of Benefits. Type A Services: Diagnostic and Preventive Care Visits and images (D0120) Office visit during regular office hours, for oral examination (limited to: 2 visits every 12 months) (D0160) Routine comprehensive or recall examination (limited to: 2 visits every 12 months) (D0150, D0180) Comprehensive periodontal evaluation (limited to: 2 visits every 12 months) (D0140) Problem-focused examination (limited to: 2 visits every 12 months) (D1110, D1120) Prophylaxis (cleaning) (limited to: 2 treatments per year) (D1208) Topical application of fluoride (limited to: 2 courses every 12 months) (D1206) Topical fluoride varnish (limited to: 2 courses every 12 months) (D1351) Sealants, per tooth (limited to: one application every 3 years for permanent molars) (D1352) Preventive resin restoration in a moderate to high caries risk patient-permanent tooth (limited to: one application every 3 years for permanent molars) (D0270-D0274) Bitewing images (limited to: 2 sets per 12 months) (D0210) Complete image series, including bitewings (limited to: 1 set every 3 years) (D0330) Panoramic images (limited to: 1 set every 3 years) (D0340) Cephalometric image (D0350) Oral facial photographic images (D0470) Diagnostic models (D0277) Vertical bitewing images (limited to: 2 sets per year) (D0220, D0230) Periapical images (D0240) Intra-oral, occlusal view, maxillary or mandibular (D9110) Emergency palliative treatment per visit Note: Diagnostic procedures of: D0330, D0340, D0350 and D0470 are covered as Type A benefit for a non-vested orthodontia patient. HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
234 Space maintainers (Includes all adjustments within 6 months after installation) (D1510, D1515) Fixed (unilateral or bilateral) (D1520, D1525) Removable (unilateral or bilateral) (D1550) Re-cementation of space maintainer (D1555) Removal of space maintainer Type B Services: Basic Restorative Care Visits and images (D9440) Professional visit after hours (payment will be made on the basis of services rendered the charge for the after-hours visit, whichever is greater) (D9310) Consultation (by other than the treating provider) (D9930) Treatment of complications (post-surgical) unusual circumstances, by report Images and pathology (D0250-D0260) Upper or lower jaw, extra-oral (D9610) Therapeutic drug injection, by report Oral surgery (D7111) Extraction, coronal remnants-deciduous tooth (D7140) Extraction, erupted tooth or exposed root (elevation and/or forceps removal) (D7210) Surgical removal of erupted tooth requiring removal of bone and/or resectioning of tooth (D7251) Coronal remnants (D7250) Surgical removal of erupted tooth/root tip Surgical removal of impacted teeth (D7220) Removal of impacted tooth (soft tissue) (D7230) Removal of impacted tooth (partially bony) (D7240) Removal of impacted tooth (completely bony) (D7241) Removal of impacted tooth (completely bony with unusual surgical complications) (D7510) Incision and drainage of abscess (D7450, D7451) Removal of odontogenic cyst or tumor (D7280) Other surgical procedures (D7310) Alveoplasty, in conjunction with extractions - per quadrant (D7311) Alveoplasty, in conjunction with extractions, 1 to 3 teeth or tooth spaces - per quadrant (D7320) Alveoplasty, not in conjunction with extraction - per quadrant (D7321) Alveoplasty, not in conjunction with extractions, 1 to 3 teeth or tooth spaces - per quadrant (D7980) Sialolithotomy: removal of salivary calculus (D7983) Closure of salivary fistula (D7970) Excision of hyperplastic tissue (D7471) Removal of exostosis (D7270) Tooth re-implantation (D7272) Transplantation of tooth or tooth bud (D7260) Closure of oral fistula of maxillary sinus (D7550) Sequestrectomy (D7283) Crown exposure to aid eruption (D7530) Removal of foreign body from soft tissue (D7960) Frenectomy HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
235 (D7910) Suture of soft tissue injury (D7971) Excision of pericornal gingiva Periodontics (D9951, D9952) Occlusal adjustment (other than with an appliance or by restoration) (D4341) Periodontal scaling and root planing, per quadrant (limited to 4 separate quadrants every 2 years) (D4342) Root planing and scaling 1 to 3 teeth per quadrant (limited to once per site every 2 years) (D4910) Periodontal maintenance procedures following active therapy (limited to: 4 in 12 months) (combined with prophylaxis after completion of active periodontal therapy) (D4381) Localized delivery of antimicrobial agents Endodontics (D3110-D3120) Pulp capping (D3220-D3222) Pulpotomy (D3230-D3240) Pulpal therapy (D3355-D3357) Pulpal regeneration Restorative dentistry Excludes inlays, crowns (other than prefabricated stainless steel or resin) and bridges. Multiple restorations in 1 surface will be considered as a single restoration. (D2140, D2150, D2160, D2161) Amalgam restorations - one, two three, four or more surfaces, primary or permanent teeth (D2330, D2331, D2332, D2335) Resin-based composite one, two three, four or more surfaces, anterior (D2390) Resin-based composite crown, anterior (D2391, D2392, D2393, D2394) Resin-based composite - one, two, three, four or more surfaces, posterior Pins (D2951) Pin retention per tooth, in addition to amalgam or resin restoration Crowns (when tooth cannot be restored with a filling material) (D2930-D2931) Prefabricated stainless steel (D2932) Prefabricated resin crown (excluding temporary crowns) (D2940) Protective resin Re-cementation (D2910) Inlay (D2920) Crown (D6930) Bridge Prosthodontics Dentures and partials (D5730, D5731) Office reline, complete denture - maxillary or mandibular (D5740, D5741) Office reline, partial denture - maxillary or mandibular (D5750, D5751) Reline, complete denture - maxillary or mandibular - laboratory HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
236 (D5760, D5761) Reline, partial denture - maxillary or mandibular - laboratory (D5850, D5851) Special tissue conditioning, per denture - maxillary or mandibular (D5710, D5711) Rebase complete denture - maxillary or mandibular (D5720, D5721) Rebase partial denture - maxillary or mandibular (D5410, D5411) Adjustment to complete denture (more than 6 months after installation) - maxillary or mandibular (D5421, D5422) Adjustment to partial denture (more than 6 months after installation) - maxillary or mandibular Repairs: Dentures and partial dentures D6980) Fixed partial denture repair, by report (D5510) Repair broken complete denture base (D5520) Replace missing or broken teeth complete denture (each tooth) (D5610) Repair resin denture base (D5620) Repair cast framework (D5630) Broken denture clasp, no teeth involved (D5640) Replacing missing or broken teeth, each tooth Adding teeth to existing partial denture (D5650) Each tooth (D5660) Each clasp General anesthesia and intravenous sedation Only when medically necessary and only when provided in conjunction with a covered dental surgical procedure (D9220) Deep sedation/general anesthesia first 30 minutes (D9221) Deep sedation/general anesthesia each additional 15 minutes (D9241) Intravenous conscious sedation first 301 minutes (D9242) Intravenous conscious sedation each additional 15 minutes Type C Services: Major Restorative Care Periodontics (D4261) Osseous surgery, including flap and closure, 1 to 3 teeth per quadrant (limited to 1 per site every 3 years) (D4260) Osseous surgery, including flap and closure, (limited to 1 per quadrant every 3 years) (D4270) Pedicle soft tissue graft procedure (D4277, D4278) Free soft tissue graft procedures (D4273) Subepithelial connective tissue graft procedure (including donor site surgery) (D4210) Gingivectomy, per quadrant (limited to 1 per quadrant every 3 years) (D4211) Gingivectomy, 1 to 3 teeth per quadrant (D4240) Gingival flap procedure - per quadrant (limited to 1 per quadrant every 3 years) (D4241) Gingival flap procedure 1 to 3 teeth per quadrant (limited to 1 per site every 3 years) (D4249) Clinical crown lengthening (D4355) Full mouth debridement (limited to 1 treatment per lifetime) Endodontics (D3351, D3352, D3353) Apexification/recalcification (D3410, D3421, D3425, D3426) Apicoectomy/periradicular surgery anterior/bicuspid/molar/each additional root HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
237 (D3354) Pulpal regeneration Root canal therapy including medically necessary images: (D3310) Anterior (D3320) Bicuspid (D3330) Molar Retreatment of previous root canal therapy including medically necessary images: (D3346) Anterior (D3347) Bicuspid (D3348) Molar (D3450) Root amputation (D3920) Hemisection (including any root removal) Restorative Inlays, onlays, labial veneers and crowns when provided as treatment for decay or acute traumatic injury and only when teeth cannot be restored with a filling material or when the tooth is an abutment to a fixed bridge (limited to: 1 per tooth every 5 years) Inlays/Onlays (limited to: 1 tooth every 5 years) (D2510, D2520, D2530) Inlay metallic, one, two, three surfaces (D2542, D2543, D2544) Onlay metallic, one, two, three and four or more surfaces (D2610, D2620, D2630) Inlay porcelain/ceramic, one, two, three or more surfaces (D2642, D2643, D2644) Onlay porcelain/ceramic, two, three and four or more surfaces (D2650, D2651, D2652) Inlay resin based composite, one, two, three or more surfaces (D2662, D2663, D2664) Onlay resin based composite, two, three and four or more surfaces Crowns (limited to: 1 tooth every 5 years) (D2710) Resin-based composite (D2712) 3/4 resin based composite (D2720) Resin with high noble metal (D2721) Resin with base metal (D2722) Resin with noble metal (D2740) Porcelain/ceramic substrate (D2750) Porcelain fused to noble metal (D2751) Porcelain fused to predominately base metal (limited to: 1 tooth every 5 years) (D2752) Porcelain fused to noble metal (D2790) Full cast high noble metal (D2791) Base metal (full cast) (D2792) Noble metal (full cast) (D2780) 3/4 cast high noble metal (D2781) 3/4 cast base metal (D2782) 3/4 cast noble metal (D2783) 3/4 porcelain/ceramic (D2794) Titanium (D2950) Core build-up, including any pins (D2952,D2953) Post and core in addition to crown, indirectly fabricated (D2954) Prefabricated post and core, in addition to crown (D2980) Crown repair HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
238 Prosthodontics Installation of dentures and bridges is covered only if needed to replace teeth which were not abutments to a denture or bridge/partial denture less than 5 years old. Replacement of existing bridges/partial denture or dentures (limited to: 1 every 5 years) Bridge/partial denture abutments (See Inlays/Onlays and Crowns) (limited to: 1 tooth every 5 years) Pontics (limited to: 1 tooth every 5 years) (D6210) Cast high noble metal (D6211) Cast base metal (D6212) Cast noble metal (D6214) Titanium (D6240) Porcelain fused to high noble metal (D6241) Porcelain fused to base metal (D6242) Porcelain fused to noble metal (D6245) Porcelain/ceramic (D6250) Resin with high noble (D6251) Resin with base metal (D6252) Resin with noble metal (D6545) Retainer cast metal for resin bonded fixed prosthesis (limited to: 1 tooth every 5 years) (D6548) Retainer porcelain/ceramic for resin bonded fixed prosthesis (limited to: 1 tooth every 5 years) Fixed partial denture retainers-crowns (limited to: 1 tooth every 5 years) (D6740) Porcelain/ceramic (D6750) Porcelain fused to high noble metal (D6751) Porcelain fused to base metal (D6752) Porcelain fused to noble metal (D6780) 3/4 cast high noble metal (D6781) 3/4 cast base metal (D6782) 3/4 cast noble metal (D6783) 3/4 porcelain/ceramic (D6790) Full cast high noble metal (D6791) Full cast base metal (D6792) Full cast noble metal (D6794 Titanium (D5281) Removable partial denture (unilateral) (limited to: 1 every 5 years) One piece casting, chrome cobalt alloy clasp attachment (all types) per unit, including pontics (limited to: 1 every 5 years) Dentures and Partials (limited to: 1 every 5 years) Fees for dentures and partial dentures include relines, rebases and adjustments within 6 months after installation. Fees for relines and rebases include adjustments within 6 months after installation. Specialized techniques and characterizations are not eligible) (D5110) Complete upper denture (D5120) Complete lower denture (D5130) Immediate upper denture (D5140) Immediate lower denture (D5211, D5212) Partial upper or lower, resin base (including any conventional clasps, rests and HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
239 teeth) (D5213, D5214) Partial upper or lower, cast metal base with resin saddles (including any conventional clasps, rests and teeth) Implants and implant services (Only if determined as a dental necessity and limited to 1 every 5 years) (D6010) Endosteal Implant (D6012) Surgical placement of interim implant body (D6040) Eposteal implant (D6050) Transosteal implant, including hardware (D6053) Implant supported complete denture (D6054) Implant supported partial denture (D6055) Connecting bar implant or abutment supported (D6056) Prefabricated abutment (D6058) Abutment supported porcelain ceramic crown (D6059) Abutment supported porcelain fused to high noble metal (D6060) Abutment supported porcelain fused to predominately base metal crown (D6061) Abutment supported porcelain fused to noble metal crown (D6062) Abutment supported cast high noble metal crown (D6063) Abutment supported cast predominately base metal crown (D6064) Abutment supported cast noble metal crown (D6065) Implant supported porcelain/ceramic crown (D6066) Implant supported porcelain fused to high noble metal (D6067) Implant supported metal crown (D6068) Abutment supported retainer for porcelain/ceramic fixed partial denture (D6069) Abutment supported retainer for porcelain fused to high noble metal fixed partial denture (D6070) Abutment supported retainer for porcelain fused to predominately base metal fixed partial denture (D6071) Abutment supported retainer for porcelain fused to noble metal fixed partial denture (D6072) Abutment supported retainer for cast high noble metal fixed partial denture (D6073) Abutment supported retainer for predominately base metal fixed partial denture (D6074) Abutment supported retainer for cast noble metal fixed partial denture (D6075) Implant supported retainer for ceramic fixed partial denture (D6076) Implant supported retainer for porcelain fused to high noble metal fixed partial denture (D6077) Implant supported retainer for cast metal fixed partial denture (D6078, D6079) Implant supported complete denture, partial denture (limited to 1 every 5 years) (D6080) Implant maintenance procedures (limited to 1 every 5 years) (D6090) Repair implant prosthesis (D6091) Replacement of semi-precious or precision attachment (D6094) Abutment supported crown titanium (D6095) Repair implant abutment (D6100) Implant removal, by report (D6110, D6111) Implant/abutment supported removable denture, maxillary or mandibular (D6112, D6113) Implant/abutment supported removable denture for partially edentulous arch, maxillary or mandibular HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
240 (D6114, D6115) Implant/abutment supported fixed denture for completely edentulous arch maxillary or mandibular (D6116, D6117) Implant/abutment supported fixed denture for partially edentulous arch maxillary or mandibular (D6100) Implant removal, by report (D6190) Implant index (D6194) Abutment supported retainer crown for fixed partial denture titanium Other services (D6940) Stress breakers (D6985) Interim partial denture (stayplate), anterior only (D9940) Occlusal guard, by report (limited to 1 in 12 months) (D8210) Removable appliance therapy (D8220) Fixed appliance therapy Orthodontic services Medically necessary comprehensive treatment (D8010) Limited orthodontic treatment of the primary dentition (D8020) Limited orthodontic treatment of the transitional dentition (D8030) Limited orthodontic treatment of the adolescent dentition (D8040) Limited orthodontic treatment of the adult dentition (D8050) Interceptive orthodontic treatment of the primary dentition (D8060) Interceptive orthodontic treatment of the transitional dentition (D8070) Comprehensive orthodontic treatment of the transitional dentition (D8080) Comprehensive orthodontic treatment of the adolescent dentition (D8090) Comprehensive treatment of adult dentition (D8660) Pre-orthodontic treatment examination to monitor growth and development (D8670) Periodic orthodontic treatment visit (as part of contract) (D8680) Orthodontic retention (removal of appliances, construction and placement of retainer(s) (D8691) Repair of orthodontic appliance (D8693) Rebonding or recementing; and/or repair, as required of fixed retainers (D8694) Repair of fixed retainers Orthodontic treatment (includes removal of appliance, construction and placement of retainer) Replacement of retainer (limited to: 1 per lifetime) Note: Benefits for codes D0330, D0340, D0350, and D0470 will be considered orthodontia when performed as part of orthodontic treatment. HO SG-OFF2016-SB AZ SG-off HO AZ Silver HNOPtion / R
Aetna Life Insurance Company
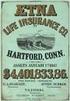 Aetna Life Insurance Company Hartford, Connecticut 06156 Amendment Policyholder: Group Policy No.: Effective Date: UNIVERSITY OF PENNSYLVANIA POSTDOCTORAL INSURANCE PLAN GP-861472 This Amendment is effective
Aetna Life Insurance Company Hartford, Connecticut 06156 Amendment Policyholder: Group Policy No.: Effective Date: UNIVERSITY OF PENNSYLVANIA POSTDOCTORAL INSURANCE PLAN GP-861472 This Amendment is effective
AETNA HEALTH INC. (GEORGIA) CERTIFICATE OF COVERAGE
 AETNA HEALTH INC. (GEORGIA) CERTIFICATE OF COVERAGE Plan Name: Silver HNOption 5200 100/50 O0140010116071 This Certificate of Coverage ("Certificate") is part of the Group Agreement ("Group Agreement")
AETNA HEALTH INC. (GEORGIA) CERTIFICATE OF COVERAGE Plan Name: Silver HNOption 5200 100/50 O0140010116071 This Certificate of Coverage ("Certificate") is part of the Group Agreement ("Group Agreement")
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Adobe Systems Incorporated. Aetna HealthFund HRA Plan
 Adobe Systems Incorporated Aetna HealthFund HRA Plan BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group
Adobe Systems Incorporated Aetna HealthFund HRA Plan BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Adobe Systems Incorporated. Aetna Choice POS II
 Adobe Systems Incorporated Aetna Choice POS II BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group Welfare
Adobe Systems Incorporated Aetna Choice POS II BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group Welfare
What Your Plan Covers and How Benefits are Paid BENEFIT PLAN. Prepared Exclusively for Leidos, Inc. Aetna Choice POS II (HDHP) - Advantage Plan
 BENEFIT PLAN Prepared Exclusively for Leidos, Inc. What Your Plan Covers and How Benefits are Paid Aetna Choice POS II (HDHP) - Advantage Plan Table of Contents Schedule of Benefits...1 Preface...18 Coverage
BENEFIT PLAN Prepared Exclusively for Leidos, Inc. What Your Plan Covers and How Benefits are Paid Aetna Choice POS II (HDHP) - Advantage Plan Table of Contents Schedule of Benefits...1 Preface...18 Coverage
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Prepared Exclusively for Cerner Corporation (Expatriate Employees)
 BENEFIT PLAN Prepared Exclusively for Cerner Corporation (Expatriate Employees) What Your Plan Covers and How Benefits are Paid PPO Medical, PPO Dental, Basic Vision and Pharmacy Aetna Life and Casualty
BENEFIT PLAN Prepared Exclusively for Cerner Corporation (Expatriate Employees) What Your Plan Covers and How Benefits are Paid PPO Medical, PPO Dental, Basic Vision and Pharmacy Aetna Life and Casualty
FEATURES NETWORK OUT-OF-NETWORK
 Schedule of Benefits Employer: The Vanguard Group, Inc. ASA: 697478-A Issue Date: January 1, 2014 Effective Date: January 1, 2014 Schedule: 3B Booklet Base: 3 For: Choice POS II - 950 Option - Retirees
Schedule of Benefits Employer: The Vanguard Group, Inc. ASA: 697478-A Issue Date: January 1, 2014 Effective Date: January 1, 2014 Schedule: 3B Booklet Base: 3 For: Choice POS II - 950 Option - Retirees
PLAN DESIGN AND BENEFITS Georgia 2-100 HNOption 13-1000-80
 Georgia Health Network Option (POS Open Access) PLAN DESIGN AND BENEFITS Georgia 2-100 HNOption 13-1000-80 PLAN FEATURES PARTICIPATING PROVIDERS NON-PARTICIPATING PROVIDERS Deductible (per calendar year)
Georgia Health Network Option (POS Open Access) PLAN DESIGN AND BENEFITS Georgia 2-100 HNOption 13-1000-80 PLAN FEATURES PARTICIPATING PROVIDERS NON-PARTICIPATING PROVIDERS Deductible (per calendar year)
What Your Plan Covers and How Benefits are Paid BENEFIT PLAN. Prepared Exclusively for The McClatchy Company. Aetna Choice Plan
 BENEFIT PLAN Prepared Exclusively for The McClatchy Company What Your Plan Covers and How Benefits are Paid Aetna Choice Plan Table of Contents Preface...1 Important Information Regarding Availability
BENEFIT PLAN Prepared Exclusively for The McClatchy Company What Your Plan Covers and How Benefits are Paid Aetna Choice Plan Table of Contents Preface...1 Important Information Regarding Availability
IN-NETWORK MEMBER PAYS. Out-of-Pocket Maximum (Includes a combination of deductible, copayments and coinsurance for health and pharmacy services)
 HMO-OA-CNT-30-45-500-500D-13 HMO Open Access Contract Year Plan Benefit Summary This is a brief summary of benefits. Refer to your Membership Agreement for complete details on benefits, conditions, limitations
HMO-OA-CNT-30-45-500-500D-13 HMO Open Access Contract Year Plan Benefit Summary This is a brief summary of benefits. Refer to your Membership Agreement for complete details on benefits, conditions, limitations
PLAN DESIGN AND BENEFITS POS Open Access Plan 1944
 PLAN FEATURES PARTICIPATING Deductible (per calendar year) $3,000 Individual $9,000 Family $4,000 Individual $12,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being
PLAN FEATURES PARTICIPATING Deductible (per calendar year) $3,000 Individual $9,000 Family $4,000 Individual $12,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being
Preventive Care Coverage Wondering what preventive care your plan covers?
 STAYING WELL Regence BlueCross BlueShield of Oregon is an Independent Licensee of the Blue Cross and Blue Shield Association Preventive Care Coverage Wondering what preventive care your plan covers? Our
STAYING WELL Regence BlueCross BlueShield of Oregon is an Independent Licensee of the Blue Cross and Blue Shield Association Preventive Care Coverage Wondering what preventive care your plan covers? Our
California PCP Selected* Not Applicable
 PLAN FEATURES Deductible (per calendar ) Member Coinsurance * Not Applicable ** Not Applicable Copay Maximum (per calendar ) $3,000 per Individual $6,000 per Family All member copays accumulate toward
PLAN FEATURES Deductible (per calendar ) Member Coinsurance * Not Applicable ** Not Applicable Copay Maximum (per calendar ) $3,000 per Individual $6,000 per Family All member copays accumulate toward
California Small Group MC Aetna Life Insurance Company
 PLAN FEATURES Deductible (per calendar year) $1,000 per member $1,000 per member Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered expenses accumulate
PLAN FEATURES Deductible (per calendar year) $1,000 per member $1,000 per member Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered expenses accumulate
Coverage for preventive care
 Coverage for preventive care Understanding your preventive care coverage Preventive care, like screenings and immunizations, helps you and your family stay healthier and can help lower your overall out-of-pocket
Coverage for preventive care Understanding your preventive care coverage Preventive care, like screenings and immunizations, helps you and your family stay healthier and can help lower your overall out-of-pocket
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Appendix A. Prepared Exclusively for The Dow Chemical Company
 Appendix A BENEFIT PLAN Prepared Exclusively for The Dow Chemical Company What Your Plan Covers and How Benefits are Paid Choice POS II (MAP Plus Option 2 - High Deductible Health Plan (HDHP) with Prescription
Appendix A BENEFIT PLAN Prepared Exclusively for The Dow Chemical Company What Your Plan Covers and How Benefits are Paid Choice POS II (MAP Plus Option 2 - High Deductible Health Plan (HDHP) with Prescription
PREFERRED CARE. All covered expenses, including prescription drugs, accumulate toward both the preferred and non-preferred Payment Limit.
 PLAN FEATURES Deductible (per plan year) $300 Individual $300 Individual None Family None Family All covered expenses, excluding prescription drugs, accumulate toward both the preferred and non-preferred
PLAN FEATURES Deductible (per plan year) $300 Individual $300 Individual None Family None Family All covered expenses, excluding prescription drugs, accumulate toward both the preferred and non-preferred
PLAN DESIGN AND BENEFITS Basic HMO Copay Plan 1-10
 PLAN FEATURES Deductible (per calendar year) Member Coinsurance Not Applicable Not Applicable Out-of-Pocket Maximum $5,000 Individual (per calendar year) $10,000 Family Once the Family Out-of-Pocket Maximum
PLAN FEATURES Deductible (per calendar year) Member Coinsurance Not Applicable Not Applicable Out-of-Pocket Maximum $5,000 Individual (per calendar year) $10,000 Family Once the Family Out-of-Pocket Maximum
New York Small Group Indemnity Aetna Life Insurance Company Plan Effective Date: 10/01/2010. PLAN DESIGN AND BENEFITS - NY Indemnity 1-10/10*
 PLAN FEATURES Deductible (per calendar year) $2,500 Individual $7,500 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services,
PLAN FEATURES Deductible (per calendar year) $2,500 Individual $7,500 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services,
PARTICIPATING PROVIDERS / REFERRED Deductible (per calendar year)
 Your HMO Plan Primary Care Physician - You choose a Primary Care Physician. The Aetna HMO Deductible provider network gives you access to a wide selection of Primary Care Physicians ( PCP's) and Specialists
Your HMO Plan Primary Care Physician - You choose a Primary Care Physician. The Aetna HMO Deductible provider network gives you access to a wide selection of Primary Care Physicians ( PCP's) and Specialists
Prevents future health problems. You receive these services without having any specific symptoms.
 Preventive Care To help you live the healthiest life possible, we offer free preventive services for most Network Health members. Please refer to your member materials, which you received when you enrolled
Preventive Care To help you live the healthiest life possible, we offer free preventive services for most Network Health members. Please refer to your member materials, which you received when you enrolled
SMALL GROUP PLAN DESIGN AND BENEFITS OPEN CHOICE OUT-OF-STATE PPO PLAN - $1,000
 PLAN FEATURES PREFERRED CARE NON-PREFERRED CARE Deductible (per calendar year; applies to all covered services) $1,000 Individual $3,000 Family $2,000 Individual $6,000 Family Plan Coinsurance ** 80% 60%
PLAN FEATURES PREFERRED CARE NON-PREFERRED CARE Deductible (per calendar year; applies to all covered services) $1,000 Individual $3,000 Family $2,000 Individual $6,000 Family Plan Coinsurance ** 80% 60%
Health Care Reform: Using preventive care for a healthier life
 HorizonBlue.com Health Care Reform: Using preventive care for a healthier life Horizon Blue Cross Blue Shield of New Jersey is committed to empowering our members with access to preventive services to
HorizonBlue.com Health Care Reform: Using preventive care for a healthier life Horizon Blue Cross Blue Shield of New Jersey is committed to empowering our members with access to preventive services to
IS HERE OPEN ENROLLMENT EMPLOYEE BENEFITS TIME TO MAKE YOUR BENEFIT CHOICES. BAYADA Home Health Care Employee Benefits
 2015 OPEN ENROLLMENT IS HERE EMPLOYEE BENEFITS TIME TO MAKE YOUR BENEFIT CHOICES BAYADA Home Health Care values the contributions of our employees. In appreciation of your dedicated service, BAYADA Home
2015 OPEN ENROLLMENT IS HERE EMPLOYEE BENEFITS TIME TO MAKE YOUR BENEFIT CHOICES BAYADA Home Health Care values the contributions of our employees. In appreciation of your dedicated service, BAYADA Home
PLAN DESIGN AND BENEFITS - Tx OAMC Basic 2500-10 PREFERRED CARE
 PLAN FEATURES Deductible (per calendar year) $2,500 Individual $4,000 Individual $7,500 Family $12,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
PLAN FEATURES Deductible (per calendar year) $2,500 Individual $4,000 Individual $7,500 Family $12,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
PLAN DESIGN AND BENEFITS - Tx OAMC 2500 08 PREFERRED CARE
 PLAN FEATURES Deductible (per calendar year) $2,500 Individual $5,000 Individual $7,500 3 Individuals per $15,000 3 Individuals per Unless otherwise indicated, the Deductible must be met prior to benefits
PLAN FEATURES Deductible (per calendar year) $2,500 Individual $5,000 Individual $7,500 3 Individuals per $15,000 3 Individuals per Unless otherwise indicated, the Deductible must be met prior to benefits
$25 copay. One routine GYN visit and pap smear per 365 days. Direct access to participating providers.
 HMO-1 Primary Care Physician Visits Office Hours After-Hours/Home Specialty Care Office Visits Diagnostic OP Lab/X Ray Testing (at facility) with PCP referral. Diagnostic OP Lab/X Ray Testing (at specialist)
HMO-1 Primary Care Physician Visits Office Hours After-Hours/Home Specialty Care Office Visits Diagnostic OP Lab/X Ray Testing (at facility) with PCP referral. Diagnostic OP Lab/X Ray Testing (at specialist)
Benefits at a Glance: Visa Inc. Policy Number: 00784A
 Benefits at a Glance: Visa Inc. Policy Number: 00784A Visa Inc. Benefits at a Glance Policy #00784A Effective Date: January 1, 2016 Visa Inc. offers Medical, Pharmacy, Vision, Dental and Medical Evacuation
Benefits at a Glance: Visa Inc. Policy Number: 00784A Visa Inc. Benefits at a Glance Policy #00784A Effective Date: January 1, 2016 Visa Inc. offers Medical, Pharmacy, Vision, Dental and Medical Evacuation
Health care reform update
 Preventive services coverage Kaiser Foundation Health Plan of the Northwest has always offered broad, affordable coverage options that encourage members to seek care before a health condition becomes serious.
Preventive services coverage Kaiser Foundation Health Plan of the Northwest has always offered broad, affordable coverage options that encourage members to seek care before a health condition becomes serious.
PLAN DESIGN & BENEFITS - CONCENTRIC MODEL
 PLAN FEATURES Deductible (per calendar year) Rice University None Family Member Coinsurance Applies to all expenses unless otherwise stated. Payment Limit (per calendar year) $1,500 Individual $3,000 Family
PLAN FEATURES Deductible (per calendar year) Rice University None Family Member Coinsurance Applies to all expenses unless otherwise stated. Payment Limit (per calendar year) $1,500 Individual $3,000 Family
What Your Plan Covers and How Benefits are Paid BENEFIT PLAN. Prepared Exclusively for Vanderbilt University. Aetna Choice POS II Health Fund Plan
 BENEFIT PLAN Prepared Exclusively for Vanderbilt University What Your Plan Covers and How Benefits are Paid Aetna Choice POS II Health Fund Plan Table of Contents Schedule of Benefits... Issued with Your
BENEFIT PLAN Prepared Exclusively for Vanderbilt University What Your Plan Covers and How Benefits are Paid Aetna Choice POS II Health Fund Plan Table of Contents Schedule of Benefits... Issued with Your
PLAN DESIGN AND BENEFITS - Tx OAMC 1500-10 PREFERRED CARE
 PLAN FEATURES Deductible (per calendar year) $1,500 Individual $3,000 Individual $4,500 Family $9,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
PLAN FEATURES Deductible (per calendar year) $1,500 Individual $3,000 Individual $4,500 Family $9,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
$20 office visit copay; deductible 20%; after deductible. $30 office visit copay; deductible Not Covered. $30 office visit copay; deductible waived
 PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $300 Individual $600 Individual $600 Family $1,200 Family All covered expenses, accumulate separately toward the preferred or non-preferred
PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $300 Individual $600 Individual $600 Family $1,200 Family All covered expenses, accumulate separately toward the preferred or non-preferred
Carnegie Mellon University Policy #02424 Benefits at a Glance Effective Date: January 1, 2014
 Carnegie Mellon University is offering Medical, Dental, Vision, Pharmacy, Medical Evacuation and Repatriation benefits through Cigna Global Health Benefits to our employees. This comprehensive international
Carnegie Mellon University is offering Medical, Dental, Vision, Pharmacy, Medical Evacuation and Repatriation benefits through Cigna Global Health Benefits to our employees. This comprehensive international
$100 Individual. Deductible
 PLAN FEATURES Deductible $100 Individual (per calendar year) $200 Family Unless otherwise indicated, the deductible must be met prior to benefits being payable. Member cost sharing for certain services,
PLAN FEATURES Deductible $100 Individual (per calendar year) $200 Family Unless otherwise indicated, the deductible must be met prior to benefits being payable. Member cost sharing for certain services,
Procedure Code(s): n/a This counseling service is included in a preventive care wellness examination or focused E&M visit.
 Coding Summary for Providers NOTE THE FOLLOWING: The purpose of this document is to provide a quick reference of the applicable codes for UnitedHealthcare plans that cover preventive care services in accordance
Coding Summary for Providers NOTE THE FOLLOWING: The purpose of this document is to provide a quick reference of the applicable codes for UnitedHealthcare plans that cover preventive care services in accordance
Unlimited except where otherwise indicated.
 PLAN FEATURES Deductible (per calendar year) $1,250 Individual $5,000 Individual $2,500 Family $10,000 Family All covered expenses including prescription drugs accumulate separately toward both the preferred
PLAN FEATURES Deductible (per calendar year) $1,250 Individual $5,000 Individual $2,500 Family $10,000 Family All covered expenses including prescription drugs accumulate separately toward both the preferred
1 exam every 12 months for members age 22 to age 65; 1 exam every 12 months for adults age 65 and older. Routine Well Child
 PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $1,000 Individual $1,000 Individual $2,000 Family $2,000 Family All covered expenses accumulate separately toward the preferred or
PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $1,000 Individual $1,000 Individual $2,000 Family $2,000 Family All covered expenses accumulate separately toward the preferred or
Medical Plan - Healthfund
 18 Medical Plan - Healthfund Oklahoma City Community College Effective Date: 07-01-2010 Aetna HealthFund Open Choice (PPO) - Oklahoma PLAN DESIGN AND BENEFITS PROVIDED BY AETNA LIFE INSURANCE COMPANY -
18 Medical Plan - Healthfund Oklahoma City Community College Effective Date: 07-01-2010 Aetna HealthFund Open Choice (PPO) - Oklahoma PLAN DESIGN AND BENEFITS PROVIDED BY AETNA LIFE INSURANCE COMPANY -
Preventive Care Services Health Care Reform The following benefits are effective beginning the first plan year on or after Sept.
 Coding Summary for Providers NOTE THE FOLLOWING: The purpose of this document is to provide a quick reference of the applicable codes for UnitedHealthcare plans that cover preventive care services in accordance
Coding Summary for Providers NOTE THE FOLLOWING: The purpose of this document is to provide a quick reference of the applicable codes for UnitedHealthcare plans that cover preventive care services in accordance
Research Triangle Institute Policy #04806A Benefits at a Glance Effective Date: January 1, 2013
 Research Triangle Institute Research Triangle Institute is offering Medical, Dental, Vision, Pharmacy, Medical Evacuation and Repatriation, and Long Term Disability> benefits through Cigna Global Health
Research Triangle Institute Research Triangle Institute is offering Medical, Dental, Vision, Pharmacy, Medical Evacuation and Repatriation, and Long Term Disability> benefits through Cigna Global Health
PLAN DESIGN AND BENEFITS AETNA LIFE INSURANCE COMPANY - Insured
 PLAN FEATURES Deductible (per calendar year) Individual $750 Individual $1,500 Family $2,250 Family $4,500 All covered expenses accumulate simultaneously toward both the preferred and non-preferred Deductible.
PLAN FEATURES Deductible (per calendar year) Individual $750 Individual $1,500 Family $2,250 Family $4,500 All covered expenses accumulate simultaneously toward both the preferred and non-preferred Deductible.
OverVIEW of Your Eligibility Class by determineing Benefits
 OVERVIEW OF YOUR BENEFITS IMPORTANT PHONE NUMBERS Benefit Fund s Member Services Department (646) 473-9200 For answers to questions about your eligibility or prescription drug benefit. You can also visit
OVERVIEW OF YOUR BENEFITS IMPORTANT PHONE NUMBERS Benefit Fund s Member Services Department (646) 473-9200 For answers to questions about your eligibility or prescription drug benefit. You can also visit
COVERAGE SCHEDULE. The following symbols are used to identify Maximum Benefit Levels, Limitations, and Exclusions:
 Exhibit D-3 HMO 1000 Coverage Schedule ROCKY MOUNTAIN HEALTH PLANS GOOD HEALTH HMO $1000 DEDUCTIBLE / 75 PLAN EVIDENCE OF COVERAGE LARGE GROUP Underwritten by Rocky Mountain Health Maintenance Organization,
Exhibit D-3 HMO 1000 Coverage Schedule ROCKY MOUNTAIN HEALTH PLANS GOOD HEALTH HMO $1000 DEDUCTIBLE / 75 PLAN EVIDENCE OF COVERAGE LARGE GROUP Underwritten by Rocky Mountain Health Maintenance Organization,
Bates College Effective date: 01-01-2010 HMO - Maine PLAN DESIGN AND BENEFITS PROVIDED BY AETNA HEALTH INC. - FULL RISK PLAN FEATURES
 PLAN FEATURES Deductible (per calendar year) $500 Individual $1,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Once Family Deductible is met, all family
PLAN FEATURES Deductible (per calendar year) $500 Individual $1,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Once Family Deductible is met, all family
Preventive Services at 100%
 September 1, 2014 Update Preventive Care Services Covered Without Cost-sharing Without Copay, Coinsurance or Deductible The Affordable Care Act (ACA) requires non-grandfathered health plans and policies
September 1, 2014 Update Preventive Care Services Covered Without Cost-sharing Without Copay, Coinsurance or Deductible The Affordable Care Act (ACA) requires non-grandfathered health plans and policies
PLAN DESIGN AND BENEFITS - PA Health Network Option AHF HRA 1.3. Fund Pays Member Responsibility
 HEALTHFUND PLAN FEATURES HealthFund Amount (Per plan year. Fund changes between tiers requires a life status change qualifying event.) Fund Coinsurance (Percentage at which the Fund will reimburse) Fund
HEALTHFUND PLAN FEATURES HealthFund Amount (Per plan year. Fund changes between tiers requires a life status change qualifying event.) Fund Coinsurance (Percentage at which the Fund will reimburse) Fund
Preventive care covered with no cost sharing
 Quality health plans & benefits Healthier living Financial well-being Intelligent solutions Preventive care covered with no cost sharing Get checkups, screenings, vaccines, prenatal care, contraceptives
Quality health plans & benefits Healthier living Financial well-being Intelligent solutions Preventive care covered with no cost sharing Get checkups, screenings, vaccines, prenatal care, contraceptives
Take advantage of preventive care to help manage your health
 Take advantage of preventive care to help manage your health Preventing disease and detecting health issues at an early stage, if they occur, are important to living a healthy life. Following these recommended
Take advantage of preventive care to help manage your health Preventing disease and detecting health issues at an early stage, if they occur, are important to living a healthy life. Following these recommended
Carnegie Mellon University Benefits at a Glance Policy #02424A Effective Date: 1/1/2015
 Carnegie Mellon University Benefits at a Glance Policy #02424A Effective Date: 1/1/2015 Carnegie Mellon University offers Medical, Pharmacy, Medical Evacuation and Repatriation, Vision, and Dental benefits
Carnegie Mellon University Benefits at a Glance Policy #02424A Effective Date: 1/1/2015 Carnegie Mellon University offers Medical, Pharmacy, Medical Evacuation and Repatriation, Vision, and Dental benefits
WHAT GRANDFATHERED PLANS DO AND DON'T HAVE TO COVER. Judy Pfriemer, Chair, Employee Benefits [email protected] HEALTH INSURANCE 2016???
 Judy Pfriemer, Chair, Employee Benefits [email protected] HEALTH INSURANCE 2016??? WHAT GRANDFATHERED PLANS DO AND DON'T HAVE TO COVER All health plans must End lifetime limits on coverage End arbitrary
Judy Pfriemer, Chair, Employee Benefits [email protected] HEALTH INSURANCE 2016??? WHAT GRANDFATHERED PLANS DO AND DON'T HAVE TO COVER All health plans must End lifetime limits on coverage End arbitrary
ACA Mandates First Dollar Coverage for Preventive Services
 I N F O R M A T I O N U P D A T E May 2013 ACA Mandates First Dollar Coverage for Preventive Services The Affordable Care Act (ACA) mandates that, effective for Plan Years beginning on or after Sept. 23,
I N F O R M A T I O N U P D A T E May 2013 ACA Mandates First Dollar Coverage for Preventive Services The Affordable Care Act (ACA) mandates that, effective for Plan Years beginning on or after Sept. 23,
$6,350 Individual $12,700 Individual
 PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible $5,000 Individual $10,000 Individual $10,000 Family $20,000 Family All covered expenses accumulate separately toward the preferred or non-preferred Deductible.
PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible $5,000 Individual $10,000 Individual $10,000 Family $20,000 Family All covered expenses accumulate separately toward the preferred or non-preferred Deductible.
Preventive Health Services
 understanding Preventive Health Services For the most current version of this document, visit www.wellwithbluemt.com or www.bcbsmt.com. Preventive health services include evidence-based screenings, immunizations,
understanding Preventive Health Services For the most current version of this document, visit www.wellwithbluemt.com or www.bcbsmt.com. Preventive health services include evidence-based screenings, immunizations,
20% 40% Individual Family
 PLAN FEATURES NON-* Deductible (per calendar year) $2,500 Individual $3,000 Individual $5,000 Family $6,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
PLAN FEATURES NON-* Deductible (per calendar year) $2,500 Individual $3,000 Individual $5,000 Family $6,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
Individual. Employee + 1 Family
 FUND FEATURES HealthFund Amount Individual Employee + 1 Family $750 $1,125 $1,500 Amount contributed to the Fund by the employer is reflected above. Fund Amount reflected is on a per calendar year basis.
FUND FEATURES HealthFund Amount Individual Employee + 1 Family $750 $1,125 $1,500 Amount contributed to the Fund by the employer is reflected above. Fund Amount reflected is on a per calendar year basis.
Health Net Life Insurance Company California Farm Bureau Members Health Insurance Plans Major Medical Expense Coverage Outline of Coverage
 Health Net Life Insurance Company California Farm Bureau Members Health Insurance Plans Major Medical Expense Coverage Outline of Coverage Read Your Certificate Carefully This outline of coverage provides
Health Net Life Insurance Company California Farm Bureau Members Health Insurance Plans Major Medical Expense Coverage Outline of Coverage Read Your Certificate Carefully This outline of coverage provides
Employer Sponsored Minimum Essential Coverage (MEC)
 P.O. Box 129 Fort Mill, SC 29716 1-877-851-0906 SAMPLE EMPLOYEE SR 123 STREET RD Date: 05/01/2014 ANY, WI 12345 Group Number: M0001023 Employer Sponsored Minimum Essential Coverage (MEC) Your employer
P.O. Box 129 Fort Mill, SC 29716 1-877-851-0906 SAMPLE EMPLOYEE SR 123 STREET RD Date: 05/01/2014 ANY, WI 12345 Group Number: M0001023 Employer Sponsored Minimum Essential Coverage (MEC) Your employer
Understanding preventive care
 Understanding preventive care We want you to be your healthiest. That s why the preventive services listed here are free for most members. What services are recommended? Know before you go. Preventive
Understanding preventive care We want you to be your healthiest. That s why the preventive services listed here are free for most members. What services are recommended? Know before you go. Preventive
Additional Information Provided by Aetna Life Insurance Company
 Additional Information Provided by Aetna Life Insurance Company Inquiry Procedure The plan of benefits described in the Booklet-Certificate is underwritten by: Aetna Life Insurance Company (Aetna) 151
Additional Information Provided by Aetna Life Insurance Company Inquiry Procedure The plan of benefits described in the Booklet-Certificate is underwritten by: Aetna Life Insurance Company (Aetna) 151
Employee + 2 Dependents
 FUND FEATURES HealthFund Amount $500 Individual $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance Percentage at
FUND FEATURES HealthFund Amount $500 Individual $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance Percentage at
PDS Tech, Inc Proposed Effective Date: 01-01-2012 Aetna HealthFund Aetna Choice POS ll - ASC
 FUND FEATURES HealthFund Amount $500 Individual $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance 100% Percentage
FUND FEATURES HealthFund Amount $500 Individual $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance 100% Percentage
SPIN Effective Date: 01-01-2013 Aetna HealthFund Aetna Choice POS ll - ASC PLAN DESIGN & BENEFITS ADMINISTERED BY AETNA LIFE INSURANCE COMPANY
 HealthFund Amount $1,500 Employee $1,500 Employee + 1 Dependent $1,500 Employee + 2 Dependents $1,500 Family Amount contributed to Fund by employer Fund Coinsurance 100% Percentage at which Fund will reimburse
HealthFund Amount $1,500 Employee $1,500 Employee + 1 Dependent $1,500 Employee + 2 Dependents $1,500 Family Amount contributed to Fund by employer Fund Coinsurance 100% Percentage at which Fund will reimburse
Rice University Effective Date: 07-01-2014 Aetna Choice POS ll - ASC PLAN DESIGN & BENEFITS ADMINISTERED BY AETNA LIFE INSURANCE COMPANY PLAN FEATURES
 PLAN DESIGN & BENEFITS PLAN FEATURES NON- Deductible (per calendar year) None Individual $1,000 Individual None Family $3,000 Family All covered expenses, excluding prescription drugs, accumulate toward
PLAN DESIGN & BENEFITS PLAN FEATURES NON- Deductible (per calendar year) None Individual $1,000 Individual None Family $3,000 Family All covered expenses, excluding prescription drugs, accumulate toward
Active and Retiree Health Benefit Summary Plan Description And Plan Document 7670-00-411309/7670-03-411309
 Active and Retiree Health Benefit Summary Plan Description And Plan Document 7670-00-411309/7670-03-411309 BENEFITS ADMINISTERED BY Table of Contents INTRODUCTION... 1 PLAN INFORMATION... 2 BENEFIT CLASS
Active and Retiree Health Benefit Summary Plan Description And Plan Document 7670-00-411309/7670-03-411309 BENEFITS ADMINISTERED BY Table of Contents INTRODUCTION... 1 PLAN INFORMATION... 2 BENEFIT CLASS
100% Fund Administration
 FUND FEATURES HealthFund Amount $500 Employee $750 Employee + Spouse $750 Employee + Child(ren) $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance Percentage at which the Fund
FUND FEATURES HealthFund Amount $500 Employee $750 Employee + Spouse $750 Employee + Child(ren) $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance Percentage at which the Fund
Business Life Insurance - Health & Medical Billing Requirements
 PLAN FEATURES Deductible (per plan year) $2,000 Employee $2,000 Employee $3,000 Employee + Spouse $3,000 Employee + Spouse $3,000 Employee + Child(ren) $3,000 Employee + Child(ren) $4,000 Family $4,000
PLAN FEATURES Deductible (per plan year) $2,000 Employee $2,000 Employee $3,000 Employee + Spouse $3,000 Employee + Spouse $3,000 Employee + Child(ren) $3,000 Employee + Child(ren) $4,000 Family $4,000
Hawaii Benchmarks Benefits under the Affordable Care Act (ACA)
 Hawaii Benchmarks Benefits under the Affordable Care Act (ACA) 10/2012 Coverage for Newborn and Foster Children Coverage Outside the Provider Network Adult Routine Physical Exams Well-Baby and Well-Child
Hawaii Benchmarks Benefits under the Affordable Care Act (ACA) 10/2012 Coverage for Newborn and Foster Children Coverage Outside the Provider Network Adult Routine Physical Exams Well-Baby and Well-Child
Aetna HealthFund Health Reimbursement Account Plan (Aetna HealthFund Open Access Managed Choice POS II )
 Health Fund The Health Fund amount reflected is on a per calendar year basis. If you do not use the entire fund by 12/31/2015, it will be moved into a Limited-Purpose Flexible Spending Account. Health
Health Fund The Health Fund amount reflected is on a per calendar year basis. If you do not use the entire fund by 12/31/2015, it will be moved into a Limited-Purpose Flexible Spending Account. Health
Greater Tompkins County Municipal Health Insurance Consortium
 WHO IS COVERED Requires both Medicare A & B enrollment. Type of Coverage Offered Single only Single only MEDICAL NECESSITY Pre-Certification Requirement None None Medical Benefit Management Program Not
WHO IS COVERED Requires both Medicare A & B enrollment. Type of Coverage Offered Single only Single only MEDICAL NECESSITY Pre-Certification Requirement None None Medical Benefit Management Program Not
2015 Medicare Advantage Summary of Benefits
 2015 Medicare Advantage Summary of Benefits HNE Medicare Premium No Rx and HNE Medicare Basic No Rx January 1, 2015 - December 31, 2015 H8578_2015_034 Accepted HNE MEDICARE ADVANTAGE ENROLLMENT KIT 2015
2015 Medicare Advantage Summary of Benefits HNE Medicare Premium No Rx and HNE Medicare Basic No Rx January 1, 2015 - December 31, 2015 H8578_2015_034 Accepted HNE MEDICARE ADVANTAGE ENROLLMENT KIT 2015
DynCorp International LLC US Expat Plan Benefits at a Glance Policy # 00257A Effective Date: January 1, 2015
 DynCorp LLC US Expat Plan Benefits at a Glance Policy # 00257A Effective Date: January 1, 2015 DynCorp LLC is offering Medical, Dental, Vision, Pharmacy, Medical Evacuation and Repatriation benefits to
DynCorp LLC US Expat Plan Benefits at a Glance Policy # 00257A Effective Date: January 1, 2015 DynCorp LLC is offering Medical, Dental, Vision, Pharmacy, Medical Evacuation and Repatriation benefits to
Important health care reform notice Women s preventive services covered with no member cost share
 Quality health plans & benefits Healthier living Financial well-being Intelligent solutions Important health care reform notice Women s preventive services covered with no member cost share www.aetna.com
Quality health plans & benefits Healthier living Financial well-being Intelligent solutions Important health care reform notice Women s preventive services covered with no member cost share www.aetna.com
Commercial. Individual & Family Plan. Health Net California Farm Bureau and PPO. Insurance Plans. Outline of Coverage and Exclusions and Limitations
 Commercial Individual & Family Plan Health Net California Farm Bureau and PPO Insurance Plans Outline of Coverage and Exclusions and Limitations Table of Contents Health Plans Outline of coverage 1 Read
Commercial Individual & Family Plan Health Net California Farm Bureau and PPO Insurance Plans Outline of Coverage and Exclusions and Limitations Table of Contents Health Plans Outline of coverage 1 Read
Sherwin-Williams Medical, Prescription Drug and Dental Plans Plan Comparison Charts
 Sherwin-Williams Medical, Prescription Drug and Dental Plans Plan Comparison Charts You and Sherwin-Williams share the cost of certain benefits including medical and dental coverage and you have the opportunity
Sherwin-Williams Medical, Prescription Drug and Dental Plans Plan Comparison Charts You and Sherwin-Williams share the cost of certain benefits including medical and dental coverage and you have the opportunity
Illinois Insurance Facts Illinois Department of Insurance
 Illinois Insurance Facts Illinois Department of Insurance Women s Health Care Issues Revised August 2012 Note: This information was developed to provide consumers with general information and guidance
Illinois Insurance Facts Illinois Department of Insurance Women s Health Care Issues Revised August 2012 Note: This information was developed to provide consumers with general information and guidance
A B. C Plan C: It s Time to Choose Your 2015 Health Benefits. Plan A
 HABLAMOS ESPANOL! Open Enrollment ends March 27. It s Time to Choose Your 2015 Health Benefits choose one... A B Plan A Wellness + Preventive $7.83 / week Plan B Plan A + Hospital Indemnity + Sickness,
HABLAMOS ESPANOL! Open Enrollment ends March 27. It s Time to Choose Your 2015 Health Benefits choose one... A B Plan A Wellness + Preventive $7.83 / week Plan B Plan A + Hospital Indemnity + Sickness,
The Healthy Michigan Plan Handbook
 The Healthy Michigan Plan Handbook Introduction The Healthy Michigan Plan is a health care program through the Michigan Department of Community Health (MDCH). Eligibility for this program will be determined
The Healthy Michigan Plan Handbook Introduction The Healthy Michigan Plan is a health care program through the Michigan Department of Community Health (MDCH). Eligibility for this program will be determined
The Healthy Michigan Plan Handbook
 The Healthy Michigan Plan Handbook Introduction The Healthy Michigan Plan is a health care program through the Michigan Department of Community Health (MDCH). The Healthy Michigan Plan provides health
The Healthy Michigan Plan Handbook Introduction The Healthy Michigan Plan is a health care program through the Michigan Department of Community Health (MDCH). The Healthy Michigan Plan provides health
MedStar Family Choice Benefits Summary District of Columbia- Healthy Families WHAT YOU GET WHO CAN GET THIS BENEFIT BENEFIT
 Primary Care Services Specialist Services Laboratory & X-ray Services Hospital Services Pharmacy Services (prescription drugs) Emergency Services Preventive, acute, and chronic health care Services generally
Primary Care Services Specialist Services Laboratory & X-ray Services Hospital Services Pharmacy Services (prescription drugs) Emergency Services Preventive, acute, and chronic health care Services generally
Summary of Benefits Community Advantage (HMO)
 Summary of Benefits Community Advantage (HMO) January 1, 2015 - December 31, 2015 This booklet gives you a summary of what we cover and what you pay. It doesn't list every service that we cover or list
Summary of Benefits Community Advantage (HMO) January 1, 2015 - December 31, 2015 This booklet gives you a summary of what we cover and what you pay. It doesn't list every service that we cover or list
CA Group Business 2-50 Employees
 PLAN FEATURES Network Primary Care Physician Selection Deductible (per calendar year) Member Coinsurance Copay Maximum (per calendar year) Lifetime Maximum Referral Requirement PHYSICIAN SERVICES Primary
PLAN FEATURES Network Primary Care Physician Selection Deductible (per calendar year) Member Coinsurance Copay Maximum (per calendar year) Lifetime Maximum Referral Requirement PHYSICIAN SERVICES Primary
If you have a question about whether MedStar Family Choice covers certain health care, call MedStar Family Choice Member Services at 888-404-3549.
 Your Health Benefits Health services covered by MedStar Family Choice The list below shows the healthcare services and benefits for all MedStar Family Choice members. For some benefits, you have to be
Your Health Benefits Health services covered by MedStar Family Choice The list below shows the healthcare services and benefits for all MedStar Family Choice members. For some benefits, you have to be
Resourcing Christian Education International Policy # 06100A Benefits at a Glance Effective Date August 1, 2013
 Resourcing Christian Education International is offering Medical, Vision, Pharmacy, and Medical Evacuation and Repatriation benefits through Cigna Global Health Benefits to our employees. This comprehensive
Resourcing Christian Education International is offering Medical, Vision, Pharmacy, and Medical Evacuation and Repatriation benefits through Cigna Global Health Benefits to our employees. This comprehensive
