Preventive Services versus Diagnostic and/or Medical Services
|
|
|
- Julianna Robinson
- 10 years ago
- Views:
Transcription
1 Manual: Policy Title: Reimbursement Policy Preventive Services versus Diagnostic and/or Medical Services Section: Administrative Subsection: None Date of Origin: 1/1/2000 Policy Number: RPM037 Last Updated: 10/15/2015 Last Reviewed: 10/21/2015 IMPORTANT STATEMENT The purpose of Moda Health Reimbursement Policy (formerly ODS Health Plan, Inc.) is to document payment policy for covered medical and surgical services and supplies. Health care providers (facilities, physicians and other professionals) are expected to exercise independent medical judgment in providing care to members. Reimbursement policy is not intended to impact care decisions or medical practice. Providers are responsible for accurately, completely, and legibly documenting the services performed. The billing office is expected to submit claims for services rendered using valid codes from HIPAA-approved code sets. Claims should be coded appropriately according to industry standard coding guidelines (including but not limited to UB Editor, AMA, CPT, CPT Assistant, HCPCS, DRG guidelines, CMS National Correct Coding Initiative (CCI/NCCI) Policy Manual, CCI table edits and other CMS guidelines). Benefit determinations will be based on the applicable member contract language. To the extent there are any conflicts between the Moda Health Reimbursement Policy and the member contract language, the member contract language will prevail, to the extent of any inconsistency. Fee determinations will be based on the applicable provider contract language and Moda Health reimbursement policy. To the extent there are any conflicts between Reimbursement Policy and the provider contract language, the provider contract language will prevail. Purpose of Policy This policy is intended to help clarify how and why the same test or service may process differently depending upon the primary diagnosis code with which it is billed. The focus of this policy is on the differences between the Preventive and the Medical benefit categories.
2 Codes and Definitions Summary of Synonyms: Preventive = Screening = Routine benefits Prophylactic = Preventive Medical = Diagnostic or Therapeutic Definition of Terms: Diagnostic (no symptoms or problems) (no symptoms or problems) (symptoms or problems exist) The member is having symptoms or health problems. Tests and/or procedures are ordered to assist in determining the cause of the symptoms or health problems. Diagnostic tests are considered under the Medical benefit category. They are never considered Preventive Care. A problem already exists. Diagnostic services are performed to obtain information to aid in the assessment of a medical condition or the identification of a disease to determine the nature and severity of an ailment or injury. (CMS 4 ) Medical Preventive Care Preventive Services Medical services are those which are recommended by a doctor in order to diagnose symptoms, or treat or monitor a known medical condition, health problem, or disease. If it's testing that's being done, it might be called diagnostic testing. Preventive, in insurance terms, is synonymous with routine or screening. Preventive, in medical terms, is also synonymous with prophylactic. Preventive service(s) are provided to help [the member] avoid becoming sick in the first place. (healthinsurance.org 1 ) Preventive tests and services are performed when the member has no signs or symptoms, no indications that they are not healthy. [Preventive Care is] a pattern of nursing and medical care that focuses on disease prevention and health maintenance. It includes early diagnosis of disease, discovery and identification of people at risk of development of specific problems, counseling, and other necessary intervention to avert a health problem. Screening tests, health education, and immunization programs are common examples of preventive care. (Mosby 2) Prophylactic Guarding from or preventing the spread or occurrence of disease or infection. Tending to prevent or ward off. Preventive. (Merriam Webste 5 ) Synonyms: Preventive, Precautionary. (Merriam Webste 5 ) Page 2 of 10
3 Routine Routine, in insurance terms, is synonymous with screening or preventative. Routine services are those things that doctors recommend to ordinary people, who are healthy as far as they know, in order to screen them for things that may not be causing symptoms yet. There are no known health problems, symptoms, chronic conditions, or injuries. Synonyms: Preventive, Screening Routine Monitoring Routine monitoring of an existing health condition (such as diabetes or high cholesterol) is not a routine preventive service. In this case, the word routine does not refer to the health insurance benefit category, but rather it means that the testing or care is considered a medical standard of care for the patient s known problem or condition. Anytime a known condition or problem exists, the testing and care for that condition is never considered preventive; instead it is covered under the benefit category for that condition (e.g. Medical, Chemical Dependency, Maternity, Infertility, etc.). Screening Services Screening, in insurance terms, is synonymous with routine or preventative. Screening is the testing for disease or disease precursors in seemingly well individuals so that early detection and treatment can be provided for those who test positive for the disease. (Optum 6 ) (emphasis added) Tests or procedures performed for a patient who does not have symptoms, abnormal findings, or any past history of the disease; used to detect an undiagnosed disease so that medical treatment can begin. (McGraw-Hill 3 ) Surveillance Close and continuous observation or testing (Merriam Webste 5 ) Surveillance testing is considered Medical if it is being done to observe or monitor a known symptom or problem. The diagnosis code needs to indicate the problem or symptom which is being observed or monitored. Surveillance testing is considered Preventive if the patient is being observed because of risk factors (e.g. work environment) or due to family history. Page 3 of 10
4 Modifier Definitions: Modifier 33 Modifier PT Modifier GA Modifier GX Preventive Services: When the primary purpose of the service is the delivery of an evidence based service in accordance with a US Preventive Services Task Force A or B rating in effect and other preventive services identified in preventive services mandates (legislative or regulatory), the service may be identified by adding 33 to the procedure. For separately reported services specifically identified as preventive, the modifier should not be used. Colorectal cancer screening test; converted to diagnostic test or other procedure Waiver of liability statement issued as required by payer policy, individual case Notice of liability issued, voluntary under payer policy General Information Sometimes, the exact same test or procedure can be covered by a member s plan in two or more different ways, depending upon why it is being done. The primary (or first-listed) diagnosis code billed describes the chief reason why the service is being done, which can affect the processing and benefit level for the service. This is one of many reasons that it is critical to accurately select the diagnosis code when submitting claims for these services. Member plans have different benefit levels and cost-sharing responsibilities for Preventive Services versus Medical Services. Although member plans do vary, medical services generally apply to the member s deductible and generally have copays and/or coinsurance. Preventive services mandated by the Patient Protection and Affordable Care Act are covered at 100% (no cost-sharing). Some lab tests and other procedures are eligible for either Preventive or Medical benefit categories, depending upon why they are done and the frequency performed. Other tests are only eligible for Medical benefits and are not covered at all under the Preventive benefit. Coding Guidelines Selection of Principle Diagnosis: The circumstances of inpatient admission always govern the selection of principle diagnosis. The principle diagnosis is defined in the Uniform Hospital Discharge Data Set (UHDDS) as that condition established after study to be chiefly responsible for occasioning the admission of the patient to the hospital for care. (Optum 7 ) In the outpatient setting, the term first-listed diagnosis is used in lieu of principle diagnosis. (Optum 8 ) Page 4 of 10
5 List first the ICD-9-CM code for the diagnosis, condition, problem, or other reason for encounter/visit shown in the medical record to be chiefly responsible for the services provided In some cases the first-listed diagnosis may be a symptom when a diagnosis has not been established (confirmed) by the physician. (Optum 9 ) List first the ICD-10-CM code for the diagnosis, condition, problem, or other reason for encounter/visit shown in the medical record to be chiefly responsible for the services provided In some cases the first-listed diagnosis may be a symptom when a diagnosis has not been established (confirmed) by the physician. (Optum 11 ) Reimbursement Guidelines A. Categories of diagnostic tests covered and not covered as routine/preventive 1. Moda Health covers the preventive services mandated in the Patient Protection and Affordable Care Act (PPACA) at 100% (no cost-sharing responsibility to the member), when the member is seeing an in-network provider. 2. In addition, Moda Health covers a limited list of additional tests when billed with a routine, preventive, or screening diagnosis code. These tests are not on the PPACA list of mandated preventive services and so are not eligible for the 100%, no-cost-share Affordable Care Act preventive benefit. The tests will be covered but are subject to the member s usual costsharing and deductible requirements. The following additional CPT codes will be covered as noted above with a routine/preventive/screening diagnosis: (Basic metabolic panel) (General health panel) 80051(Electrolyte panel) (Comprehensive metabolic panel) (Lipid panel) (Urinalysis, by dip stick or tablet reagent; automated, with microscopy) (Calcium; total) (Hemoglobin; glycosylated (A1C)) (Lead) (Thyroid stimulating hormone (TSH)) (Blood count; complete (CBC), automated) Chlamydia screening for males (87110, 87270, 87370, 87490, 87491, 87492, 87810) (Note: female Chlamydia screening covered under 100%) Gonorrhea (gonorrhoeae) screening for males (87590, and 87592) (Note: female Gonorrhea (gonorrhoeae) screening covered under 100%) Page 5 of 10
6 3. The remainder of lab procedure codes and diagnostic services are covered when billed with a medical diagnosis code (diagnosis indicating the member has symptoms or problems) but are considered non-covered and will be denied if billed with a routine/preventive diagnosis code. Financial responsibility for non-covered screening lab tests: a. Provider Responsibility. Non-covered screening lab procedure codes will be denied to provider responsibility, as Moda Health believes the lack of a symptom or medical problem diagnosis code for these tests most often represents an oversight or billing error on the claim for which the member should not be financially liable. b. Member Responsibility. Effective for claims with date of service 02/01/2015 and after: When these non-covered screening procedure codes are performed in the absence of any symptoms or problems because either you or the member believes one of these tests is needed for screening purposes, the denials may be processed to member responsibility when all of the following requirements are met: i. The member signs and dates a waiver of liability form on or prior to the date of service. a) The services must be performed or initiated within 30-days of when the waiver of liability was signed. b) For an ongoing course of treatment and/or rental, the waiver is valid for no more than one year from the date of the member signature. A new waiver of liability would need to be obtained before billing additional services beyond one year. ii. The procedure codes are billed with modifier GA or GX appended. a) Please be prepared to submit a copy of the waiver of liability form upon request should review become necessary (e.g. in case of a member appeal). b) If the original claim was submitted without modifier GA or GX and a corrected claim needs to be submitted, a copy of the waiver of liability form needs to accompany the corrected claim to support the change in coding from the original submitted claim. For dates of service 1/31/2015 and prior, non-covered screening procedure codes are denied to provider write-off (see 3.a above). To request a change of financial liability to member responsibility, the billing office may submit a copy of a signed waiver of liability form with a written appeal for review. A corrected claim with modifiers GA or GX will not be required for these dates of service. Page 6 of 10
7 4. To summarize categories # 1, 2, & 3 above, Moda Health covers routine/preventive testing as follows: Covered at 100%: (if performed by in-network provider) (mandated, category 1 ) List of preventive services mandated in the Patient Protection and Affordable Care Act (PPACA). Covered, not necessarily at 100% level. Deductible and usual member cost-sharing apply. (not mandated, category 2 ) 80048, 80050, 80051, 80053, 80061, 81001, 82310, 83036, 83655, 84443, 85025, 87110, 87270, 87370, 87490, 87491, 87492, 87810, 87590, and Not covered for routine, preventive, or screening diagnosis codes: (not covered, category 3 ) All other tests. B. Determining the benefit category for processing: Proper payment of preventive services by Moda Health is dependent upon claim submission using diagnosis and procedure codes which identify the services as preventive. Moda Health categorizes diagnosis codes as follows: Personal history of diagnosis codes are considered Medical. Family history of diagnosis codes are considered Preventive. (Please check to verify benefits.) Screening diagnosis codes are considered Preventive. Routine diagnosis codes are considered Preventive. For example: ICD-9-CM codes V20.2, V70.0 or ICD-10-CM codes Z00.121, Z00.129, Z00.00, Z00.01 Prophylactic diagnosis codes are considered Preventive. NOTE: There are many V-codes (ICD-9 diagnosis codes beginning with the letter V) which are not considered routine/preventive. Examples include V58.1 (encounter for chemotherapy) and V54.0 (aftercare involving removal of fracture plate or other internal fixation device). Just because a service is billed with a V-code diagnosis does not automatically make it a routine/preventive service. Similarly, ICD-10 diagnosis codes in chapter 21 (beginning with Z ) are not automatically considered routine/preventive; some will be considered medical diagnosis codes. The determination is based upon the code description, not merely in which section of the code set the code is found. C. Diagnostic Services Combined with a Preventive E/M Visit If an abnormality is encountered or a problem existing prior to this visit is addressed in the process of performing the preventive medicine evaluation, CPT guidelines define the Page 7 of 10
8 documentation and coding requirements for reporting an additional problem-oriented E/M service in combination with the preventive E/M service code. Similarly, lab tests ordered at an annual preventive health visit ( ) are not all automatically eligible for coverage at the 100%, no-cost-share Affordable Care Act preventive benefit, only those tests mandated by the PPACA. Additional tests ordered because of problems existing prior to this visit, abnormalities, or new problems encountered during the preventive visit are to be billed with the diagnosis code to describe the problem or reason the test was ordered, not the diagnosis code for the preventive visit. These additional tests are considered Medical, not Preventive. D. Modifier 33 (Preventive Services) Moda Health has configured our system to properly apply the PPACA benefit for mandated tests regardless of the presence or absence of modifier 33. E. Modifier PT (Colorectal cancer screening test; converted to diagnostic test or other procedure) The following procedure codes are configured as valid to use in combination with modifier PT: Code Code Definition Colonoscopy, rigid or flexible, transabdominal via colotomy, single or multiple Colonoscopy, flexible, proximal to splenic flexure; diagnostic, with or without collection of specimen(s) by brushing or washing, with or without colon decompression (separate procedure) Colonoscopy, flexible, proximal to splenic flexure; with removal of foreign body Colonoscopy, flexible, proximal to splenic flexure; with biopsy, single or multiple Colonoscopy, flexible, proximal to splenic flexure; with directed submucosal injection(s), any substance Colonoscopy, flexible, proximal to splenic flexure; with control of bleeding (eg, injection, bipolar cautery, unipolar cautery, laser, heater probe, stapler, plasma coagulator) Colonoscopy, flexible, proximal to splenic flexure; with ablation of tumor(s), polyp(s), or other lesion(s) not amenable to removal by hot biopsy forceps, bipolar cautery or snare technique Colonoscopy, flexible, proximal to splenic flexure; with removal of tumor(s), polyp(s), or other lesion(s) by hot biopsy forceps or bipolar cautery Colonoscopy, flexible, proximal to splenic flexure; with removal of tumor(s), polyp(s), or other lesion(s) by snare technique Colonoscopy, flexible, proximal to splenic flexure; with dilation by balloon, 1 or more strictures Colonoscopy, flexible, proximal to splenic flexure; with transendoscopic stent placement (includes predilation) Colonoscopy, flexible, proximal to splenic flexure; with endoscopic ultrasound examination Page 8 of 10
9 Code Code Definition Colonoscopy, flexible, proximal to splenic flexure; with transendoscopic ultrasound guided intramural or transmural fine needle aspiration/biopsy(s) G0105 Colorectal cancer screening; colonoscopy on individual at high risk G0120 Colorectal cancer screening; alternative to G0105, screening colonoscopy, barium enema G0121 Colorectal cancer screening; colonoscopy on individual not meeting criteria for high risk Cross References Moda Health Plan Adult and Child Preventive Services summaries. To locate, go to and search for keyword preventive. (See: ) References & Resources 1. healthinsurance.org. last accessed 10/31/ Mosby's Medical Dictionary, 8th edition. 2009, Elsevier. last accessed 10/31/ last accessed 10/31/ CMS. Diagnostic Services Defined. Medicare Benefit Policy Manual (Pub ). Chapter 6, Merriam Webster. Online Medical Dictionary Official ICD-9-CM Guidelines for Coding and Reporting, I, C, 18, d, 5). ICD-9-CM Optum: Official ICD-9-CM Guidelines for Coding and Reporting, II. ICD-9-CM Optum: Official ICD-9-CM Guidelines for Coding and Reporting, IV, A, 1 & 2. ICD-9-CM Optum: Official ICD-9-CM Guidelines for Coding and Reporting, IV, H. ICD-9-CM Optum: Rodriguez, Denis, CPC. "Keep up with ASC Colonoscopy Clarifications." AAPC Cutting Edge, May 2013: pp Page 9 of 10
10 11. Official ICD-10-CM Guidelines for Coding and Reporting, IV, G. ICD-9-CM Optum: Page 10 of 10
Billing Guideline. Subject: Colorectal Cancer Screening Exams (Invasive Procedures) Effective Date: 1/1/2012 Last Update Effective: 4/16
 Subject: Colorectal Cancer Screening Exams (Invasive Procedures) Effective Date: 1/1/2012 Last Update Effective: 4/16 Billing Guideline Background Health First administers benefit packages with full coverage
Subject: Colorectal Cancer Screening Exams (Invasive Procedures) Effective Date: 1/1/2012 Last Update Effective: 4/16 Billing Guideline Background Health First administers benefit packages with full coverage
LOWER GI ENDOSCOPIES So why is CMS yanking our chain? General Concepts for all GI Endoscopy Procedures
 LOWER GI ENDOSCOPIES We have lots of changes to lower GI coding for 2015 to talk about. Code definitions have been revised and many new codes have been added to this chapter. First the good news: All these
LOWER GI ENDOSCOPIES We have lots of changes to lower GI coding for 2015 to talk about. Code definitions have been revised and many new codes have been added to this chapter. First the good news: All these
The Official Guidelines for coding and reporting using ICD-9-CM
 Reporting Accurate Codes In the Era of Recovery Audit Contractor Reviews Sue Roehl, RHIT, CCS The Official Guidelines for coding and reporting using ICD-9-CM A set of rules that have been developed to
Reporting Accurate Codes In the Era of Recovery Audit Contractor Reviews Sue Roehl, RHIT, CCS The Official Guidelines for coding and reporting using ICD-9-CM A set of rules that have been developed to
Payment Policy. Evaluation and Management
 Purpose Payment Policy Evaluation and Management The purpose of this payment policy is to define how Health New England (HNE) reimburses for Evaluation and Management Services. Applicable Plans Definitions
Purpose Payment Policy Evaluation and Management The purpose of this payment policy is to define how Health New England (HNE) reimburses for Evaluation and Management Services. Applicable Plans Definitions
2015 CPT coding changes will have mixed effects on payment for general surgeons
 CPT coding changes will have mixed effects on payment for general surgeons 17 by Linda Barney, MD, FACS, and Mark T. Savarise, MD, FACS JAN BULLETIN American College of Surgeons 18 Significant changes
CPT coding changes will have mixed effects on payment for general surgeons 17 by Linda Barney, MD, FACS, and Mark T. Savarise, MD, FACS JAN BULLETIN American College of Surgeons 18 Significant changes
Modifier -25 Significant, Separately Identifiable E/M Service
 Manual: Policy Title: Reimbursement Policy Modifier -25 Significant, Separately Identifiable E/M Service Section: Modifiers Subsection: None Date of Origin: 1/1/2000 Policy Number: RPM028 Last Updated:
Manual: Policy Title: Reimbursement Policy Modifier -25 Significant, Separately Identifiable E/M Service Section: Modifiers Subsection: None Date of Origin: 1/1/2000 Policy Number: RPM028 Last Updated:
Modifiers XE, XS, XP, XU, and 59 - Distinct Procedural Service
 Manual: Policy Title: Reimbursement Policy Modifiers XE, XS, XP, XU, and 59 - Distinct Procedural Service Section: Modifiers Subsection: None Date of Origin: 1/1/2000 Policy Number: RPM027 Last Updated:
Manual: Policy Title: Reimbursement Policy Modifiers XE, XS, XP, XU, and 59 - Distinct Procedural Service Section: Modifiers Subsection: None Date of Origin: 1/1/2000 Policy Number: RPM027 Last Updated:
Modifiers 80, 81, 82, and AS - Assistant At Surgery
 Manual: Policy Title: Reimbursement Policy Modifiers 80, 81, 82, and AS - Assistant At Surgery Section: Modifiers Subsection: None Date of Origin: 1/1/2000 Policy Number: RPM013 Last Updated: 8/29/2014
Manual: Policy Title: Reimbursement Policy Modifiers 80, 81, 82, and AS - Assistant At Surgery Section: Modifiers Subsection: None Date of Origin: 1/1/2000 Policy Number: RPM013 Last Updated: 8/29/2014
Routine Venipuncture and/or Collection of Specimens
 Manual: Policy Title: Reimbursement Policy Routine Venipuncture and/or Collection of Specimens Section: Laboratory & Pathology Subsection: None Date of Origin: 1/1/2000 Policy Number: RPM012 Last Updated:
Manual: Policy Title: Reimbursement Policy Routine Venipuncture and/or Collection of Specimens Section: Laboratory & Pathology Subsection: None Date of Origin: 1/1/2000 Policy Number: RPM012 Last Updated:
Preventive Service HCPCS. Procedure Description ICD-9 Codes Modifier 33 Required? Page 1 of 6
 Well-Woman Exam G0101 Cervical or vaginal cancer screening; pelvic and clinical breast examination Breast Cancer V72.31 77057 Screening mammography, bilateral (2-view film study of each breast) V10.3 77052
Well-Woman Exam G0101 Cervical or vaginal cancer screening; pelvic and clinical breast examination Breast Cancer V72.31 77057 Screening mammography, bilateral (2-view film study of each breast) V10.3 77052
Modifiers 58, 78, and 79 Staged, Related, and Unrelated Procedures
 Manual: Policy Title: Reimbursement Policy Modifiers 58, 78, and 79 Staged, Related, and Unrelated Procedures Section: Modifiers Subsection: None Date of Origin: 9/22/2004 Policy Number: RPM010 Last Updated:
Manual: Policy Title: Reimbursement Policy Modifiers 58, 78, and 79 Staged, Related, and Unrelated Procedures Section: Modifiers Subsection: None Date of Origin: 9/22/2004 Policy Number: RPM010 Last Updated:
How To Write A Procedure Code
 Manual: Policy Title: Reimbursement Policy Technical Component (TC), Professional Component (PC/26), and Global Service Billing Section: Modifiers Subsection: None Date of Origin: 1/1/2000 Policy Number:
Manual: Policy Title: Reimbursement Policy Technical Component (TC), Professional Component (PC/26), and Global Service Billing Section: Modifiers Subsection: None Date of Origin: 1/1/2000 Policy Number:
Local Coverage Article: Venipuncture Necessitating Physician s Skill for Specimen Collection Supplemental Instructions Article (A50852)
 Local Coverage Article: Venipuncture Necessitating Physician s Skill for Specimen Collection Supplemental Instructions Article (A50852) Contractor Information Contractor Name CGS Administrators, LLC Article
Local Coverage Article: Venipuncture Necessitating Physician s Skill for Specimen Collection Supplemental Instructions Article (A50852) Contractor Information Contractor Name CGS Administrators, LLC Article
The Impact of Modifiers. By: Rhonda Granja, B.S.,CMA, CMC, CPC, CMOM
 The Impact of Modifiers By: Rhonda Granja, B.S.,CMA, CMC, CPC, CMOM A modifier provides the means to report or indicate that a service or procedure that has been performed has been altered by some specific
The Impact of Modifiers By: Rhonda Granja, B.S.,CMA, CMC, CPC, CMOM A modifier provides the means to report or indicate that a service or procedure that has been performed has been altered by some specific
IN-NETWORK MEMBER PAYS. Out-of-Pocket Maximum (Includes a combination of deductible, copayments and coinsurance for health and pharmacy services)
 HMO-OA-CNT-30-45-500-500D-13 HMO Open Access Contract Year Plan Benefit Summary This is a brief summary of benefits. Refer to your Membership Agreement for complete details on benefits, conditions, limitations
HMO-OA-CNT-30-45-500-500D-13 HMO Open Access Contract Year Plan Benefit Summary This is a brief summary of benefits. Refer to your Membership Agreement for complete details on benefits, conditions, limitations
CPT COD1NG UPDATES Gastroenterology CPT Advisors
 2014 CPT COD1NG UPDATES Gastroenterology CPT Advisors Joel V. Brill, MD, AGA CPT Advisor Daniel C. DeMarco, MD, ACG CPT Advisor Glenn D. Littenberg, MD, ASGE CPT Advisor The American College of Gastroenterology
2014 CPT COD1NG UPDATES Gastroenterology CPT Advisors Joel V. Brill, MD, AGA CPT Advisor Daniel C. DeMarco, MD, ACG CPT Advisor Glenn D. Littenberg, MD, ASGE CPT Advisor The American College of Gastroenterology
COM Compliance Policy No. 3
 COM Compliance Policy No. 3 THE UNIVERSITY OF ILLINOIS AT CHICAGO NO.: 3 UIC College of Medicine DATE: 8/5/10 Chicago, Illinois PAGE: 1of 7 UNIVERSITY OF ILLINOIS COLLEGE OF MEDICINE CODING AND DOCUMENTATION
COM Compliance Policy No. 3 THE UNIVERSITY OF ILLINOIS AT CHICAGO NO.: 3 UIC College of Medicine DATE: 8/5/10 Chicago, Illinois PAGE: 1of 7 UNIVERSITY OF ILLINOIS COLLEGE OF MEDICINE CODING AND DOCUMENTATION
How to Effectively Code for Endoscopic Procedures in Gastroenterology
 How to Effectively Code for Endoscopic Procedures in Gastroenterology Ariwan Rakvit, MD Associate Professor Interim Chief, Division of Gastroenterology Texas Tech University Health Science Center All rights
How to Effectively Code for Endoscopic Procedures in Gastroenterology Ariwan Rakvit, MD Associate Professor Interim Chief, Division of Gastroenterology Texas Tech University Health Science Center All rights
Billing and Claim Billing and Claim Submission Boot Camp Submission Boot Camp Beverly Remm Beverly Remm
 Billing and Claim Submission Boot Camp Presented by: Beverly Remm Orion Healthcare Technology Billing and Claim Submission Boot Camp Presented by: Beverly Remm Orion Healthcare Technology The presentation
Billing and Claim Submission Boot Camp Presented by: Beverly Remm Orion Healthcare Technology Billing and Claim Submission Boot Camp Presented by: Beverly Remm Orion Healthcare Technology The presentation
LABORATORY and PATHOLOGY SERVICES
 LABORATORY and PATHOLOGY SERVICES Policy Neighborhood Health Plan reimburses participating clinical laboratory and pathology providers for tests medically necessary for the diagnosis, treatment and prevention
LABORATORY and PATHOLOGY SERVICES Policy Neighborhood Health Plan reimburses participating clinical laboratory and pathology providers for tests medically necessary for the diagnosis, treatment and prevention
FAQ for Coding Encounters in ICD 10 CM
 FAQ for Coding Encounters in ICD 10 CM Topics: Encounter for Routine Health Exams Encounter for Vaccines Follow Up Encounters Coding for Injuries Encounter for Suture Removal External Cause Codes Tobacco
FAQ for Coding Encounters in ICD 10 CM Topics: Encounter for Routine Health Exams Encounter for Vaccines Follow Up Encounters Coding for Injuries Encounter for Suture Removal External Cause Codes Tobacco
2014 Procedural Reimbursement Guide for Endoscopy
 2014 Procedural Reimbursement Guide for Endoscopy 2014 Procedural Reimbursement Guide For THIS PROCEDURAL REIMBURSEMENT GUIDE, FOR SELECT ENDOSCOPY PROCEDURES, provides coding and reimbursement information
2014 Procedural Reimbursement Guide for Endoscopy 2014 Procedural Reimbursement Guide For THIS PROCEDURAL REIMBURSEMENT GUIDE, FOR SELECT ENDOSCOPY PROCEDURES, provides coding and reimbursement information
professional billing module
 professional billing module Professional CMS-1500 Billing Module Coding Requirements...2 Evaluation and Management Services...2 Diagnosis...2 Procedures...2 Basic Rules...3 Before You Begin...3 Modifiers...3
professional billing module Professional CMS-1500 Billing Module Coding Requirements...2 Evaluation and Management Services...2 Diagnosis...2 Procedures...2 Basic Rules...3 Before You Begin...3 Modifiers...3
Modifier -52 Reduced Services
 Manual: Policy Title: Reimbursement Policy Modifier -52 Reduced Services Section: Administrative Subsection: Policy Number: RPM 003 Date of Origin: Insert date approved Last Updated: same IMPORTANT STATEMENT
Manual: Policy Title: Reimbursement Policy Modifier -52 Reduced Services Section: Administrative Subsection: Policy Number: RPM 003 Date of Origin: Insert date approved Last Updated: same IMPORTANT STATEMENT
BCBSKS Billing Guidelines. For. Home Health Agencies
 BCBSKS Billing Guidelines For Home Health Agencies BCBSKS IPM BCBSKS Home Health Agency Manual -1 TABLE OF CONTENTS I. Overview II. General Guidelines III. Case Management IV. Home Care Benefits V. Covered
BCBSKS Billing Guidelines For Home Health Agencies BCBSKS IPM BCBSKS Home Health Agency Manual -1 TABLE OF CONTENTS I. Overview II. General Guidelines III. Case Management IV. Home Care Benefits V. Covered
Questions & Answers on ACA Section 4106 Improving Access to Preventive Services for Eligible Adults in Medicaid
 Questions & Answers on ACA Section 4106 Improving Access to Preventive Services for Eligible Adults in Medicaid STATE PLAN AMENDMENT (SPA) Q1. Can a state submit a SPA to implement section 4106 at any
Questions & Answers on ACA Section 4106 Improving Access to Preventive Services for Eligible Adults in Medicaid STATE PLAN AMENDMENT (SPA) Q1. Can a state submit a SPA to implement section 4106 at any
CENTRAL MICHIGAN UNIVERSITY - Premier Plan (PPO1) 007000285-0002 0004 Effective Date: July 1, 2015 Benefits-at-a-Glance
 CENTRAL MICHIGAN UNIVERSITY - Premier Plan (PPO1) 007000285-0002 0004 Effective Date: July 1, 2015 Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only a general overview
CENTRAL MICHIGAN UNIVERSITY - Premier Plan (PPO1) 007000285-0002 0004 Effective Date: July 1, 2015 Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only a general overview
My Coding Connection, LLC 618-530-1196. 24 Unrelated E/M by the same physician during a postoperative period
 MODIFIERS Rachel Coon, CCS-P, CPC, CPC-P, CPMA, CPC-I, CEMC, ICD-10 My Coding Connection, LLC 618-530-1196 GLOBAL PACKAGE MODIFIERS 24 Unrelated E/M by the same physician during a postoperative period
MODIFIERS Rachel Coon, CCS-P, CPC, CPC-P, CPMA, CPC-I, CEMC, ICD-10 My Coding Connection, LLC 618-530-1196 GLOBAL PACKAGE MODIFIERS 24 Unrelated E/M by the same physician during a postoperative period
Aetna Life Insurance Company
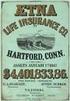 Aetna Life Insurance Company Hartford, Connecticut 06156 Amendment Policyholder: Group Policy No.: Effective Date: UNIVERSITY OF PENNSYLVANIA POSTDOCTORAL INSURANCE PLAN GP-861472 This Amendment is effective
Aetna Life Insurance Company Hartford, Connecticut 06156 Amendment Policyholder: Group Policy No.: Effective Date: UNIVERSITY OF PENNSYLVANIA POSTDOCTORAL INSURANCE PLAN GP-861472 This Amendment is effective
New Medicare Preventive
 New Medicare Preventive Services Screening Tests You Can Perform in the Office Charles B. Root, PhD Medicare is finally getting serious about preventive services. Until now, the limited preventive testing
New Medicare Preventive Services Screening Tests You Can Perform in the Office Charles B. Root, PhD Medicare is finally getting serious about preventive services. Until now, the limited preventive testing
Coverage Analysis: The Cornerstone of Clinical Research Billing Presented by: Mary L. Veazie, CPA, MBA, CHC, CHRC Executive Director, Clinical
 Coverage Analysis: The Cornerstone of Clinical Research Billing Presented by: Mary L. Veazie, CPA, MBA, CHC, CHRC Executive Director, Clinical Research Finance The University of Texas MD Anderson Cancer
Coverage Analysis: The Cornerstone of Clinical Research Billing Presented by: Mary L. Veazie, CPA, MBA, CHC, CHRC Executive Director, Clinical Research Finance The University of Texas MD Anderson Cancer
Federally Qualified Health Center Billing (100)
 1. As a federally qualified health center (FQHC) can we bill for a license medical social worker? The core practitioner must be a licensed or certified clinical social worker (CSW) in your state. Unless
1. As a federally qualified health center (FQHC) can we bill for a license medical social worker? The core practitioner must be a licensed or certified clinical social worker (CSW) in your state. Unless
Initial Preventive Physical Examination
 Initial Preventive Physical Examination Overview The Medicare Prescription Drug, Improvement, and Modernization Act (MMA) of 2003 expanded Medicare's coverage of preventive services. Central to the Centers
Initial Preventive Physical Examination Overview The Medicare Prescription Drug, Improvement, and Modernization Act (MMA) of 2003 expanded Medicare's coverage of preventive services. Central to the Centers
National PPO 1000. PPO Schedule of Payments (Maryland Small Group)
 PPO Schedule of Payments (Maryland Small Group) National PPO 1000 The benefits outlined in this Schedule are in addition to the benefits offered under Coventry Health & Life Insurance Company Small Employer
PPO Schedule of Payments (Maryland Small Group) National PPO 1000 The benefits outlined in this Schedule are in addition to the benefits offered under Coventry Health & Life Insurance Company Small Employer
Medicare Preventive Services National Provider Call: The Initial Preventive Physical Exam and the Annual Wellness Visit.
 Medicare Preventive Services National Provider Call: The Initial Preventive Physical Exam and the Annual Wellness Visit March 28, 2012 1 Today s Panel of Experts Jamie Hermansen Health Insurance Specialist
Medicare Preventive Services National Provider Call: The Initial Preventive Physical Exam and the Annual Wellness Visit March 28, 2012 1 Today s Panel of Experts Jamie Hermansen Health Insurance Specialist
Section 9. Claims Claim Submission Molina Healthcare PO Box 22815 Long Beach, CA 90801
 Section 9. Claims As a contracted provider, it is important to understand how the claims process works to avoid delays in processing your claims. The following items are covered in this section for your
Section 9. Claims As a contracted provider, it is important to understand how the claims process works to avoid delays in processing your claims. The following items are covered in this section for your
The ABCs of the Initial Preventive Physical Exam and the Annual Wellness Visit. National Provider Call July 21, 2011
 The ABCs of the Initial Preventive Physical Exam and the Annual Wellness Visit National Provider Call July 21, 2011 1 Today s Panel of Experts Jamie Hermansen Health Insurance Specialist Coverage & Analysis
The ABCs of the Initial Preventive Physical Exam and the Annual Wellness Visit National Provider Call July 21, 2011 1 Today s Panel of Experts Jamie Hermansen Health Insurance Specialist Coverage & Analysis
Medical, Surgical, and Routine Supplies (including but not limited to 99070)
 Manual: Policy Title: Reimbursement Policy Medical, Surgical, and Routine Supplies (including but not limited to 99070) Section: Administrative Subsection: none Date of Origin: 1/1/2002 Policy Number:
Manual: Policy Title: Reimbursement Policy Medical, Surgical, and Routine Supplies (including but not limited to 99070) Section: Administrative Subsection: none Date of Origin: 1/1/2002 Policy Number:
Risk Adjustment/HCC Coding and Documentation
 Manual: Policy Title: Reimbursement Policy Risk Adjustment/HCC Coding and Documentation Section: Administrative Subsection: None Date of Origin: 1/2/2013 Policy Number: RPM050 Last Updated: 6/8/2016 Last
Manual: Policy Title: Reimbursement Policy Risk Adjustment/HCC Coding and Documentation Section: Administrative Subsection: None Date of Origin: 1/2/2013 Policy Number: RPM050 Last Updated: 6/8/2016 Last
There are two levels of modifiers: Level 1 (CPT) and Level II (CMS, also known as HCPCS).
 PROVIDER BILLING GUIDELINES Modifiers Modifiers are two digit or alphanumeric characters that are appended to CPT and HCPCS codes. The modifier allows the provider to indicate that a procedure was affected
PROVIDER BILLING GUIDELINES Modifiers Modifiers are two digit or alphanumeric characters that are appended to CPT and HCPCS codes. The modifier allows the provider to indicate that a procedure was affected
Health First Billing Guideline
 Subject: Preventive Services Health First Billing Guideline Effective: January 1, 2013 Last Updated: December 2013 Background: Health First is committed to the wellness of its members and encourages preventive
Subject: Preventive Services Health First Billing Guideline Effective: January 1, 2013 Last Updated: December 2013 Background: Health First is committed to the wellness of its members and encourages preventive
CODING. Neighborhood Health Plan 1 Provider Payment Guidelines
 CODING Policy The terms of this policy set forth the guidelines for reporting the provision of care rendered by NHP participating providers, including but not limited to use of standard diagnosis and procedure
CODING Policy The terms of this policy set forth the guidelines for reporting the provision of care rendered by NHP participating providers, including but not limited to use of standard diagnosis and procedure
FEATURES NETWORK OUT-OF-NETWORK
 Schedule of Benefits Employer: The Vanguard Group, Inc. ASA: 697478-A Issue Date: January 1, 2014 Effective Date: January 1, 2014 Schedule: 3B Booklet Base: 3 For: Choice POS II - 950 Option - Retirees
Schedule of Benefits Employer: The Vanguard Group, Inc. ASA: 697478-A Issue Date: January 1, 2014 Effective Date: January 1, 2014 Schedule: 3B Booklet Base: 3 For: Choice POS II - 950 Option - Retirees
TUTORIAL: How to Code an Emergency Department (ED) Record
 TUTORIAL: How to Code an Emergency Department (ED) Record Welcome! Assigning ICD-10-CM codes to diagnoses and CPT/HCPCS Level II codes to procedures/services for emergency department office records can
TUTORIAL: How to Code an Emergency Department (ED) Record Welcome! Assigning ICD-10-CM codes to diagnoses and CPT/HCPCS Level II codes to procedures/services for emergency department office records can
University of Michigan Group: 007005187-0000, 0001 Comprehensive Major Medical (CMM) Benefits-at-a-Glance
 University of Michigan Group: 007005187-0000, 0001 Comprehensive Major Medical (CMM) Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only a general overview of your benefits.
University of Michigan Group: 007005187-0000, 0001 Comprehensive Major Medical (CMM) Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only a general overview of your benefits.
CONNECTIONS TESTING FOR ICD-10
 TESTING FOR ICD-10 In conjunction with the Centers for Medicare and Medicaid Services (CMS), Providence Health Plan (PHP) and all major payers will convert from International Classification of Diseases,
TESTING FOR ICD-10 In conjunction with the Centers for Medicare and Medicaid Services (CMS), Providence Health Plan (PHP) and all major payers will convert from International Classification of Diseases,
The Two Sides of Gastroenterology
 The Two Sides of Gastroenterology Jill Young, CPC, CEDC, CIMC 1 Disclaimer This material is designed to offer basic information for coding and billing. The information presented here is based on the experience,
The Two Sides of Gastroenterology Jill Young, CPC, CEDC, CIMC 1 Disclaimer This material is designed to offer basic information for coding and billing. The information presented here is based on the experience,
2006 Provider Coding/Billing Information. www.novoseven-us.com
 2006 Provider Coding/Billing Information 2 3 Contents About NovoSeven...2 Coverage...4 Coding...4 Reimbursement...8 Establishing Medical Necessity and Appealing Denied Claims...10 Claims Materials...12
2006 Provider Coding/Billing Information 2 3 Contents About NovoSeven...2 Coverage...4 Coding...4 Reimbursement...8 Establishing Medical Necessity and Appealing Denied Claims...10 Claims Materials...12
Preventive Medicine and Screening Policy
 REIMBURSEMENT POLICY Policy Number 2015R0013C Preventive Medicine and Screening Policy Annual Approval Date 3/11/2015 Approved By Payment Policy Oversight Committee IMPORTANT NOTE ABOUT THIS REIMBURSEMENT
REIMBURSEMENT POLICY Policy Number 2015R0013C Preventive Medicine and Screening Policy Annual Approval Date 3/11/2015 Approved By Payment Policy Oversight Committee IMPORTANT NOTE ABOUT THIS REIMBURSEMENT
PLAN DESIGN AND BENEFITS - Tx OAMC Basic 2500-10 PREFERRED CARE
 PLAN FEATURES Deductible (per calendar year) $2,500 Individual $4,000 Individual $7,500 Family $12,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
PLAN FEATURES Deductible (per calendar year) $2,500 Individual $4,000 Individual $7,500 Family $12,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
SMALL GROUP PLAN DESIGN AND BENEFITS OPEN CHOICE OUT-OF-STATE PPO PLAN - $1,000
 PLAN FEATURES PREFERRED CARE NON-PREFERRED CARE Deductible (per calendar year; applies to all covered services) $1,000 Individual $3,000 Family $2,000 Individual $6,000 Family Plan Coinsurance ** 80% 60%
PLAN FEATURES PREFERRED CARE NON-PREFERRED CARE Deductible (per calendar year; applies to all covered services) $1,000 Individual $3,000 Family $2,000 Individual $6,000 Family Plan Coinsurance ** 80% 60%
Understanding Coding & Reimbursement for SBI. Presented By: Jen Cohrs CPC, CPMA, CGIC Director of Educational Strategies Wisconsin Medical Society
 Understanding Coding & Reimbursement for SBI Presented By: Jen Cohrs CPC, CPMA, CGIC Director of Educational Strategies Wisconsin Medical Society CPT codes, descriptions and material only are Copyright
Understanding Coding & Reimbursement for SBI Presented By: Jen Cohrs CPC, CPMA, CGIC Director of Educational Strategies Wisconsin Medical Society CPT codes, descriptions and material only are Copyright
Section 2. Licensed Nurse Practitioner
 Section 2 Table of Contents 1 General Information... 2 1-1 General Policy... 2 1-2 Fee-For-Service or Managed Care... 2 1-3 Definitions... 2 2 Provider Participation Requirements... 3 2-1 Provider Enrollment...
Section 2 Table of Contents 1 General Information... 2 1-1 General Policy... 2 1-2 Fee-For-Service or Managed Care... 2 1-3 Definitions... 2 2 Provider Participation Requirements... 3 2-1 Provider Enrollment...
Laboratory Services Policy
 Policy Number 2014R0014F Annual Approval Date Laboratory Services Policy 1/27/2014 Approved By National Reimbursement Forum United HealthCare Community & State Payment Policy Committee IMPORTANT NOTE ABOUT
Policy Number 2014R0014F Annual Approval Date Laboratory Services Policy 1/27/2014 Approved By National Reimbursement Forum United HealthCare Community & State Payment Policy Committee IMPORTANT NOTE ABOUT
UNITED WORLD LIFE INSURANCE COMPANY OMAHA, NEBRASKA A Mutual of Omaha Company OUTLINE OF MEDICARE SUPPLEMENT COVERAGE COVER PAGE
 UNITED WORLD LIFE INSURANCE COMPANY OMAHA, NEBRASKA A Mutual of Omaha Company OUTLINE OF MEDICARE SUPPLEMENT COVERAGE COVER PAGE The Commissioner of Insurance of the State of Minnesota has established
UNITED WORLD LIFE INSURANCE COMPANY OMAHA, NEBRASKA A Mutual of Omaha Company OUTLINE OF MEDICARE SUPPLEMENT COVERAGE COVER PAGE The Commissioner of Insurance of the State of Minnesota has established
What is your level of coding experience?
 The TrustHCS Academy is dedicated to growing new coders to enter the field of medical records coding while also increasing the ICD-10 skills of seasoned coding professionals. A unique combination of on-line
The TrustHCS Academy is dedicated to growing new coders to enter the field of medical records coding while also increasing the ICD-10 skills of seasoned coding professionals. A unique combination of on-line
Routine Preventive Services. Covered by Medicare 2012
 Routine Preventive Services Covered by Medicare 2012 Brook Golshan, CPC, ACS-EM 2/20/2012 1 Preventive Services Covered by Medicare 2012 Covered by Medicare Part B: Original/Direct Medicare Most of the
Routine Preventive Services Covered by Medicare 2012 Brook Golshan, CPC, ACS-EM 2/20/2012 1 Preventive Services Covered by Medicare 2012 Covered by Medicare Part B: Original/Direct Medicare Most of the
5557 FAQs & Definitions
 5557 FAQs & Definitions These Questions and Answers are intended to present information that has been acquired as part of the discovery process and provides necessary context for the Policy Directives
5557 FAQs & Definitions These Questions and Answers are intended to present information that has been acquired as part of the discovery process and provides necessary context for the Policy Directives
Refer to https://www.bcbsal.org/providers/hcreform/hcrpreventivecod ing.pdf for the Quick Reference Guide for HCR Preventive Care Services
 Refer to https://www.bcbsal.org/providers/hcreform/hcrpreventivecod ing.pdf for the Quick Reference Guide for HCR Preventive Care Services Name of Policy: Preventive Care Services under Health Care Reform
Refer to https://www.bcbsal.org/providers/hcreform/hcrpreventivecod ing.pdf for the Quick Reference Guide for HCR Preventive Care Services Name of Policy: Preventive Care Services under Health Care Reform
Empire BlueCross BlueShield Professional Reimbursement Policy
 Subject: Evaluation and Management Services and Related Modifiers -25 & 57 NY Policy: 0026 Effective: 8/19/2013 1/31/2014 Coverage is subject to the terms, conditions, and limitations of an individual
Subject: Evaluation and Management Services and Related Modifiers -25 & 57 NY Policy: 0026 Effective: 8/19/2013 1/31/2014 Coverage is subject to the terms, conditions, and limitations of an individual
Reimbursement Questions and Answers for IBCLCs Judith L. Gutowski, BA, IBCLC, RLC Chair, USLCA Licensure and Reimbursement Committee June 2012
 Reimbursement Questions and Answers for IBCLCs Judith L. Gutowski, BA, IBCLC, RLC Chair, USLCA Licensure and Reimbursement Committee June 2012 The USLCA often receives inquiries about insurance and Medicaid
Reimbursement Questions and Answers for IBCLCs Judith L. Gutowski, BA, IBCLC, RLC Chair, USLCA Licensure and Reimbursement Committee June 2012 The USLCA often receives inquiries about insurance and Medicaid
Glossary of Frequently Used Billing and Coding Terms
 Glossary of Frequently Used Billing and Coding Terms Accountable Care Organization (ACO) Accounts Receivable Reports All Inclusive Fees Allowances and Adjustments Capitation Payments Care Coordination
Glossary of Frequently Used Billing and Coding Terms Accountable Care Organization (ACO) Accounts Receivable Reports All Inclusive Fees Allowances and Adjustments Capitation Payments Care Coordination
PROTOCOLS FOR PHYSICAL THERAPY PROVIDERS
 PROTOCOLS FOR PHYSICAL THERAPY PROVIDERS A Member may access Physical Therapy services (PT) when treatment is prescribed by a physician to restore or improve a person s ability to undertake activities
PROTOCOLS FOR PHYSICAL THERAPY PROVIDERS A Member may access Physical Therapy services (PT) when treatment is prescribed by a physician to restore or improve a person s ability to undertake activities
STANDARD AND SELECT NETWORK PRODUCTS FROM TUFTS HEALTH PLAN
 STANDARD AND SELECT NETWORK PRODUCTS FROM TUFTS HEALTH PLAN 2015 PLAN OPTIONS Standard Network: The Standard Network plans provide members with a choice of more than 25,000 participating doctors and 90
STANDARD AND SELECT NETWORK PRODUCTS FROM TUFTS HEALTH PLAN 2015 PLAN OPTIONS Standard Network: The Standard Network plans provide members with a choice of more than 25,000 participating doctors and 90
istent Trabecular Micro-Bypass Stent Reimbursement Guide
 istent Trabecular Micro-Bypass Stent Reimbursement Guide Table of Contents Overview Coding 3 4 Coding Overview Procedure Coding Device Coding Additional Coding Information Coverage Payment 10 11 Payment
istent Trabecular Micro-Bypass Stent Reimbursement Guide Table of Contents Overview Coding 3 4 Coding Overview Procedure Coding Device Coding Additional Coding Information Coverage Payment 10 11 Payment
Procedures for Coding Inpatient Medical Record Cases for the CCS Examination
 Procedures for Coding Inpatient Medical Record Cases for the CCS Examination Instructions and official guidelines for coding medical records are included in the following resources: ICD-10-CM/PCS, CPT,
Procedures for Coding Inpatient Medical Record Cases for the CCS Examination Instructions and official guidelines for coding medical records are included in the following resources: ICD-10-CM/PCS, CPT,
Section: Administrative Subsection: None Date of Origin: 7/25/2011 Policy Number: RPM040 Last Updated: 11/6/2014 Last Reviewed: 11/11/2015
 Manual: Policy Title: Reimbursement Policy Incident-To Services Section: Administrative Subsection: None Date of Origin: 7/25/2011 Policy Number: RPM040 Last Updated: 11/6/2014 Last Reviewed: 11/11/2015
Manual: Policy Title: Reimbursement Policy Incident-To Services Section: Administrative Subsection: None Date of Origin: 7/25/2011 Policy Number: RPM040 Last Updated: 11/6/2014 Last Reviewed: 11/11/2015
Gone are the days when healthy
 Five Common Coding Mistakes That Are Costing You Fix these problems to increase your bottom line. GREG CLARKE Emily Hill, PA-C Gone are the days when healthy third-party reimbursements meant practices
Five Common Coding Mistakes That Are Costing You Fix these problems to increase your bottom line. GREG CLARKE Emily Hill, PA-C Gone are the days when healthy third-party reimbursements meant practices
NOVOSTE BETA-CATH SYSTEM
 HOSPITAL INPATIENT AND OUTPATIENT BILLING GUIDE FOR THE NOVOSTE BETA-CATH SYSTEM INTRAVASCULAR BRACHYTHERAPY DEVICE This guide is intended solely for use as a tool to help hospital billing staff resolve
HOSPITAL INPATIENT AND OUTPATIENT BILLING GUIDE FOR THE NOVOSTE BETA-CATH SYSTEM INTRAVASCULAR BRACHYTHERAPY DEVICE This guide is intended solely for use as a tool to help hospital billing staff resolve
UnitedHealthcare Choice Plus. UnitedHealthcare Insurance Company. Certificate of Coverage
 UnitedHealthcare Choice Plus UnitedHealthcare Insurance Company Certificate of Coverage For the Plan 7EG of Educators Benefit Services, Inc. Enrolling Group Number: 717578 Effective Date: January 1, 2012
UnitedHealthcare Choice Plus UnitedHealthcare Insurance Company Certificate of Coverage For the Plan 7EG of Educators Benefit Services, Inc. Enrolling Group Number: 717578 Effective Date: January 1, 2012
UnitedHealthcare Choice Plus. UnitedHealthcare Insurance Company. Certificate of Coverage
 UnitedHealthcare Choice Plus UnitedHealthcare Insurance Company Certificate of Coverage For the Health Savings Account (HSA) Plan 7PD of Educators Benefit Services, Inc. Enrolling Group Number: 717578
UnitedHealthcare Choice Plus UnitedHealthcare Insurance Company Certificate of Coverage For the Health Savings Account (HSA) Plan 7PD of Educators Benefit Services, Inc. Enrolling Group Number: 717578
UNITED TEACHER ASSOCIATES INSURANCE COMPANY P.O. Box 26580 Austin, Texas 78755-0580 (800) 880-8824
 UNITED TEACHER ASSOCIATES INSURANCE COMPANY P.O. Box 26580 Austin, Texas 78755-0580 (800) 880-8824 OUTLINE OF MEDICARE SUPPLEMENT COVERAGE - COVER PAGE BASIC AND EXTENDED BASIC PLANS The Commissioner of
UNITED TEACHER ASSOCIATES INSURANCE COMPANY P.O. Box 26580 Austin, Texas 78755-0580 (800) 880-8824 OUTLINE OF MEDICARE SUPPLEMENT COVERAGE - COVER PAGE BASIC AND EXTENDED BASIC PLANS The Commissioner of
istent Trabecular Micro-Bypass Stent Reimbursement Guide
 istent Trabecular Micro-Bypass Stent Reimbursement Guide Table of Contents Overview Coding 2 3 Coding Overview Procedure Coding Device Coding Additional Coding Information Coverage Payment 8 9 Payment
istent Trabecular Micro-Bypass Stent Reimbursement Guide Table of Contents Overview Coding 2 3 Coding Overview Procedure Coding Device Coding Additional Coding Information Coverage Payment 8 9 Payment
WELLCARE CLAIM PAYMENT POLICIES
 WellCare and Harmony Health Plan s claim payment policies are based on publicly distributed guidelines from established industry sources such as the Centers for Medicare and Medicaid Services (CMS), the
WellCare and Harmony Health Plan s claim payment policies are based on publicly distributed guidelines from established industry sources such as the Centers for Medicare and Medicaid Services (CMS), the
Reimbursement Rules That Could Trip Up Hospital Attorneys THEMES
 Reimbursement Rules That Could Trip Up Hospital Attorneys Cynthia F. Wisner Associate Counsel, Trinity Health 1 THEMES Medicare is eliminating grandfathering and bundling payments Lab technical fees 3
Reimbursement Rules That Could Trip Up Hospital Attorneys Cynthia F. Wisner Associate Counsel, Trinity Health 1 THEMES Medicare is eliminating grandfathering and bundling payments Lab technical fees 3
Consumer Guide to. Health Insurance. Oregon Insurance Division
 Consumer Guide to Health Insurance Oregon Insurance Division The Department of Consumer and Business Services, Oregon s largest business regulatory and consumer protection agency, produced this guide.
Consumer Guide to Health Insurance Oregon Insurance Division The Department of Consumer and Business Services, Oregon s largest business regulatory and consumer protection agency, produced this guide.
Article from: Health Section News. October 2002 Issue No. 44
 Article from: Health Section News October 2002 Issue No. 44 Outpatient Facility Reimbursement by Brian G. Small Outpatient Charge Levels Today s outpatient care can be every bit as intense and expensive
Article from: Health Section News October 2002 Issue No. 44 Outpatient Facility Reimbursement by Brian G. Small Outpatient Charge Levels Today s outpatient care can be every bit as intense and expensive
PLAN DESIGN AND BENEFITS POS Open Access Plan 1944
 PLAN FEATURES PARTICIPATING Deductible (per calendar year) $3,000 Individual $9,000 Family $4,000 Individual $12,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being
PLAN FEATURES PARTICIPATING Deductible (per calendar year) $3,000 Individual $9,000 Family $4,000 Individual $12,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being
PLAN DESIGN AND BENEFITS - Tx OAMC 1500-10 PREFERRED CARE
 PLAN FEATURES Deductible (per calendar year) $1,500 Individual $3,000 Individual $4,500 Family $9,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
PLAN FEATURES Deductible (per calendar year) $1,500 Individual $3,000 Individual $4,500 Family $9,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
Inpatient or Outpatient Only: Why Observation Has Lost Its Status
 Inpatient or Outpatient Only: Why Observation Has Lost Its Status W h i t e p a p e r Proper patient status classification affects the clinical and financial success of hospitals. Unfortunately, assigning
Inpatient or Outpatient Only: Why Observation Has Lost Its Status W h i t e p a p e r Proper patient status classification affects the clinical and financial success of hospitals. Unfortunately, assigning
Compensation and Claims Processing
 Compensation and Claims Processing Compensation The network rate for eligible outpatient visits is reimbursed to you at the lesser of (1) your customary charge, less any applicable co-payments, coinsurance
Compensation and Claims Processing Compensation The network rate for eligible outpatient visits is reimbursed to you at the lesser of (1) your customary charge, less any applicable co-payments, coinsurance
Medicare Claims Benefit Manual Chapter 15 Covered Medical and Other Health Services Incident To
 Medicare Claims Benefit Manual Chapter 15 Covered Medical and Other Health Services Incident To Revision Date 11/18/11 60 - Services and Supplies 60.1 - Incident To Physician s Professional Services 60.2
Medicare Claims Benefit Manual Chapter 15 Covered Medical and Other Health Services Incident To Revision Date 11/18/11 60 - Services and Supplies 60.1 - Incident To Physician s Professional Services 60.2
Title: Coding and Documentation for Inpatient Services
 Title: Coding and Documentation for Effective Date: 2/01; Rev. 6/03, 7/05 POLICY: Diagnoses and procedures will be coded utilizing the International Classification of Diseases, Ninth Revision, Clinical
Title: Coding and Documentation for Effective Date: 2/01; Rev. 6/03, 7/05 POLICY: Diagnoses and procedures will be coded utilizing the International Classification of Diseases, Ninth Revision, Clinical
CPT Coding in Oral Medicine
 CPT Coding in Oral Medicine CPT - Current Procedural Terminology Medical Code Set (00000-99999) Established as an indexing/coding system to standardize terminology among physicians and other providers
CPT Coding in Oral Medicine CPT - Current Procedural Terminology Medical Code Set (00000-99999) Established as an indexing/coding system to standardize terminology among physicians and other providers
Wellness Exam Coverage Highlights
 The following Medicare Advantage plans have updated coding procedures for 2013: AARP MedicareComplete UnitedHealthcare MedicareComplete UnitedHealthcare Dual Complete UnitedHealthcare MedicareDirect Wellness
The following Medicare Advantage plans have updated coding procedures for 2013: AARP MedicareComplete UnitedHealthcare MedicareComplete UnitedHealthcare Dual Complete UnitedHealthcare MedicareDirect Wellness
LABORATORY COMPLIANCE AND MEDICAL NECESSITY
 LABORATORY COMPLIANCE AND MEDICAL NECESSITY Jump to: Medical Necessity Local/National Coverage Determinations Advance Beneficiary Notice (ABN) ABN Form in English ABN Form in Spanish Annual Physician Notification
LABORATORY COMPLIANCE AND MEDICAL NECESSITY Jump to: Medical Necessity Local/National Coverage Determinations Advance Beneficiary Notice (ABN) ABN Form in English ABN Form in Spanish Annual Physician Notification
Schedule of Benefits HARVARD PILGRIM LAHEY HEALTH VALUE HMO MASSACHUSETTS MEMBER COST SHARING
 Schedule of s HARVARD PILGRIM LAHEY HEALTH VALUE HMO MASSACHUSETTS ID: MD0000003378_ X Please Note: In this plan, Members have access to network benefits only from the providers in the Harvard Pilgrim-Lahey
Schedule of s HARVARD PILGRIM LAHEY HEALTH VALUE HMO MASSACHUSETTS ID: MD0000003378_ X Please Note: In this plan, Members have access to network benefits only from the providers in the Harvard Pilgrim-Lahey
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Appendix A. Prepared Exclusively for The Dow Chemical Company
 Appendix A BENEFIT PLAN Prepared Exclusively for The Dow Chemical Company What Your Plan Covers and How Benefits are Paid Choice POS II (MAP Plus Option 2 - High Deductible Health Plan (HDHP) with Prescription
Appendix A BENEFIT PLAN Prepared Exclusively for The Dow Chemical Company What Your Plan Covers and How Benefits are Paid Choice POS II (MAP Plus Option 2 - High Deductible Health Plan (HDHP) with Prescription
Physician Fee Schedule BCBSRI follows CMS Physician Fee Schedule (PFS) Relative Value Units (RVU) for details relating to
 Policy Coding and Guidelines EFFECTIVE DATE: 09 01 2015 POLICY LAST UPDATED: 09 02 2015 OVERVIEW This Policy provides an overview of coding and guidelines as they pertain to claims submitted to Blue Cross
Policy Coding and Guidelines EFFECTIVE DATE: 09 01 2015 POLICY LAST UPDATED: 09 02 2015 OVERVIEW This Policy provides an overview of coding and guidelines as they pertain to claims submitted to Blue Cross
CLAIM FORM REQUIREMENTS
 CLAIM FORM REQUIREMENTS When billing for services, please pay attention to the following points: Submit claims on a current CMS 1500 or UB04 form. Please include the following information: 1. Patient s
CLAIM FORM REQUIREMENTS When billing for services, please pay attention to the following points: Submit claims on a current CMS 1500 or UB04 form. Please include the following information: 1. Patient s
ICD-10 Frequently Asked Questions For Providers
 ICD-10 Frequently Asked Questions For Providers ICD-10 Basics ICD-10 Coding and Claims ICD-10 s ICD-10 Testing ICD-10 Resources ICD-10 Basics What is ICD-10? International Classification of Diseases, 10th
ICD-10 Frequently Asked Questions For Providers ICD-10 Basics ICD-10 Coding and Claims ICD-10 s ICD-10 Testing ICD-10 Resources ICD-10 Basics What is ICD-10? International Classification of Diseases, 10th
Premera Blue Cross Medicare Advantage Provider Reference Manual
 Premera Blue Cross Medicare Advantage Provider Reference Manual Introduction to Premera Blue Cross Medicare Advantage Plans Premera Blue Cross offers Medicare Advantage (MA) plans in King, Pierce, Snohomish,
Premera Blue Cross Medicare Advantage Provider Reference Manual Introduction to Premera Blue Cross Medicare Advantage Plans Premera Blue Cross offers Medicare Advantage (MA) plans in King, Pierce, Snohomish,
