AETNA HEALTH OF UTAH INC. (IDAHO) CERTIFICATE OF COVERAGE In-network and out-of-network coverage under the Aetna Peak Preference plan
|
|
|
- Camilla Fox
- 7 years ago
- Views:
Transcription
1 Plan Name: ID Bronze Peak Pref HNOpt /55/40 HSA IDO AETNA HEALTH OF UTAH INC. (IDAHO) CERTIFICATE OF COVERAGE In-network and out-of-network coverage under the Aetna Peak Preference plan This Certificate of Coverage ("Certificate") is part of the Group Agreement ("Group Agreement") between Aetna Health of Utah Inc., hereinafter referred to as Aetna, and the Contract Holder. The Group Agreement determines the terms and conditions of coverage. The Certificate describes covered health care benefits. Provisions of this Certificate include the Schedule of Benefits, and any amendments, endorsements, inserts, or attachments. Amendments, endorsements, inserts, or attachments may be delivered with the Certificate or added thereafter. Coverage is not provided for any services received before coverage starts or after coverage ends, except as shown in the Continuation and Conversion section of this Certificate. Certain words have specific meanings when used in this Certificate. The defined terms appear in bold type with initial capital letters. The definitions of those terms are found in the Definitions section of this Certificate. This Certificate is not in lieu of insurance for Workers Compensation. This Certificate is governed by applicable federal law and the laws of. Coverage under this plan is non-occupational. Only non-occupational injuries and non-occupational illnesses are covered under this plan. If you are an owner of the company that applied for coverage under this plan and no other sources of coverage or reimbursement are available to you for the services or supplies, then you will also be covered for occupational injuries and occupational illnesses. Other sources of coverage or reimbursement may include workers compensation, or an occupational illness or similar program under local, state or federal law. A source of coverage or reimbursement will be considered available to you even if you waived your right to payment from that source. If you are also covered under a workers compensation law or similar law, and submit proof that you are not covered for a particular illness or injury under such law, that illness or injury will be considered non-occupational regardless of cause. READ THIS ENTIRE CERTIFICATE CAREFULLY. IT DESCRIBES THE RIGHTS AND OBLIGATIONS OF MEMBERS AND AETNA. IT IS THE CONTRACT HOLDER S AND THE MEMBER'S RESPONSIBILITY TO UNDERSTAND THE TERMS AND CONDITIONS IN THIS CERTIFICATE. IN SOME CIRCUMSTANCES, CERTAIN MEDICAL SERVICES ARE NOT COVERED OR MAY REQUIRE PRECERTIFICATION BY AETNA. NO SERVICES ARE COVERED UNDER THIS CERTIFICATE IN THE ABSENCE OF PAYMENT OF CURRENT PREMIUMS SUBJECT TO THE GRACE PERIOD AND THE PREMIUMS SECTION OF THE GROUP AGREEMENT. ID-SG-COC-PP SG Off Exchange
2 THIS CERTIFICATE APPLIES TO COVERAGE ONLY AND DOES NOT RESTRICT A MEMBER S ABILITY TO RECEIVE HEALTH CARE SERVICES THAT ARE NOT, OR MIGHT NOT BE, COVERED BENEFITS UNDER THIS CERTIFICATE. PARTICIPATING PROVIDERS, NON-PARTICIPATING PROVIDERS, INSTITUTIONS, FACILITIES OR AGENCIES ARE NEITHER AGENTS NOR EMPLOYEES OF AETNA. Important Unless otherwise specifically provided, no Member has the right to receive the benefits of this plan for health care services or supplies furnished following termination of coverage. Benefits of this plan are available only for services or supplies furnished during the term the coverage is in effect and while the individual claiming the benefits is actually covered by the Group Agreement. Benefits may be modified during the term of this plan as specifically provided under the terms of the Group Agreement or upon renewal. If benefits are modified, the revised benefits (including any reduction in benefits or elimination of benefits) apply for services or supplies furnished on or after the effective date of the modification. There is no vested right to receive the benefits of the Group Agreement. Edward C Lee Vice President and Secretary HO SG2015COC 01 2 SG Off Exchange
3 TABLE OF CONTENTS Section Page Aetna Procedure 4 Eligibility and Enrollment 8 Covered Benefits 13 Exclusions and Limitations 55 Termination of Coverage 70 Continuation and Conversion 71 Claim Procedures/Complaints and Appeals 73 /Dispute Resolution Coordination of Benefits 81 Subrogation and Right of Recovery 81 Responsibility of Members 86 General Provisions 87 Definitions 91 HO SG2015COC 01 3 SG Off Exchange
4 AETNA PROCEDURE This Plan provides coverage for medical expenses for the treatment of illness or injury. It does not provide benefits for all medical care. The plan also provides coverage for certain preventive and wellness benefits. The Aetna Peak Preference plan offers you a unique opportunity to choose your benefit level at the time you select your provider. You will notice in the Peak Preference Provider Directory that every provider listed has a designation of Level 1 or 2 participating benefit plus a non-participating provider benefit. Availability of Level 1 providers may vary based on geographic location. Levels and corresponding benefit amounts are indicated in your medical benefits brochure When you go to a provider, your claim will be processed according to the benefit indicated by that provider s Level, as listed in the Peak Preference Provider Directory. For example, if you visit a physician designated as a Level 1 provider, Level 1 benefits will apply. When you choose to access your non-participating option, you continue to have comprehensive benefits but with higher out-of-pocket expenses. When you receive services from non-participating providers and facilities, you are responsible for your copay, coinsurance, and deductible expenses plus any costs above your eligible medical expenses. If your non-participating provider s charges exceed your eligible medical expenses, your provider may ask you to pay those additional charges. Important Note: Network providers have contracted with Aetna, an affiliate or third party vendor to provide health care services and supplies to Aetna plan members. Network providers are generally identified in the printed directory and the on-line version of the provider Directory you can find this information on DocFind on or by calling the number on your identification card. Out-of-network providers are not listed in the Aetna directory. Selecting a Participating Primary Care Physician At the time of enrollment, each Member must choose to select a Primary Care Physician (PCP) that is a Participating Provider from Aetna s Directory of Participating Providers to access Covered Benefits as described in this Contract. The choice of a PCP is made solely by the Member. If the Member is a minor or otherwise incapable of selecting a PCP, the Subscriber should select a PCP on the Member s behalf. You can select a PCP from one of the following specialties: Family Practice, Internal Medicine, General Practice, Obstetrics/Gynecology (OB/GYN), or Pediatrics. Although an OB/GYN may be considered a PCP, many OB/GYN physicians choose not to provide primary care. If you want an OB/GYN as your PCP, ask that Provider if he or she provides primary care services. The Primary Care Physician The PCP coordinates a Member's medical care, as appropriate, either by providing treatment or may direct the Member to other Participating Providers. The PCP can also order lab tests and x-rays, prescribe medicines or therapies, and arrange hospitalization. HO SG2015COC 01 4 SG Off Exchange
5 The PCP provides services for the treatment of routine illnesses, injuries, well baby and preventive care services which do not require the services of a Specialist, and for non-office hour Urgent Care services under this plan. The Member s selected PCP or that PCP s covering Physician is required to be available 7 days a week, 24 hours a day for Urgent Care services. A Member will be subject to the PCP Copayment listed on the Schedule of Benefits when a Member obtains Covered Benefits from any Participating PCP. Participating Providers can only bill for the deductible, copayment, and coinsurance. Certain PCP offices are affiliated with integrated delivery systems or other provider groups (i.e., Independent Practice Associations and Physician-Hospital Organizations), and Members who select these PCPs will generally be referred to Specialists and Hospitals within that system or group. However, if the group does not include a Provider qualified to meet the Member s medical needs, the Member may request to have services provided by nonaffiliated Providers. Availability of Providers Aetna cannot guarantee the availability or continued participation of a particular Provider. Either Aetna or any Participating Provider may terminate the Provider contract or limit the number of Members that will be accepted as patients. If the PCP initially selected cannot accept additional patients, the Member will be notified and given an opportunity to make another PCP selection. The Member must then cooperate with Aetna to select another PCP. Until a PCP is selected, benefits are limited to coverage for Medical Emergency care. Changing a PCP You may change your PCP at any time by calling Member Services at the toll-free telephone number listed on the Member s identification card or by written or electronic submission of the Aetna s change form. A Member may contact Aetna to request a change form or for assistance in completing that form. The change will become effective upon Aetna s receipt and approval of the request. Ongoing Reviews Aetna conducts ongoing reviews of those services and supplies which are recommended or provided by Health Professionals to determine whether such services and supplies are Covered Benefits under this Certificate. If Aetna determines that the recommended services and supplies are not Covered Benefits, the Member will be notified. If a Member wishes to appeal such determination, the Member may then contact Aetna to seek a review of the determination. Please refer to the Claim Procedures/Complaints and Appeals/Dispute Resolution section of this Certificate. Precertification Certain services and supplies under this Certificate may require precertification by Aetna to determine if they are Covered Benefits under this Certificate. HO SG2015COC 01 5 SG Off Exchange
6 Certain services, such as inpatient stays, require Precertification by Aetna. Precertification is a process that helps you and your Physician determine whether the services being recommended are Covered Benefits under the plan. It also allows Aetna to help your Provider coordinate your transition from an inpatient setting to an outpatient setting (called discharge planning), and to register you for specialized programs or case management when appropriate. You do not need to precertify services provided by a participating provider. Participating providers will be responsible for obtaining necessary precertification for you. Since precertification is the provider s responsibility, there is no additional out-of-pocket cost to you as a result of a participating provider's failure to precertify services. When you go to a non-participating provider, it is your responsibility to obtain precertification from Aetna for any services or supplies on the precertification list below. If you do not precertify, your benefits may be reduced. The list of services requiring precertification appear later in this section. Precertification for Emergency services is not required, however, we do suggest that you, or your Physician or facility call as soon as reasonably possible. If your outpatient Hospice Care has been Precertified, and you subsequently require a Hospital stay for pain control or acute symptom management, that Hospital stay does not have to be Precertified. Important Note Please read the following sections in their entirety for important information on the precertification process, and any impact it may have on your coverage. Services and Supplies Which Require Precertification Precertification is required for the following types of medical expenses: Inpatient and Outpatient Care Stays in a hospital; Stays in a skilled nursing facility; Stays in a rehabilitation facility; Stays in a hospice facility; Stays in a residential treatment facility for treatment of mental disorders and substance abuse; Complex imaging; Cosmetic and reconstructive surgery; Emergency transportation by airplane; Injectables, (immunoglobulins, growth hormones, Multiple Sclerosis medications, Osteoporosis medications, Botox, Hepatitis C medications); Kidney dialysis; Bariatric surgery (obesity); Outpatient back surgery not performed in a physician s office; Sleep studies; Knee surgery; and Wrist surgery. The Out-of-Network Precertification Process Precertification should be secured within the timeframes specified below. To obtain precertification, call Aetna at the telephone number listed on the back of your ID card. This call must be made: HO SG2015COC 01 6 SG Off Exchange
7 For non-emergency admissions: For an emergency admission: For an urgent admission: For outpatient non-emergency medical services requiring Precertification: You or a member of your family, your Physician or the facility will need to call and request Precertification at least 14 days before the date you are scheduled to be admitted. You or a member of your family, your Physician or the facility should call within 48 hours or as soon as reasonably possible after you have been admitted. You or a member of your family, your Physician or the facility will need to call before you are scheduled to be admitted. You or a member of your family, your Physician or the facility must call at least 14 days before the outpatient care is provided, or the treatment or procedure is scheduled. Aetna will provide a written notification to you and your Physician of the Precertification decision where required under applicable State law. If your Precertified expenses are approved the approval is good for 180 days as long as you remain enrolled in the plan. Precertification, Precertify, Precertified A process where Aetna is contacted before certain services are provided, such as hospitalization or outpatient services, or prescription drugs are prescribed to determine whether the services being recommended or the drugs prescribed are considered covered expenses under the plan. It is not a guarantee that benefits will be payable if, for example, it is determined at the time the claim is submitted that you were not eligible for benefits at that time. Precertification Penalty Aetna will reduce the benefits payable under this Certificate by the percentage or dollar amount set forth on the Schedule of Benefits if the procedures for Precertification set forth in this Certificate are not followed when the member uses their non-participating benefits. The Member will be responsible to pay the unpaid balance of the benefits. FAILURE TO PRECERTIFY WILL RESULT IN A REDUCTION OF BENEFITS UNDER THIS CERTIFICATE. PLEASE REFER TO THE SCHEDULE OF BENEFITS FOR THE PRECERTIFICATION PENALTY. The additional percentage or dollar amount of the Recognized Charge for non-participating benefits which a Member may pay as a penalty for failure to obtain Precertification under this section is not a Covered Expense, and will not be applied to the Deductible amount or the Maximum Out-of-Pocket Limit, if any. HO SG2015COC 01 7 SG Off Exchange
8 ELIGIBILITY AND ENROLLMENT Eligibility Subscriber To be eligible to enroll as a Subscriber, an individual must: Meet all applicable eligibility requirements agreed upon by the Contract Holder employer and Aetna; and Live or work in the Service Area Determining if You Are in an Eligible Class You are in an eligible class if you are a regular full-time employee, as defined by your employer. Determining When You Become Eligible You become eligible for the plan on your eligibility date, which is determined as follows: On the Effective Date of the Plan If you are in an Eligible Class on the effective date of your plan, your Eligibility Date is the effective date of this Plan or, if later, the date you complete the period of continuous service required by your employer. Your employer determines the criteria that is used to define the Eligible Class for coverage under this Certificate. Such criteria are based solely upon conditions related to your employment. See your employer for details. After the Effective Date of the Plan If you are in an Eligible Class on the date of hire, your Eligibility Date is the effective date of this Plan or, if later, the date you complete the period of continuous service required by your employer. Your employer determines the criteria that is used to define the Eligible Class for coverage under this Certificate. Such criteria are based solely upon conditions related to your employment. See your employer for details. Waiting Period Once you enter an eligible class, you will need to complete the waiting period before your coverage under this plan begins. Obtaining Coverage for Dependents To be eligible to enroll as a Covered Dependent, the Contract Holder employer must provide dependent coverage for Subscribers who are eligible and must be: Your legal spouse; Your dependent children. HO SG2015COC 01 8 SG Off Exchange
9 Coverage for Dependent Children To be eligible for coverage, a dependent child must be: Under 26 years of age. Covered Benefits for a Covered Dependent who is not capable of self-support due to intellectual disability or physical disability will be continued past the maximum age for a child. An eligible dependent child includes: Your biological children. Your stepchildren. Your legally adopted children. Your foster children, including any children placed with you for adoption. Any children for whom you are responsible under court order. Your grandchildren in your court-ordered custody. Any child whose parent is your child and your child is covered as a dependent under this Plan. Any other child with whom you have a parent-child relationship. No individual may be covered both as an employee and dependent and no individual may be covered as a dependent of more than one employee. How And When To Enroll Enrollment Unless otherwise noted, an eligible individual and any eligible dependents may enroll in Aetna regardless of health status, age, or requirements for health services within 31 days from the eligibility date. Newly Eligible Individuals and Eligible Dependents An eligible individual and any eligible dependents may enroll within 31 days of the eligibility date. Enrollment of Newly Eligible Dependents Newborn Children Newborn children of the Subscriber are eligible for coverage from the date of birth for a 60 day period. Adoptive children of the Subscriber, including children Placed For Adoption, are eligible for coverage for a 60 day period from (a) the date of birth, if Placed For Adoption within 60 days of the child s birth; or (b) the date of placement, if the adoptive child is Placed For Adoption 60 days or more after the child s birth. Coverage will be continued beyond the initial 60 days only if Aetna receives the required enrollment forms or paperwork and any additional premium due for the Child s birth, adoption, or Placement for Adoption. If additional premium is required to enroll the child and is not received after Thirty-one (31) days from the premium billing notice provided to the employee by the Group, coverage will not continue for the child. Aetna will pursue collection of the additional premium required for the initial 60-day period of coverage. HO SG2015COC 01 9 SG Off Exchange
10 Special Rules Which Apply to Children Qualified Medical Child Support Order When a subscriber or subscriber s spouse is required by court order, Qualified Medical Support Order (QMSO), National Medical Support Notice (NMSN), or other administrative order to provide health insurance coverage for a child, we may not deny enrollment of the child on the grounds that the child does not reside with the subscriber or within our service area. The subscriber must provide proof of court order, QMSO, NMSN, or administratively ordered coverage. At the time of enrollment, the child s state of residence must be established. The custodial parent must abide by all terms and conditions of the benefit plan. The Coventry Health Care National Network of providers is available to court-ordered dependent children living outside the service area. Participating benefits apply to services received from these providers. If the child chooses to use an Aetna provider or a Coventry Health Care National Network provider, prior authorization must be obtained for those services listed. section of this handbook. Handicapped Children An unmarried child of the Subscriber or the Subscriber s lawful spouse who is age twenty-six (26) or older, who is certified as incapable of self-sustaining employment by reason of intellectual disability or physical disability incurred prior to the child s 26 th birthday, who is chiefly dependent upon the Subscriber or the Subscriber s lawful spouse for support, and is not eligible for other health care coverage. Proof of such incapacity and dependency must be furnished to Us within thirty (30) days of request. Such certification will consist of a statement by a qualified Physician, attesting to the disability. Proof of continued incapacity, including a medical examination, must be submitted to Aetna as requested, but not more frequently than annually beginning after the 2 year period. Notification of Change in Status It shall be a Member s responsibility to notify Aetna of any changes which affect the Member s coverage under this Certificate, unless a different notification process is agreed to between Aetna and Contract Holder employer. Such status changes include, but are not limited to, change of address, change of Covered Dependent status, and enrollment in Medicare or any other group health plan of any Member. Additionally, if requested, a Subscriber must provide to Aetna, within 31 days of the date of the request, evidence satisfactory to Aetna that a dependent meets the eligibility requirements described in this Certificate. Special Enrollment Period An eligible individual and eligible dependents may be enrolled during a Special Enrollment Periods. A Special Enrollment Period may apply when an eligible individual or eligible dependent loses other health coverage or when an eligible individual acquires a new eligible dependent through marriage, birth, adoption or placement for adoption. HO SG2015COC SG Off Exchange
11 Special Enrollment Period for Certain Individuals Who Lose Other Health Coverage: An eligible individual or an eligible dependent may be enrolled during a Special Enrollment Period, if the following requirements, as applicable, are met: The eligible individual or the eligible dependent was covered under another group health plan or other health insurance coverage when initially eligible for coverage under Aetna; The eligible individual or eligible dependent previously declined coverage in writing under Aetna The eligible individual or eligible dependent becomes eligible for State premium assistance in connection with coverage under Aetna The eligible individual or eligible dependent loses coverage under the other group health plan or other health insurance coverage for one of the following reasons: - The other group health coverage is COBRA continuation coverage under another plan, and the COBRA continuation coverage under that other plan has since been exhausted; - The other coverage is a group health plan or other health insurance coverage, and the other coverage has been terminated as a result of loss of eligibility for the coverage or employer contributions towards the other coverage have been terminated; or - The other health insurance coverage is Medicaid or an S-Chip plan and the eligible individual or eligible dependent no longer qualifies for such coverage. Loss of eligibility includes the following: - A loss of coverage as a result of legal separation, divorce or death; - Termination of employment; - Reduction in the number of hours of employment; - Any loss of eligibility after a period that is measured by reference to any of the foregoing; - Termination of Aetna coverage due to Member action- movement outside of the Aetna s service area; and also the termination of health coverage including Non-Aetna, due to plan termination. - Plan ceases to offer coverage to a group of similarly situated individuals; - Cessation of a dependent s status as an eligible dependent - Termination of benefit package Loss of eligibility does not include a loss due to failure of the individual or the participant to pay Premiums on a timely basis or due to termination of coverage for cause as referenced in the Termination of Coverage section of this Certificate. To be enrolled in Aetna during a Special Enrollment Period, the eligible individual or eligible dependent must enroll within: 31 days, beginning on the date of the eligible individual's or eligible dependent's loss of other group health plan or other health insurance coverage; or 60 days, beginning on the date the eligible individual or eligible dependent - Becomes eligible for premium assistance in connection with coverage under Aetna, or - Is no longer qualified for coverage under Medicaid or S-Chip. HO SG2015COC SG Off Exchange
12 The Effective Date of Coverage will be the first day of the first calendar month following the date the completed request for enrollment is received. Special Enrollment Period When a New Eligible Dependent is Acquired: When a new eligible dependent is acquired through marriage, birth, adoption or placement for adoption, the new eligible dependent (and, if not otherwise enrolled, the eligible individual and other eligible dependents) may be enrolled during a special enrollment period. The special enrollment period is a period of 60 days, beginning on the date of the marriage, birth, adoption or placement for adoption (as the case may be). If a completed request for enrollment is made during that period, the Effective Date of Coverage will be: In the case of marriage, the first day of the first calendar month following the date the completed request for enrollment is received. In the case of a dependent s birth, adoption or placement for adoption, the date of such birth, adoption or placement for adoption. The eligible individual or the eligible dependent enrolling during a special enrollment period will not be subject to late enrollment provisions, if any, described in this Certificate. Effective Date of Coverage Coverage shall take effect at 12:01 a.m. on the Member s effective date. Coverage shall continue in effect from month to month subject to payment of Premiums made by the Contract Holder employer and subject to the Termination section of the Group Agreement, and the Termination of Coverage section of this Certificate. Hospital Confinement on Effective Date of Coverage If a Member is an inpatient in a Hospital on the Effective Date of Coverage, the Member will be covered as of that date. Such services are not covered if the Member is covered by another health plan on that date and the other health plan is responsible for the cost of the services. Aetna will not cover any service that is not a Covered Benefit under this Certificate. HO SG2015COC SG Off Exchange
13 COVERED BENEFITS A Member shall be entitled to the Covered Benefits as specified below, in accordance with the terms and conditions of this Certificate. Unless specifically stated otherwise, in order for benefits to be covered, they must be Medically Necessary. For the purpose of coverage, Aetna may determine whether any benefit provided under the Certificate is Medically Necessary, and Aetna has the option to only authorize coverage for a Covered Benefit performed by a particular Provider. Preventive care, as described below, will be considered Medically Necessary. Important Note: You should review your Schedule of Benefits for the cost sharing that applies to the Covered Benefits in this section. This will help you become familiar with your payment responsibilities. Some Covered Benefits may have visit limits and maximums that apply to the service or supply. You should always review your Certificate and Schedule of Benefits together. ALL SERVICES ARE SUBJECT TO THE EXCLUSIONS AND LIMITATIONS DESCRIBED IN THIS CERTIFICATE. To be Medically Necessary, the service or supply must: Be care or treatment as likely to produce a significant positive outcome as, and no more likely to produce a negative outcome than, any alternative service or supply, both as to the disease or injury involved and the Member's overall health condition; Be care or services related to diagnosis or treatment of an existing illness or injury, except for Preventive Care Benefits, as determined by Aetna; Be a diagnostic procedure, indicated by the health status of the Member and be as likely to result in information that could affect the course of treatment as, and no more likely to produce a negative outcome than, any alternative service or supply, both as to the disease or injury involved and the Member's overall health condition; Include only those services and supplies that cannot be safely and satisfactorily provided at home, in a Physician s or Dental Provider s office, on an outpatient basis, or in any facility other than a Hospital, when used in relation to inpatient Hospital services; and As to diagnosis, care and treatment be no more costly (taking into account all health expenses incurred in connection with the service or supply) than any equally effective service or supply in meeting the above tests. In determining if a service or supply is Medically Necessary, Aetna s Patient Management Medical Director or its Physician or Dentist designee will consider: Information provided on the Member's health status; Reports in peer reviewed medical literature; Reports and guidelines published by nationally recognized health care organizations that include supporting scientific data; HO SG2015COC SG Off Exchange
14 Professional standards of safety and effectiveness which are generally recognized in the United States for diagnosis, care or treatment; The opinion of Health Professionals in the generally recognized health specialty involved; The opinion of the attending Physicians or Dental Providers, which have credence but do not overrule contrary opinions; and Any other relevant information brought to Aetna's attention. All Covered Benefits will be covered in accordance with the guidelines determined by Aetna. If a Member has questions regarding coverage under this Certificate, the Member may call the Member Services toll-free telephone number listed on the Member s identification card. THE MEMBER IS RESPONSIBLE FOR PAYMENT OF THE APPLICABLE COPAYMENTS AND DEDUCTIBLES LISTED ON THE SCHEDULE OF BENEFITS. IMPORTANT: REFER TO THE AETNA PROCEDURE SECTION OF THIS CERTIFICATE FOR THE LIST OF SERVICES AND SUPPLIES WHICH REQUIRE PRECERTIFICATION. 1. Preventive Care and Wellness Benefits Preventive Care 1. The recommendations and guidelines of the: Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention; United States Preventive Services Task Force; Health Resources and Services Administration; and American Academy of Pediatrics/Bright Futures Guidelines for Children and Adolescents as referenced throughout this Preventive Care Benefit may be updated periodically. This Plan is subject to updated recommendations or guidelines that are issued by these organizations beginning on the first day of the plan year, one year after the recommendation or guideline is issued. 2. If any diagnostic x-rays, lab, or other tests or procedures are ordered, or given, in connection with any of the Preventive Care Benefits described below, those diagnostic x-rays, lab or other tests or procedures will not be covered as Preventive Care Benefits. Those that are Covered Benefits will be subject to the cost-sharing that applies to those specific services under this Plan. 3. Refer to the Schedule of Benefits for information about cost-sharing and maximums that apply to Preventive Care benefits. 4. To learn what frequency and age limits apply to routine physical exams and routine cancer screenings, contact your physician or contact Member Services by logging onto your Aetna Navigator secure member website at or calling the number on the back of your ID card. This information can also be found at the website. HO SG2015COC SG Off Exchange
15 Routine Physical Exam Benefit Covered Benefits include office visits to a Member's Physician or Primary Care Physician (PCP) for routine physical exams, including routine vision and hearing screenings given as part of the routine physical exam. A routine exam is a medical exam given by a physician for a reason other than to diagnose or treat a suspected or identified illness or injury, and also includes: Evidence-based items that have in effect a rating of A or B in the current recommendations of the United States Preventive Services Task Force; Services as recommended in the American Academy of Pediatrics/Bright Futures/Health Resources and Services Administration guidelines for children and adolescents. For females, screenings and counseling services as provided for in the comprehensive guidelines recommended by the Health Resources and Services Administration. These services may include but are not limited to: - Screening and counseling services, such as those on: - Interpersonal and domestic violence; - Sexually transmitted diseases; and - Human Immune Deficiency Virus (HIV) infections. - Screening for gestational diabetes. - High risk Human Papillomavirus (HPV) DNA testing for women age 30 and older. X-rays, lab and other tests given in connection with the exam. For covered newborns, an initial Hospital checkup. Benefits for the routine physical exam services above may be subject to visit maximums as shown in the Schedule of Benefits. For details on the frequency and age limits that apply to Routine Physical Exam Benefit, Members may contact Member Services by logging onto your Aetna Navigator secure member website at or calling the number on the back of your ID card. Benefit Limitations: Unless specified above, not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; Services which are for diagnosis or treatment of a suspected or identified illness or injury; Exams given while the Member is confined in a Hospital or other facility for medical care; Services not given by a Physician or under his or her direction; and Psychiatric, psychological, personality or emotional testing or exams. Preventive Care Immunizations Benefit Covered Benefits include: Immunizations for infectious diseases; and The materials for administration of immunizations; provided by a Member's PCP or a facility. The immunizations must be recommended by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention. HO SG2015COC SG Off Exchange
16 Benefit Limitations: Not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; and Immunizations that are not considered preventive care such as those required due to a Member's employment or travel. Preventive Care Drugs and Supplements Covered Benefits include preventive care drugs and supplements (including over-the-counter drugs and supplements) obtained at a pharmacy. They are covered when they are: prescribed by a Physician; obtained at a pharmacy; and submitted to a pharmacist for processing. The preventive care drugs and supplements covered under this plan include, but may not be limited to: Aspirin: Benefits are available to adults. Oral Fluoride Supplements: Benefits are available to pre-school children whose primary water source is deficient in fluoride. Folic Acid Supplements: Benefits are available to adult females planning to become pregnant or capable of pregnancy. Iron Supplements: Benefits are available to children without symptoms of iron deficiency. Coverage is limited to children who are at increased risk for iron deficiency anemia. Vitamin D Supplements: Benefits are available to adults to promote calcium absorption and bone growth in their bodies Reimbursement of Preventive Care Drugs and Supplements at a Pharmacy You will be reimbursed by Aetna for the cost of the preventive care drugs and supplements when you submit proof of loss to Aetna that you purchased a preventive care drug or supplement at a pharmacy. Proof of loss means a copy of the receipt that contains the Prescription information provided by the pharmacist (it is attached to the bag that contains the preventive care OTC drug or supplement). Refer to the provisions Reporting of Claims and Payment of Benefits later in this booklet-certificate for information. You can also contact Member Services by logging onto your Aetna Navigator secure member website at or calling the number on the back of your ID card. Risk Reducing Breast Cancer Prescription Drugs Covered Benefits include Prescription Drugs when prescribed by a Prescriber and the Prescription is submitted to the pharmacist for processing for a woman who is at: Increased risk for breast cancer, and Low risk for adverse medication side effects Coverage of preventive care drugs and supplements will be subject to any sex, age, medical condition, family history, and frequency guidelines in the recommendations of the United States Preventive Services Task Force. HO SG2015COC SG Off Exchange
17 Contraceptives Covered expenses include charges made by a physician for female contraceptive generic prescription drugs and generic and brand name devices that are approved by the FDA. Coverage includes the related services and supplies needed to administer the covered contraceptive. The following contraceptive drugs and devices are covered: Contraceptive Pills Depo Provera Cervical cap and diaphragm Female Condom Implantable Capsules Injection Administration Intrauterine Devices (IUDs) Spermicide and Cervical Sponge/Shield Contraceptive rings and patches Additional information: Covered expenses include charges made by a pharmacy for the following contraceptive methods when prescribed by a prescriber and the prescription is submitted to the pharmacist for processing: Female contraceptives that are prescription drugs and over-the-counter (OTC), including emergency contraceptives that are included on the preferred drug list (formulary). Female contraceptive devices. Benefits are payable under your medical or pharmacy benefit depending on the type of expense and how and where the expense is incurred. Benefits are payable under your medical plan when charges are made by a physician to insert or remove a prescription drug or device. Refer to your Schedule of Benefits for the Female Contraceptives - Copayment and Deductible Waiver provision for more information. Important Note: For details on the guidelines and the current list of covered preventive care drugs and supplements, including risk reducing breast cancer Prescription Drugs, contact Member Services by logging onto your Aetna Navigator secure member website at or calling the number on the back of your ID card. Refer to the Schedule of Benefits for the cost-sharing and supply limits that apply to these benefits. Well Woman Preventive Visits Benefit Covered Benefits include a routine well woman preventive exam office visit, including Pap smears, provided by a Member's PCP, Physician, obstetrician, or gynecologist in accordance with the recommendations by the Health Resources and Services Administration. A routine well woman preventive exam is a medical exam given by a Physician for a reason other than to diagnose or treat a suspected or identified illness or injury; and HO SG2015COC SG Off Exchange
18 routine preventive care breast cancer genetic counseling and breast cancer (BRCA) gene blood testing. Covered Benefits include charges made by a Physician and lab for the BRCA gene blood test and charges made by a genetic counselor to interpret the test results and evaluate treatment. These benefits will be subject to any age; family history; and frequency guidelines that are: Evidence-based items or services that have in effect a rating of A or B in the recommendations of the United States Preventive Services Task Force; and Evidence-informed items or services provided in the comprehensive guidelines supported by the Health Resources and Services Administration. Benefits for the well woman preventive visit services above are subject to visit maximums as shown in the Schedule of Benefits. Benefit Limitations: Unless specified above, not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; Services which are for diagnosis or treatment of a suspected or identified illness or injury; Exams given while the Member is confined in a Hospital or other facility for medical care; Services not given by a Physician or under his or her direction; and Psychiatric, psychological, personality or emotional testing or exams. Screening and Counseling Services Benefit Covered Benefits include the following services provided by a Member's PCP or Physician, as applicable, in an individual or group setting: Obesity and Healthy Diet Counseling Benefit Covered Benefits include screening and counseling services to aid in weight reduction due to obesity. Coverage includes: Preventive counseling visits and/or risk factor reduction intervention; Nutritional counseling; and Healthy diet counseling visits provided in connection with Hyperlipidemia (high cholesterol) and other known risk factors for cardiovascular and diet-related chronic disease. Benefits for the screening and counseling services above are subject to the visit maximums as shown in the Schedule of Benefits. Misuse of Alcohol and/or Drugs Benefit Covered Benefits include screening and counseling services to aid in the prevention or reduction of the use of an alcohol agent or controlled substance. Coverage includes preventive counseling visits, risk factor reduction intervention and a structured assessment. Benefits for the screening and counseling services above are subject to visit maximums as shown later in this amendment. HO SG2015COC SG Off Exchange
19 Use of Tobacco Products Benefit Covered Benefits include screening and counseling services to aid in the cessation of the use of tobacco products. Coverage includes: Preventive counseling visits; Treatment visits; and Class visits; to aid in the cessation of the use of tobacco products. Tobacco product means a substance containing tobacco or nicotine including: Cigarettes; Cigars; Smoking tobacco; Snuff; Smokeless tobacco; and Candy-like products that contain tobacco. Benefits for the screening and counseling services above are subject to visit maximums as shown in the Schedule of Benefits. Sexually Transmitted Infection Counseling Covered Benefits include the counseling services to help you prevent or reduce sexually transmitted infections. Genetic Risk Counseling for Breast and Ovarian Cancer Covered Benefits include the counseling and evaluation services to help you assess whether or not you are at risk of breast and ovarian cancer. Benefit Limitations: Unless specified above, not covered under this benefit are services which are covered to any extent under any other part of this Certificate. Routine Cancer Screenings Benefit Covered Benefits include, but are not limited to, the following routine cancer screenings: Mammograms; Fecal occult blood tests; Digital rectal exams; Prostate specific antigen (PSA) tests; Sigmoidoscopies; Double contrast barium enema (DCBE); and Colonoscopies; (removal of polyps performed during a screening procedure is a Covered Benefit); and Lung cancer screenings. HO SG2015COC SG Off Exchange
20 Benefit Limitations: Coverage for mammography shall include at least the following benefits: 1. One baseline mammogram for a woman who is 35 through 39 years of age. 2. A mammogram every two years for a woman who is 40 through 49 years of age, or more frequently if recommended by the woman s physician. 3. A mammogram every year for a woman who is 50 years of age or older. 4. A mammogram for any woman desiring a mammogram for medical cause. Mammogram services that exceed the frequency and/or age provisions set forth in 1 through 3 above will be covered if guidelines established by Aetna, the United States Preventive Services Task Force, or local government health authorities indicate that such services are recommended. These benefits will be subject to any age, family history and frequency guidelines that are: Evidence-based items or services that have in effect a rating of A or B in the recommendations of the United States Preventive Services Task Force; and Evidence-informed items or services provided in the comprehensive guidelines supported by the Health Resources and Services Administration. For details on the frequency and age limits that apply to Routine Cancer Screenings Benefit, Members may contact Member Services by logging onto your Aetna Navigator secure member website at or calling the number on the back of your ID card. As to routine gynecological exams performed as part of a routine cancer screening, the Member may go directly to a Participating obstetrician (OB), gynecologist (GYN), obstetrician/gynecologist (OB/GYN). Unless specified above, not covered under this benefit are services which are covered to any extent under any other part of this Plan. Prenatal Care Benefit Prenatal care will be covered as Preventive Care for services received by a pregnant female in a PCP, or Physician's, OB-GYN, obstetrician's, or gynecologist's office but only to the extent described below. Coverage for prenatal care under this benefit is limited to pregnancy-related Physician office visits including the initial and subsequent history and physical exams of the pregnant woman (maternal weight, blood pressure, fetal heart rate check and fundal height). Benefit Limitations: Unless specified above, not covered under this benefit are: Services which are covered to any extent under any other part of this Plan; and Services for maternity care (other than prenatal care as described above). Important Note: Refer to the: Maternity Care and Related Newborn Care Benefits section of the Certificate; and Prenatal Care Services, Delivery Services and Postpartum Care Services cost-sharing in the Schedule of Benefits; for more information on coverage for services related to maternity care under this Plan. HO SG2015COC SG Off Exchange
21 Comprehensive Lactation Support and Counseling Services Benefit Covered Benefits include comprehensive lactation support (assistance and training in breast feeding) and counseling services provided to females during pregnancy or at any time following delivery, for breastfeeding by a certified lactation support provider. Covered Benefits also include the rental or purchase of breast feeding equipment as described below. Lactation support and lactation counseling services are Covered Benefits when provided in either a group or individual setting. Benefits for lactation counseling services are subject to the visit maximum shown later in this amendment. Breast Feeding Durable Medical Equipment Covered Benefits includes the rental or purchase of breast feeding Durable Medical Equipment for the purpose of lactation support (pumping and storage of breast milk). Family Planning Services - Female Contraceptives Benefit Important Note: For a list of the types of female contraceptives covered under this plan, refer to the section What the Pharmacy Benefit Covers and the Contraceptives benefit later in this Booklet-Certificate. For females with reproductive capacity, Covered Benefits include those services and supplies that are provided to a Member to prevent pregnancy. All contraceptive methods, services and supplies covered under this benefit must be approved by the U.S. Food and Drug Administration (FDA). Contraceptives Covered Benefits include charges made by a Physician or pharmacy for: Services and supplies needed to administer or remove a covered contraceptive Prescription Drug or device; Female oral and injectable contraceptive that are Biosimilar Prescription Drugs, Brand Name Prescription Drugs and Generic Prescription Drugs; Female contraceptive devices that are generic devices and brand name devices; FDA-approved female: - Biosimilar, brand name and generic emergency contraceptives; - Brand name and generic over-the-counter (OTC) emergency contraceptives for which a Prescription is not needed. Voluntary Sterilization Covered Benefits include charges billed separately by the provider for female voluntary sterilization procedures and related services and supplies including, but not limited to, tubal ligation and sterilization implants. HO SG2015COC SG Off Exchange
22 Physician and Other Health Professional Care Primary Care Physician Benefit Office visits during office hours. Home visits. After-hours PCP services. PCPs are required to provide or arrange for on-call coverage 24 hours a day, 7 days a week. If a Member becomes sick or is injured after the PCP's regular office hours, the Member should: - call the PCP's office; - identify himself or herself as a Member; and - follow the PCP's or covering Physician s instructions. If the Member's injury or illness is a Medical Emergency, the Member should follow the procedures outlined under the Emergency Care/Urgent Care Benefits section of this Certificate. Hospital visits. Immunizations for infectious disease, but not if solely for your employment or travel. Allergy testing and allergy injections. Charges made by the Physician for supplies, radiological services, x-rays, and tests provided by the Physician. Covered Benefits include outpatient and inpatient services. Member may request a second opinion regarding a proposed surgery or course of treatment recommended by Member's PCP or a Specialist. Important Reminder: For a description of the preventive care benefits covered under this Certificate, refer to the Preventive Care Benefits section in this Certificate. 2. Hospital and Other Facility Care Hospital Benefit A Member is covered for inpatient Hospital services and supplies. All services are subject to precertification by Aetna. In the event that the Member elects to remain in the Hospital after the date that the provider and/or the Aetna Medical Director has determined and advised the Member that the Member no longer meets the criteria for continued inpatient confinement, the Member shall be fully responsible for direct payment to the Hospital Facility for such additional Hospital, Physician and other Provider services, and Aetna shall not be financially responsible for such additional services. Inpatient Hospital cardiac and pulmonary rehabilitation services are covered by Participating and Non- Participating Providers and precertification by Aetna. Refer to the Short-Term Cardiac and Pulmonary Rehabilitation Therapy Services benefit for more information. HO SG2015COC SG Off Exchange
Aetna Life Insurance Company
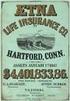 Aetna Life Insurance Company Hartford, Connecticut 06156 Amendment Policyholder: Group Policy No.: Effective Date: UNIVERSITY OF PENNSYLVANIA POSTDOCTORAL INSURANCE PLAN GP-861472 This Amendment is effective
Aetna Life Insurance Company Hartford, Connecticut 06156 Amendment Policyholder: Group Policy No.: Effective Date: UNIVERSITY OF PENNSYLVANIA POSTDOCTORAL INSURANCE PLAN GP-861472 This Amendment is effective
AETNA HEALTH INC. (GEORGIA) CERTIFICATE OF COVERAGE
 AETNA HEALTH INC. (GEORGIA) CERTIFICATE OF COVERAGE Plan Name: Silver HNOption 5200 100/50 O0140010116071 This Certificate of Coverage ("Certificate") is part of the Group Agreement ("Group Agreement")
AETNA HEALTH INC. (GEORGIA) CERTIFICATE OF COVERAGE Plan Name: Silver HNOption 5200 100/50 O0140010116071 This Certificate of Coverage ("Certificate") is part of the Group Agreement ("Group Agreement")
AETNA HEALTH OF UTAH INC. (WYOMING) CERTIFICATE OF COVERAGE In-network and out-of-network coverage under the Aetna
 AETNA HEALTH OF UTAH INC. (WYOMING) WY Silver HNOption 3000 70/50 WYO0070010116071 CERTIFICATE OF COVERAGE In-network and out-of-network coverage under the Aetna This Certificate of Coverage ("Certificate")
AETNA HEALTH OF UTAH INC. (WYOMING) WY Silver HNOption 3000 70/50 WYO0070010116071 CERTIFICATE OF COVERAGE In-network and out-of-network coverage under the Aetna This Certificate of Coverage ("Certificate")
AETNA HEALTH INC. (Arizona) CERTIFICATE OF COVERAGE
 AETNA HEALTH INC. (Arizona) CERTIFICATE OF COVERAGE Plan Name: AZ Silver HNOption 1500 70/50 AZO0010010116071 This Certificate of Coverage ("Certificate") is part of the Group Agreement ("Group Agreement")
AETNA HEALTH INC. (Arizona) CERTIFICATE OF COVERAGE Plan Name: AZ Silver HNOption 1500 70/50 AZO0010010116071 This Certificate of Coverage ("Certificate") is part of the Group Agreement ("Group Agreement")
AETNA HEALTH INC. (Arizona) CERTIFICATE OF COVERAGE
 Plan Name: AZ Gold HMO 25/50/500 AZN1010010116071 AETNA HEALTH INC. (Arizona) CERTIFICATE OF COVERAGE This Certificate of Coverage ("Certificate") is part of the Group Agreement ("Group Agreement") between
Plan Name: AZ Gold HMO 25/50/500 AZN1010010116071 AETNA HEALTH INC. (Arizona) CERTIFICATE OF COVERAGE This Certificate of Coverage ("Certificate") is part of the Group Agreement ("Group Agreement") between
The Aetna Home Health Benefit Contract
 INTRODUCTION TO YOUR INDIVIDUAL ADVANTAGE CONTRACT Welcome and thank you for choosing Aetna for your health benefits. We are pleased to provide you with this Contract. This Contract and other plan documents
INTRODUCTION TO YOUR INDIVIDUAL ADVANTAGE CONTRACT Welcome and thank you for choosing Aetna for your health benefits. We are pleased to provide you with this Contract. This Contract and other plan documents
What Your Plan Covers and How Benefits are Paid BENEFIT PLAN. Prepared Exclusively for Leidos, Inc. Aetna Choice POS II (HDHP) - Advantage Plan
 BENEFIT PLAN Prepared Exclusively for Leidos, Inc. What Your Plan Covers and How Benefits are Paid Aetna Choice POS II (HDHP) - Advantage Plan Table of Contents Schedule of Benefits...1 Preface...18 Coverage
BENEFIT PLAN Prepared Exclusively for Leidos, Inc. What Your Plan Covers and How Benefits are Paid Aetna Choice POS II (HDHP) - Advantage Plan Table of Contents Schedule of Benefits...1 Preface...18 Coverage
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Adobe Systems Incorporated. Aetna Choice POS II
 Adobe Systems Incorporated Aetna Choice POS II BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group Welfare
Adobe Systems Incorporated Aetna Choice POS II BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group Welfare
What Your Plan Covers and How Benefits are Paid BENEFIT PLAN. Prepared Exclusively for SAMPLE. Open Access Aetna Select
 BENEFIT PLAN Prepared Exclusively for SAMPLE What Your Plan Covers and How Benefits are Paid Open Access Aetna Select Table of Contents Schedule of Benefits... 1 Preface...20 Coverage for You and Your
BENEFIT PLAN Prepared Exclusively for SAMPLE What Your Plan Covers and How Benefits are Paid Open Access Aetna Select Table of Contents Schedule of Benefits... 1 Preface...20 Coverage for You and Your
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Adobe Systems Incorporated. Aetna HealthFund HRA Plan
 Adobe Systems Incorporated Aetna HealthFund HRA Plan BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group
Adobe Systems Incorporated Aetna HealthFund HRA Plan BENEFIT PLAN What Your Plan Covers and How Benefits are Paid This summary is part of, and is meant to be read with, the Adobe Systems Incorporated Group
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Prepared Exclusively for Cerner Corporation (Expatriate Employees)
 BENEFIT PLAN Prepared Exclusively for Cerner Corporation (Expatriate Employees) What Your Plan Covers and How Benefits are Paid PPO Medical, PPO Dental, Basic Vision and Pharmacy Aetna Life and Casualty
BENEFIT PLAN Prepared Exclusively for Cerner Corporation (Expatriate Employees) What Your Plan Covers and How Benefits are Paid PPO Medical, PPO Dental, Basic Vision and Pharmacy Aetna Life and Casualty
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Prepared Exclusively for : Ohio Members participating through the Federal Exchange
 BENEFIT PLAN Prepared Exclusively for : What Your Plan Covers and How Benefits are Paid Ohio Members participating through the Federal Exchange Aetna Life Insurance Company Introduction to Your Policy
BENEFIT PLAN Prepared Exclusively for : What Your Plan Covers and How Benefits are Paid Ohio Members participating through the Federal Exchange Aetna Life Insurance Company Introduction to Your Policy
PARTICIPATING PROVIDERS / REFERRED Deductible (per calendar year)
 Your HMO Plan Primary Care Physician - You choose a Primary Care Physician. The Aetna HMO Deductible provider network gives you access to a wide selection of Primary Care Physicians ( PCP's) and Specialists
Your HMO Plan Primary Care Physician - You choose a Primary Care Physician. The Aetna HMO Deductible provider network gives you access to a wide selection of Primary Care Physicians ( PCP's) and Specialists
FEATURES NETWORK OUT-OF-NETWORK
 Schedule of Benefits Employer: The Vanguard Group, Inc. ASA: 697478-A Issue Date: January 1, 2014 Effective Date: January 1, 2014 Schedule: 3B Booklet Base: 3 For: Choice POS II - 950 Option - Retirees
Schedule of Benefits Employer: The Vanguard Group, Inc. ASA: 697478-A Issue Date: January 1, 2014 Effective Date: January 1, 2014 Schedule: 3B Booklet Base: 3 For: Choice POS II - 950 Option - Retirees
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Appendix A. Prepared Exclusively for The Dow Chemical Company
 Appendix A BENEFIT PLAN Prepared Exclusively for The Dow Chemical Company What Your Plan Covers and How Benefits are Paid Choice POS II (MAP Plus Option 2 - High Deductible Health Plan (HDHP) with Prescription
Appendix A BENEFIT PLAN Prepared Exclusively for The Dow Chemical Company What Your Plan Covers and How Benefits are Paid Choice POS II (MAP Plus Option 2 - High Deductible Health Plan (HDHP) with Prescription
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Prepared Exclusively for Yale University
 BENEFIT PLAN Prepared Exclusively for Yale University What Your Plan Covers and How Benefits are Paid Aetna Choice POS II - Faculty, Management and Professional Staff Table of Contents Preface...1 Important
BENEFIT PLAN Prepared Exclusively for Yale University What Your Plan Covers and How Benefits are Paid Aetna Choice POS II - Faculty, Management and Professional Staff Table of Contents Preface...1 Important
What Your Plan Covers and How Benefits are Paid BENEFIT PLAN. Prepared Exclusively for The McClatchy Company. Aetna Choice Plan
 BENEFIT PLAN Prepared Exclusively for The McClatchy Company What Your Plan Covers and How Benefits are Paid Aetna Choice Plan Table of Contents Preface...1 Important Information Regarding Availability
BENEFIT PLAN Prepared Exclusively for The McClatchy Company What Your Plan Covers and How Benefits are Paid Aetna Choice Plan Table of Contents Preface...1 Important Information Regarding Availability
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Prepared Exclusively for ConocoPhillips
 BENEFIT PLAN Prepared Exclusively for ConocoPhillips What Your Plan Covers and How Benefits are Paid PPO Medical, Pharmacy, and Comprehensive Dental Inpatriate Plan Aetna Life Insurance Company Booklet-Certificate
BENEFIT PLAN Prepared Exclusively for ConocoPhillips What Your Plan Covers and How Benefits are Paid PPO Medical, Pharmacy, and Comprehensive Dental Inpatriate Plan Aetna Life Insurance Company Booklet-Certificate
California Small Group MC Aetna Life Insurance Company
 PLAN FEATURES Deductible (per calendar year) $3,000 Individual $6,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered expenses accumulate separately
PLAN FEATURES Deductible (per calendar year) $3,000 Individual $6,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered expenses accumulate separately
IN-NETWORK MEMBER PAYS. Out-of-Pocket Maximum (Includes a combination of deductible, copayments and coinsurance for health and pharmacy services)
 HMO-OA-CNT-30-45-500-500D-13 HMO Open Access Contract Year Plan Benefit Summary This is a brief summary of benefits. Refer to your Membership Agreement for complete details on benefits, conditions, limitations
HMO-OA-CNT-30-45-500-500D-13 HMO Open Access Contract Year Plan Benefit Summary This is a brief summary of benefits. Refer to your Membership Agreement for complete details on benefits, conditions, limitations
PLAN DESIGN AND BENEFITS POS Open Access Plan 1944
 PLAN FEATURES PARTICIPATING Deductible (per calendar year) $3,000 Individual $9,000 Family $4,000 Individual $12,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being
PLAN FEATURES PARTICIPATING Deductible (per calendar year) $3,000 Individual $9,000 Family $4,000 Individual $12,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being
California Small Group MC Aetna Life Insurance Company
 PLAN FEATURES Deductible (per calendar year) $1,000 per member $1,000 per member Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered expenses accumulate
PLAN FEATURES Deductible (per calendar year) $1,000 per member $1,000 per member Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered expenses accumulate
BENEFIT PLAN. What Your Plan Covers and How Benefits are Paid. Prepared Exclusively for : Participating Illinois Members. Aetna Life Insurance Company
 BENEFIT PLAN Prepared Exclusively for : What Your Plan Covers and How Benefits are Paid Participating Illinois Members Aetna Life Insurance Company This Policy is part of the Insurance Policy between Aetna
BENEFIT PLAN Prepared Exclusively for : What Your Plan Covers and How Benefits are Paid Participating Illinois Members Aetna Life Insurance Company This Policy is part of the Insurance Policy between Aetna
PREFERRED CARE. All covered expenses, including prescription drugs, accumulate toward both the preferred and non-preferred Payment Limit.
 PLAN FEATURES Deductible (per plan year) $300 Individual $300 Individual None Family None Family All covered expenses, excluding prescription drugs, accumulate toward both the preferred and non-preferred
PLAN FEATURES Deductible (per plan year) $300 Individual $300 Individual None Family None Family All covered expenses, excluding prescription drugs, accumulate toward both the preferred and non-preferred
PLAN DESIGN AND BENEFITS Georgia 2-100 HNOption 13-1000-80
 Georgia Health Network Option (POS Open Access) PLAN DESIGN AND BENEFITS Georgia 2-100 HNOption 13-1000-80 PLAN FEATURES PARTICIPATING PROVIDERS NON-PARTICIPATING PROVIDERS Deductible (per calendar year)
Georgia Health Network Option (POS Open Access) PLAN DESIGN AND BENEFITS Georgia 2-100 HNOption 13-1000-80 PLAN FEATURES PARTICIPATING PROVIDERS NON-PARTICIPATING PROVIDERS Deductible (per calendar year)
PLAN DESIGN AND BENEFITS HMO Open Access Plan 912
 PLAN FEATURES Deductible (per calendar year) $1,000 Individual $2,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services
PLAN FEATURES Deductible (per calendar year) $1,000 Individual $2,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services
SMALL GROUP PLAN DESIGN AND BENEFITS OPEN CHOICE OUT-OF-STATE PPO PLAN - $1,000
 PLAN FEATURES PREFERRED CARE NON-PREFERRED CARE Deductible (per calendar year; applies to all covered services) $1,000 Individual $3,000 Family $2,000 Individual $6,000 Family Plan Coinsurance ** 80% 60%
PLAN FEATURES PREFERRED CARE NON-PREFERRED CARE Deductible (per calendar year; applies to all covered services) $1,000 Individual $3,000 Family $2,000 Individual $6,000 Family Plan Coinsurance ** 80% 60%
California PCP Selected* Not Applicable
 PLAN FEATURES Deductible (per calendar ) Member Coinsurance * Not Applicable ** Not Applicable Copay Maximum (per calendar ) $3,000 per Individual $6,000 per Family All member copays accumulate toward
PLAN FEATURES Deductible (per calendar ) Member Coinsurance * Not Applicable ** Not Applicable Copay Maximum (per calendar ) $3,000 per Individual $6,000 per Family All member copays accumulate toward
Bates College Effective date: 01-01-2010 HMO - Maine PLAN DESIGN AND BENEFITS PROVIDED BY AETNA HEALTH INC. - FULL RISK PLAN FEATURES
 PLAN FEATURES Deductible (per calendar year) $500 Individual $1,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Once Family Deductible is met, all family
PLAN FEATURES Deductible (per calendar year) $500 Individual $1,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Once Family Deductible is met, all family
New York Small Group Indemnity Aetna Life Insurance Company Plan Effective Date: 10/01/2010. PLAN DESIGN AND BENEFITS - NY Indemnity 1-10/10*
 PLAN FEATURES Deductible (per calendar year) $2,500 Individual $7,500 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services,
PLAN FEATURES Deductible (per calendar year) $2,500 Individual $7,500 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services,
PLAN DESIGN AND BENEFITS Basic HMO Copay Plan 1-10
 PLAN FEATURES Deductible (per calendar year) Member Coinsurance Not Applicable Not Applicable Out-of-Pocket Maximum $5,000 Individual (per calendar year) $10,000 Family Once the Family Out-of-Pocket Maximum
PLAN FEATURES Deductible (per calendar year) Member Coinsurance Not Applicable Not Applicable Out-of-Pocket Maximum $5,000 Individual (per calendar year) $10,000 Family Once the Family Out-of-Pocket Maximum
PLAN DESIGN AND BENEFITS - New York Open Access EPO 1-10/10
 PLAN FEATURES Deductible (per calendar year) $1,000 Individual $3,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services,
PLAN FEATURES Deductible (per calendar year) $1,000 Individual $3,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. Member cost sharing for certain services,
PLAN DESIGN AND BENEFITS - Tx OAMC Basic 2500-10 PREFERRED CARE
 PLAN FEATURES Deductible (per calendar year) $2,500 Individual $4,000 Individual $7,500 Family $12,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
PLAN FEATURES Deductible (per calendar year) $2,500 Individual $4,000 Individual $7,500 Family $12,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
Preventive Care Coverage Wondering what preventive care your plan covers?
 STAYING WELL Regence BlueCross BlueShield of Oregon is an Independent Licensee of the Blue Cross and Blue Shield Association Preventive Care Coverage Wondering what preventive care your plan covers? Our
STAYING WELL Regence BlueCross BlueShield of Oregon is an Independent Licensee of the Blue Cross and Blue Shield Association Preventive Care Coverage Wondering what preventive care your plan covers? Our
PLAN DESIGN AND BENEFITS - Tx OAMC 2500 08 PREFERRED CARE
 PLAN FEATURES Deductible (per calendar year) $2,500 Individual $5,000 Individual $7,500 3 Individuals per $15,000 3 Individuals per Unless otherwise indicated, the Deductible must be met prior to benefits
PLAN FEATURES Deductible (per calendar year) $2,500 Individual $5,000 Individual $7,500 3 Individuals per $15,000 3 Individuals per Unless otherwise indicated, the Deductible must be met prior to benefits
$25 copay. One routine GYN visit and pap smear per 365 days. Direct access to participating providers.
 HMO-1 Primary Care Physician Visits Office Hours After-Hours/Home Specialty Care Office Visits Diagnostic OP Lab/X Ray Testing (at facility) with PCP referral. Diagnostic OP Lab/X Ray Testing (at specialist)
HMO-1 Primary Care Physician Visits Office Hours After-Hours/Home Specialty Care Office Visits Diagnostic OP Lab/X Ray Testing (at facility) with PCP referral. Diagnostic OP Lab/X Ray Testing (at specialist)
What Your Plan Covers and How Benefits are Paid BENEFIT PLAN. Prepared Exclusively for Vanderbilt University. Aetna Choice POS II Health Fund Plan
 BENEFIT PLAN Prepared Exclusively for Vanderbilt University What Your Plan Covers and How Benefits are Paid Aetna Choice POS II Health Fund Plan Table of Contents Schedule of Benefits... Issued with Your
BENEFIT PLAN Prepared Exclusively for Vanderbilt University What Your Plan Covers and How Benefits are Paid Aetna Choice POS II Health Fund Plan Table of Contents Schedule of Benefits... Issued with Your
100% Percentage at which the Fund will reimburse Fund Administration
 FUND FEATURES HealthFund Amount $500 Employee $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund amount reflected is on a per
FUND FEATURES HealthFund Amount $500 Employee $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund amount reflected is on a per
National PPO 1000. PPO Schedule of Payments (Maryland Small Group)
 PPO Schedule of Payments (Maryland Small Group) National PPO 1000 The benefits outlined in this Schedule are in addition to the benefits offered under Coventry Health & Life Insurance Company Small Employer
PPO Schedule of Payments (Maryland Small Group) National PPO 1000 The benefits outlined in this Schedule are in addition to the benefits offered under Coventry Health & Life Insurance Company Small Employer
Medical Plan - Healthfund
 18 Medical Plan - Healthfund Oklahoma City Community College Effective Date: 07-01-2010 Aetna HealthFund Open Choice (PPO) - Oklahoma PLAN DESIGN AND BENEFITS PROVIDED BY AETNA LIFE INSURANCE COMPANY -
18 Medical Plan - Healthfund Oklahoma City Community College Effective Date: 07-01-2010 Aetna HealthFund Open Choice (PPO) - Oklahoma PLAN DESIGN AND BENEFITS PROVIDED BY AETNA LIFE INSURANCE COMPANY -
PLAN DESIGN AND BENEFITS AETNA LIFE INSURANCE COMPANY - Insured
 PLAN FEATURES Deductible (per calendar year) Individual $750 Individual $1,500 Family $2,250 Family $4,500 All covered expenses accumulate simultaneously toward both the preferred and non-preferred Deductible.
PLAN FEATURES Deductible (per calendar year) Individual $750 Individual $1,500 Family $2,250 Family $4,500 All covered expenses accumulate simultaneously toward both the preferred and non-preferred Deductible.
PLAN DESIGN AND BENEFITS - PA Health Network Option AHF HRA 1.3. Fund Pays Member Responsibility
 HEALTHFUND PLAN FEATURES HealthFund Amount (Per plan year. Fund changes between tiers requires a life status change qualifying event.) Fund Coinsurance (Percentage at which the Fund will reimburse) Fund
HEALTHFUND PLAN FEATURES HealthFund Amount (Per plan year. Fund changes between tiers requires a life status change qualifying event.) Fund Coinsurance (Percentage at which the Fund will reimburse) Fund
Individual. Employee + 1 Family
 FUND FEATURES HealthFund Amount Individual Employee + 1 Family $750 $1,125 $1,500 Amount contributed to the Fund by the employer is reflected above. Fund Amount reflected is on a per calendar year basis.
FUND FEATURES HealthFund Amount Individual Employee + 1 Family $750 $1,125 $1,500 Amount contributed to the Fund by the employer is reflected above. Fund Amount reflected is on a per calendar year basis.
100% Fund Administration
 FUND FEATURES HealthFund Amount $500 Employee $750 Employee + Spouse $750 Employee + Child(ren) $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance Percentage at which the Fund
FUND FEATURES HealthFund Amount $500 Employee $750 Employee + Spouse $750 Employee + Child(ren) $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance Percentage at which the Fund
Business Life Insurance - Health & Medical Billing Requirements
 PLAN FEATURES Deductible (per plan year) $2,000 Employee $2,000 Employee $3,000 Employee + Spouse $3,000 Employee + Spouse $3,000 Employee + Child(ren) $3,000 Employee + Child(ren) $4,000 Family $4,000
PLAN FEATURES Deductible (per plan year) $2,000 Employee $2,000 Employee $3,000 Employee + Spouse $3,000 Employee + Spouse $3,000 Employee + Child(ren) $3,000 Employee + Child(ren) $4,000 Family $4,000
PLAN DESIGN & BENEFITS MEDICAL PLAN PROVIDED BY AETNA LIFE INSURANCE COMPANY
 Gettysburg College, Inc. PLAN FEATURES Deductible (per calendar year) $500 Individual $1,500 Individual $1,000 Family $3,000 Family All covered expenses accumulate separately toward the preferred or non-preferred
Gettysburg College, Inc. PLAN FEATURES Deductible (per calendar year) $500 Individual $1,500 Individual $1,000 Family $3,000 Family All covered expenses accumulate separately toward the preferred or non-preferred
PLAN DESIGN AND BENEFITS - Tx OAMC 1500-10 PREFERRED CARE
 PLAN FEATURES Deductible (per calendar year) $1,500 Individual $3,000 Individual $4,500 Family $9,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
PLAN FEATURES Deductible (per calendar year) $1,500 Individual $3,000 Individual $4,500 Family $9,000 Family 3 Individuals per Family 3 Individuals per Family Unless otherwise indicated, the Deductible
Unlimited except where otherwise indicated.
 PLAN FEATURES Deductible (per calendar year) $1,250 Individual $5,000 Individual $2,500 Family $10,000 Family All covered expenses including prescription drugs accumulate separately toward both the preferred
PLAN FEATURES Deductible (per calendar year) $1,250 Individual $5,000 Individual $2,500 Family $10,000 Family All covered expenses including prescription drugs accumulate separately toward both the preferred
PLAN DESIGN & BENEFITS - CONCENTRIC MODEL
 PLAN FEATURES Deductible (per calendar year) Rice University None Family Member Coinsurance Applies to all expenses unless otherwise stated. Payment Limit (per calendar year) $1,500 Individual $3,000 Family
PLAN FEATURES Deductible (per calendar year) Rice University None Family Member Coinsurance Applies to all expenses unless otherwise stated. Payment Limit (per calendar year) $1,500 Individual $3,000 Family
HEALTH SAVINGS PPO PLAN (WITH HSA) - COLUMBUS PROVIDED BY AETNA LIFE INSURANCE COMPANY EFFECTIVE JANUARY 1, 2016 AETNA INC.
 HEALTH SAVINGS PPO PLAN (WITH HSA) - COLUMBUS PROVIDED BY AETNA LIFE INSURANCE COMPANY EFFECTIVE JANUARY 1, 2016 AETNA INC. CPOS II DEDUCTIBLE, COPAYS/COINSURANCE AND DOLLAR MAXIMUMS and Aligned Deductible
HEALTH SAVINGS PPO PLAN (WITH HSA) - COLUMBUS PROVIDED BY AETNA LIFE INSURANCE COMPANY EFFECTIVE JANUARY 1, 2016 AETNA INC. CPOS II DEDUCTIBLE, COPAYS/COINSURANCE AND DOLLAR MAXIMUMS and Aligned Deductible
OverVIEW of Your Eligibility Class by determineing Benefits
 OVERVIEW OF YOUR BENEFITS IMPORTANT PHONE NUMBERS Benefit Fund s Member Services Department (646) 473-9200 For answers to questions about your eligibility or prescription drug benefit. You can also visit
OVERVIEW OF YOUR BENEFITS IMPORTANT PHONE NUMBERS Benefit Fund s Member Services Department (646) 473-9200 For answers to questions about your eligibility or prescription drug benefit. You can also visit
Employee + 2 Dependents
 FUND FEATURES HealthFund Amount $500 Individual $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance Percentage at
FUND FEATURES HealthFund Amount $500 Individual $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance Percentage at
Additional Information Provided by Aetna Life Insurance Company
 Additional Information Provided by Aetna Life Insurance Company Inquiry Procedure The plan of benefits described in the Booklet-Certificate is underwritten by: Aetna Life Insurance Company (Aetna) 151
Additional Information Provided by Aetna Life Insurance Company Inquiry Procedure The plan of benefits described in the Booklet-Certificate is underwritten by: Aetna Life Insurance Company (Aetna) 151
$6,350 Individual $12,700 Individual
 PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible $5,000 Individual $10,000 Individual $10,000 Family $20,000 Family All covered expenses accumulate separately toward the preferred or non-preferred Deductible.
PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible $5,000 Individual $10,000 Individual $10,000 Family $20,000 Family All covered expenses accumulate separately toward the preferred or non-preferred Deductible.
PREVENTIVE HEALTHCARE GUIDELINES INTRODUCTION
 PREVENTIVE HEALTHCARE GUIDELINES INTRODUCTION Health Plan of Nevada and Sierra Health and Life suggest that health plan members get certain screening tests, exams and shots to stay healthy. This document
PREVENTIVE HEALTHCARE GUIDELINES INTRODUCTION Health Plan of Nevada and Sierra Health and Life suggest that health plan members get certain screening tests, exams and shots to stay healthy. This document
1 exam every 12 months for members age 22 to age 65; 1 exam every 12 months for adults age 65 and older. Routine Well Child
 PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $1,000 Individual $1,000 Individual $2,000 Family $2,000 Family All covered expenses accumulate separately toward the preferred or
PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $1,000 Individual $1,000 Individual $2,000 Family $2,000 Family All covered expenses accumulate separately toward the preferred or
Cost Sharing Definitions
 SU Pro ( and ) Annual Deductible 1 Coinsurance Cost Sharing Definitions $200 per individual with a maximum of $400 for a family 5% of allowable amount for inpatient hospitalization - or - 50% of allowable
SU Pro ( and ) Annual Deductible 1 Coinsurance Cost Sharing Definitions $200 per individual with a maximum of $400 for a family 5% of allowable amount for inpatient hospitalization - or - 50% of allowable
Boehringer Ingelheim Benefit Information Sheet Plan Year 2016
 Boehringer Ingelheim Benefit Information Sheet Plan Year 2016 AETNA CHOICE POS II AETNA HEALTHFUND HRA AETNA HEALTHFUND HSA Contact and Further Information Internet Web Sites Overview Service Area If you
Boehringer Ingelheim Benefit Information Sheet Plan Year 2016 AETNA CHOICE POS II AETNA HEALTHFUND HRA AETNA HEALTHFUND HSA Contact and Further Information Internet Web Sites Overview Service Area If you
PDS Tech, Inc Proposed Effective Date: 01-01-2012 Aetna HealthFund Aetna Choice POS ll - ASC
 FUND FEATURES HealthFund Amount $500 Individual $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance 100% Percentage
FUND FEATURES HealthFund Amount $500 Individual $1,000 Employee + 1 Dependent $1,000 Employee + 2 Dependents $1,000 Family Amount contributed to the Fund by the employer Fund Coinsurance 100% Percentage
COVERAGE SCHEDULE. The following symbols are used to identify Maximum Benefit Levels, Limitations, and Exclusions:
 Exhibit D-3 HMO 1000 Coverage Schedule ROCKY MOUNTAIN HEALTH PLANS GOOD HEALTH HMO $1000 DEDUCTIBLE / 75 PLAN EVIDENCE OF COVERAGE LARGE GROUP Underwritten by Rocky Mountain Health Maintenance Organization,
Exhibit D-3 HMO 1000 Coverage Schedule ROCKY MOUNTAIN HEALTH PLANS GOOD HEALTH HMO $1000 DEDUCTIBLE / 75 PLAN EVIDENCE OF COVERAGE LARGE GROUP Underwritten by Rocky Mountain Health Maintenance Organization,
Preventive Services at 100%
 September 1, 2014 Update Preventive Care Services Covered Without Cost-sharing Without Copay, Coinsurance or Deductible The Affordable Care Act (ACA) requires non-grandfathered health plans and policies
September 1, 2014 Update Preventive Care Services Covered Without Cost-sharing Without Copay, Coinsurance or Deductible The Affordable Care Act (ACA) requires non-grandfathered health plans and policies
$100 Individual. Deductible
 PLAN FEATURES Deductible $100 Individual (per calendar year) $200 Family Unless otherwise indicated, the deductible must be met prior to benefits being payable. Member cost sharing for certain services,
PLAN FEATURES Deductible $100 Individual (per calendar year) $200 Family Unless otherwise indicated, the deductible must be met prior to benefits being payable. Member cost sharing for certain services,
PLAN DESIGN AND BENEFITS STANDARD HEALTH BENEFITS PLAN NJ HMO $30 PLAN (Also Marketed As: NJ SGB HMO $30/$300/D (5/10K) Plan)
 PLAN FEATURES Deductible (per calendar year) Plan Coinsurance Maximum Out-of-Pocket (per calendar year) $5,000 Individual $10,000 Family All covered expenses apply toward the Maximum Out-of-Pocket. Once
PLAN FEATURES Deductible (per calendar year) Plan Coinsurance Maximum Out-of-Pocket (per calendar year) $5,000 Individual $10,000 Family All covered expenses apply toward the Maximum Out-of-Pocket. Once
Sub Health Insurance Option Food Service - New Hire Memo
 MESQUITE ISD BENEFITS Sub Health Insurance Option Food Service - New Hire Memo Welcome to the Mesquite ISD family! If you are a new substitute, you must enroll in or decline medical coverage within 31
MESQUITE ISD BENEFITS Sub Health Insurance Option Food Service - New Hire Memo Welcome to the Mesquite ISD family! If you are a new substitute, you must enroll in or decline medical coverage within 31
Procedure Code(s): n/a This counseling service is included in a preventive care wellness examination or focused E&M visit.
 Coding Summary for Providers NOTE THE FOLLOWING: The purpose of this document is to provide a quick reference of the applicable codes for UnitedHealthcare plans that cover preventive care services in accordance
Coding Summary for Providers NOTE THE FOLLOWING: The purpose of this document is to provide a quick reference of the applicable codes for UnitedHealthcare plans that cover preventive care services in accordance
Rice University Effective Date: 07-01-2014 Aetna Choice POS ll - ASC PLAN DESIGN & BENEFITS ADMINISTERED BY AETNA LIFE INSURANCE COMPANY PLAN FEATURES
 PLAN DESIGN & BENEFITS PLAN FEATURES NON- Deductible (per calendar year) None Individual $1,000 Individual None Family $3,000 Family All covered expenses, excluding prescription drugs, accumulate toward
PLAN DESIGN & BENEFITS PLAN FEATURES NON- Deductible (per calendar year) None Individual $1,000 Individual None Family $3,000 Family All covered expenses, excluding prescription drugs, accumulate toward
Coverage for preventive care
 Coverage for preventive care Understanding your preventive care coverage Preventive care, like screenings and immunizations, helps you and your family stay healthier and can help lower your overall out-of-pocket
Coverage for preventive care Understanding your preventive care coverage Preventive care, like screenings and immunizations, helps you and your family stay healthier and can help lower your overall out-of-pocket
Member s responsibility (deductibles, copays, coinsurance and dollar maximums)
 MICHIGAN CATHOLIC CONFERENCE January 2015 Benefit Summary This is intended as an easy-to-read summary and provides only a general overview of your benefits. It is not a contract. Additional limitations
MICHIGAN CATHOLIC CONFERENCE January 2015 Benefit Summary This is intended as an easy-to-read summary and provides only a general overview of your benefits. It is not a contract. Additional limitations
Essentials Choice Rx 24 (HMO-POS) offered by PacificSource Medicare
 Essentials Choice Rx 24 (HMO-POS) offered by PacificSource Medicare Annual Notice of Changes for 2016 You are currently enrolled as a member of Essentials Choice Rx 24 (HMO-POS). Next year, there will
Essentials Choice Rx 24 (HMO-POS) offered by PacificSource Medicare Annual Notice of Changes for 2016 You are currently enrolled as a member of Essentials Choice Rx 24 (HMO-POS). Next year, there will
CA Group Business 2-50 Employees
 PLAN FEATURES Network Primary Care Physician Selection Deductible (per calendar year) Member Coinsurance Copay Maximum (per calendar year) Lifetime Maximum Referral Requirement PHYSICIAN SERVICES Primary
PLAN FEATURES Network Primary Care Physician Selection Deductible (per calendar year) Member Coinsurance Copay Maximum (per calendar year) Lifetime Maximum Referral Requirement PHYSICIAN SERVICES Primary
SPIN Effective Date: 01-01-2013 Aetna HealthFund Aetna Choice POS ll - ASC PLAN DESIGN & BENEFITS ADMINISTERED BY AETNA LIFE INSURANCE COMPANY
 HealthFund Amount $1,500 Employee $1,500 Employee + 1 Dependent $1,500 Employee + 2 Dependents $1,500 Family Amount contributed to Fund by employer Fund Coinsurance 100% Percentage at which Fund will reimburse
HealthFund Amount $1,500 Employee $1,500 Employee + 1 Dependent $1,500 Employee + 2 Dependents $1,500 Family Amount contributed to Fund by employer Fund Coinsurance 100% Percentage at which Fund will reimburse
Sherwin-Williams Medical, Prescription Drug and Dental Plans Plan Comparison Charts
 Sherwin-Williams Medical, Prescription Drug and Dental Plans Plan Comparison Charts You and Sherwin-Williams share the cost of certain benefits including medical and dental coverage and you have the opportunity
Sherwin-Williams Medical, Prescription Drug and Dental Plans Plan Comparison Charts You and Sherwin-Williams share the cost of certain benefits including medical and dental coverage and you have the opportunity
Essentials Choice Rx 25 (HMO-POS) offered by PacificSource Medicare
 Essentials Choice Rx 25 (HMO-POS) offered by PacificSource Medicare Annual Notice of Changes for 2016 You are currently enrolled as a member of Essentials Choice Rx 25 (HMO-POS). Next year, there will
Essentials Choice Rx 25 (HMO-POS) offered by PacificSource Medicare Annual Notice of Changes for 2016 You are currently enrolled as a member of Essentials Choice Rx 25 (HMO-POS). Next year, there will
Illinois Insurance Facts Illinois Department of Insurance
 Illinois Insurance Facts Illinois Department of Insurance Women s Health Care Issues Revised August 2012 Note: This information was developed to provide consumers with general information and guidance
Illinois Insurance Facts Illinois Department of Insurance Women s Health Care Issues Revised August 2012 Note: This information was developed to provide consumers with general information and guidance
IL Small Group MC Open Access Aetna Life Insurance Company Plan Effective Date: 10/01/2010 PLAN DESIGN AND BENEFITS- MC CDHP $2,500 90/70 (10/10)
 PLAN FEATURES Deductible (per calendar ) $2,500 Individual $5,000 Individual $7,500 Family $15,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered
PLAN FEATURES Deductible (per calendar ) $2,500 Individual $5,000 Individual $7,500 Family $15,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable. All covered
Aetna HealthFund Health Reimbursement Account Plan (Aetna HealthFund Open Access Managed Choice POS II )
 Health Fund The Health Fund amount reflected is on a per calendar year basis. If you do not use the entire fund by 12/31/2015, it will be moved into a Limited-Purpose Flexible Spending Account. Health
Health Fund The Health Fund amount reflected is on a per calendar year basis. If you do not use the entire fund by 12/31/2015, it will be moved into a Limited-Purpose Flexible Spending Account. Health
Group Insurance Plan of Benefits for New York University (Control # 620610) administered by Aetna International Effective Date: January 1, 2016
 Eligibility Provision Employee Regular full-time employees of New York University participating in this plan working a minimum of 25 hours per week. Dependent Wife or husband; same or opposite sex domestic
Eligibility Provision Employee Regular full-time employees of New York University participating in this plan working a minimum of 25 hours per week. Dependent Wife or husband; same or opposite sex domestic
CENTRAL MICHIGAN UNIVERSITY - Premier Plan (PPO1) 007000285-0002 0004 Effective Date: July 1, 2015 Benefits-at-a-Glance
 CENTRAL MICHIGAN UNIVERSITY - Premier Plan (PPO1) 007000285-0002 0004 Effective Date: July 1, 2015 Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only a general overview
CENTRAL MICHIGAN UNIVERSITY - Premier Plan (PPO1) 007000285-0002 0004 Effective Date: July 1, 2015 Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only a general overview
Summary of Benefits Community Advantage (HMO)
 Summary of Benefits Community Advantage (HMO) January 1, 2015 - December 31, 2015 This booklet gives you a summary of what we cover and what you pay. It doesn't list every service that we cover or list
Summary of Benefits Community Advantage (HMO) January 1, 2015 - December 31, 2015 This booklet gives you a summary of what we cover and what you pay. It doesn't list every service that we cover or list
Important health care reform notice Women s preventive services covered with no member cost share
 Quality health plans & benefits Healthier living Financial well-being Intelligent solutions Important health care reform notice Women s preventive services covered with no member cost share www.aetna.com
Quality health plans & benefits Healthier living Financial well-being Intelligent solutions Important health care reform notice Women s preventive services covered with no member cost share www.aetna.com
PPO Schedule of Payments (Maryland Large Group) Qualified High Deductible Health Plan National QA2000-20
 PPO Schedule of Payments (Maryland Large Group) Qualified High Health Plan National QA2000-20 Benefit Year Individual Family (Amounts for Participating and s services are separated in calculating when
PPO Schedule of Payments (Maryland Large Group) Qualified High Health Plan National QA2000-20 Benefit Year Individual Family (Amounts for Participating and s services are separated in calculating when
HBS PPO Enhanced Plan B1 Benefits-at-a-Glance Trinity Health
 HBS PPO Enhanced Plan B1 Benefits-at-a-Glance Trinity Health Deductible, Copays/Coinsurance and Dollar Maximums Deductible - per calendar year Tier 1 Tier 2 Tier 3 PPO In-Network Facility Trinity Health
HBS PPO Enhanced Plan B1 Benefits-at-a-Glance Trinity Health Deductible, Copays/Coinsurance and Dollar Maximums Deductible - per calendar year Tier 1 Tier 2 Tier 3 PPO In-Network Facility Trinity Health
January 1, 2015 December 31, 2015 Summary of Benefits. Altius Advantra (HMO) H8649-003 80.06.361.1-UTWY A
 January, 205 December 3, 205 Summary of Benefits H8649-003 80.06.36.-UTWY A Y0022_205_H8649_003_UT_WYa Accepted /204 Summary of Benefits January, 205 December 3, 205 This booklet gives you a summary of
January, 205 December 3, 205 Summary of Benefits H8649-003 80.06.36.-UTWY A Y0022_205_H8649_003_UT_WYa Accepted /204 Summary of Benefits January, 205 December 3, 205 This booklet gives you a summary of
IL Small Group PPO Aetna Life Insurance Company Plan Effective Date: 04/01/2009 PLAN DESIGN AND BENEFITS- PPO HSA HDHP $2,500 100/80 (04/09)
 PLAN FEATURES OUT-OF- Deductible (per calendar ) $2,500 Individual $5,000 Individual $5,000 Family $10,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
PLAN FEATURES OUT-OF- Deductible (per calendar ) $2,500 Individual $5,000 Individual $5,000 Family $10,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
University of Michigan Group: 007005187-0000, 0001 Comprehensive Major Medical (CMM) Benefits-at-a-Glance
 University of Michigan Group: 007005187-0000, 0001 Comprehensive Major Medical (CMM) Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only a general overview of your benefits.
University of Michigan Group: 007005187-0000, 0001 Comprehensive Major Medical (CMM) Benefits-at-a-Glance This is intended as an easy-to-read summary and provides only a general overview of your benefits.
THE MITRE CORPORATION PPO High Deductible Plan with a Health Saving Account (HSA)
 THE MITRE CORPORATION PPO High Deductible Plan with a Health Saving Account (HSA) Effective Date: 01-01-2016 PLAN FEATURES Annual Deductible $1,500 Employee $3,000 Employee $3,000 Employee + 1 Dependent
THE MITRE CORPORATION PPO High Deductible Plan with a Health Saving Account (HSA) Effective Date: 01-01-2016 PLAN FEATURES Annual Deductible $1,500 Employee $3,000 Employee $3,000 Employee + 1 Dependent
2013 Health Benefits Guide for HRA-Eligible Employees
 2013 Health Benefits Guide for HRA-Eligible Employees Revised: August 2013 Health Benefits Guide for HRA-Eligible Employees Table of Contents Important Phone Numbers... 5 Introduction... 6 Eligibility...
2013 Health Benefits Guide for HRA-Eligible Employees Revised: August 2013 Health Benefits Guide for HRA-Eligible Employees Table of Contents Important Phone Numbers... 5 Introduction... 6 Eligibility...
Active and Retiree Health Benefit Summary Plan Description And Plan Document 7670-00-411309/7670-03-411309
 Active and Retiree Health Benefit Summary Plan Description And Plan Document 7670-00-411309/7670-03-411309 BENEFITS ADMINISTERED BY Table of Contents INTRODUCTION... 1 PLAN INFORMATION... 2 BENEFIT CLASS
Active and Retiree Health Benefit Summary Plan Description And Plan Document 7670-00-411309/7670-03-411309 BENEFITS ADMINISTERED BY Table of Contents INTRODUCTION... 1 PLAN INFORMATION... 2 BENEFIT CLASS
$20 office visit copay; deductible 20%; after deductible. $30 office visit copay; deductible Not Covered. $30 office visit copay; deductible waived
 PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $300 Individual $600 Individual $600 Family $1,200 Family All covered expenses, accumulate separately toward the preferred or non-preferred
PLAN FEATURES IN-NETWORK OUT-OF-NETWORK Deductible (per calendar year) $300 Individual $600 Individual $600 Family $1,200 Family All covered expenses, accumulate separately toward the preferred or non-preferred
Hawaii Benchmarks Benefits under the Affordable Care Act (ACA)
 Hawaii Benchmarks Benefits under the Affordable Care Act (ACA) 10/2012 Coverage for Newborn and Foster Children Coverage Outside the Provider Network Adult Routine Physical Exams Well-Baby and Well-Child
Hawaii Benchmarks Benefits under the Affordable Care Act (ACA) 10/2012 Coverage for Newborn and Foster Children Coverage Outside the Provider Network Adult Routine Physical Exams Well-Baby and Well-Child
20% 40% Individual Family
 PLAN FEATURES NON-* Deductible (per calendar year) $2,500 Individual $3,000 Individual $5,000 Family $6,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
PLAN FEATURES NON-* Deductible (per calendar year) $2,500 Individual $3,000 Individual $5,000 Family $6,000 Family Unless otherwise indicated, the Deductible must be met prior to benefits being payable.
please refer to our internet site, www.harvardpilgrim.org, or contact the Member Services
 Schedule of s HPHC Insurance Company, Inc. THE HPHC INSURANCE COMPANY PPO PLAN MAINE ID: MD0000000750_F2 X This Schedule of s summarizes your benefits under The HPHC Insurance Company PPO Plan (the Plan)
Schedule of s HPHC Insurance Company, Inc. THE HPHC INSURANCE COMPANY PPO PLAN MAINE ID: MD0000000750_F2 X This Schedule of s summarizes your benefits under The HPHC Insurance Company PPO Plan (the Plan)
Independent Health s Medicare Passport Advantage (PPO)
 Independent Health s Medicare Passport Advantage (PPO) (a Medicare Advantage Preferred Provider Organization Option (PPO) offered by INDEPENDENT HEALTH BENEFITS CORPORATION with a Medicare contract) Summary
Independent Health s Medicare Passport Advantage (PPO) (a Medicare Advantage Preferred Provider Organization Option (PPO) offered by INDEPENDENT HEALTH BENEFITS CORPORATION with a Medicare contract) Summary
January 1, 2015 December 31, 2015 Summary of Benefits. Advantra (HMO) H3928-001 80.06.360.1-LA1
 January, 205 December 3, 205 Summary of Benefits H3928-00 80.06.360.-LA Y0022_205_H3928_00_LA Accepted 9/204 Summary of Benefits January, 205 December 3, 205 This booklet gives you a summary of what we
January, 205 December 3, 205 Summary of Benefits H3928-00 80.06.360.-LA Y0022_205_H3928_00_LA Accepted 9/204 Summary of Benefits January, 205 December 3, 205 This booklet gives you a summary of what we
2015 Medicare Advantage Summary of Benefits
 2015 Medicare Advantage Summary of Benefits HNE Medicare Premium No Rx and HNE Medicare Basic No Rx January 1, 2015 - December 31, 2015 H8578_2015_034 Accepted HNE MEDICARE ADVANTAGE ENROLLMENT KIT 2015
2015 Medicare Advantage Summary of Benefits HNE Medicare Premium No Rx and HNE Medicare Basic No Rx January 1, 2015 - December 31, 2015 H8578_2015_034 Accepted HNE MEDICARE ADVANTAGE ENROLLMENT KIT 2015
Greater Tompkins County Municipal Health Insurance Consortium
 WHO IS COVERED Requires both Medicare A & B enrollment. Type of Coverage Offered Single only Single only MEDICAL NECESSITY Pre-Certification Requirement None None Medical Benefit Management Program Not
WHO IS COVERED Requires both Medicare A & B enrollment. Type of Coverage Offered Single only Single only MEDICAL NECESSITY Pre-Certification Requirement None None Medical Benefit Management Program Not
[2015] SUMMARY OF BENEFITS H1189_2015SB
![[2015] SUMMARY OF BENEFITS H1189_2015SB [2015] SUMMARY OF BENEFITS H1189_2015SB](/thumbs/32/15705129.jpg) [2015] SUMMARY OF BENEFITS H1189_2015SB Section I You have choices in your health care One choice is to get your Medicare benefits through Original Medicare (fee-for-service Medicare). Original Medicare
[2015] SUMMARY OF BENEFITS H1189_2015SB Section I You have choices in your health care One choice is to get your Medicare benefits through Original Medicare (fee-for-service Medicare). Original Medicare
Benefit Summary - A, G, C, E, Y, J and M
 Benefit Summary - A, G, C, E, Y, J and M Benefit Year: Calendar Year Payment for Services Deductible Individual $600 $1,200 Family (Embedded*) $1,200 $2,400 Coinsurance (the percentage amount the Covered
Benefit Summary - A, G, C, E, Y, J and M Benefit Year: Calendar Year Payment for Services Deductible Individual $600 $1,200 Family (Embedded*) $1,200 $2,400 Coinsurance (the percentage amount the Covered
Reliability and predictable costs for individuals and families
 INDIVIDUAL & FAMILY PLANS HEALTH NET HMO PLANS Reliability and predictable costs for individuals and families If you re looking for a health plan that s simple to use and easy to understand, you ve found
INDIVIDUAL & FAMILY PLANS HEALTH NET HMO PLANS Reliability and predictable costs for individuals and families If you re looking for a health plan that s simple to use and easy to understand, you ve found
Commercial. Individual & Family Plan. Health Net California Farm Bureau and PPO. Insurance Plans. Outline of Coverage and Exclusions and Limitations
 Commercial Individual & Family Plan Health Net California Farm Bureau and PPO Insurance Plans Outline of Coverage and Exclusions and Limitations Table of Contents Health Plans Outline of coverage 1 Read
Commercial Individual & Family Plan Health Net California Farm Bureau and PPO Insurance Plans Outline of Coverage and Exclusions and Limitations Table of Contents Health Plans Outline of coverage 1 Read
